Poster Session C
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (1776–1795) Spondyloarthritis Including Psoriatic Arthritis – Basic Science Poster
1776: Macrophage Migration Inhibitory Factor May Help Maintain Tight Junctions in the Gut by Enhancing Occludin Expression
Tuesday, November 14, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- SF
Shaghayegh Foroozan, MSc (she/her/hers)
University Health Network/University of Toronto
Toronto, ON, CanadaDisclosure information not submitted.
Abstract Poster Presenter(s)
Shaghayegh Foroozan1 and Nigil Haroon2, 1University Health Network/University of Toronto, Toronto, ON, Canada, 2University of Toronto, University Health Network, Schroeder Arthritis Institute, Department of Medicine/Rheumatology, Toronto, ON, Canada
Background/Purpose: Axial Spondyloarthritis (AxSpA) is a chronic inflammatory disease with multifactorial origins, primarily affecting the musculoskeletal system. Gut inflammation is seen in the majority of AxSpA patients, with 60% having microscopic changes and 10% with overt Inflammatory Bowel Disease (IBD). Over the years many pathways and cell populations have been linked to the pathogenesis of gut inflammation in AxSpA. Macrophage migration inhibitory factor (MIF) plays a critical role in the pathogenesis of AxSpA. Over-expression of MIF in a mouse model of SpA (SKG mice) causes major clinical features of AxSpA while blocking or depletion of MIF significantly suppresses these symptoms. However, the role of MIF in gut inflammation in AxSpA is unknown. We hypothesized that MIF is a key player driving gut inflammation in AxSPA.
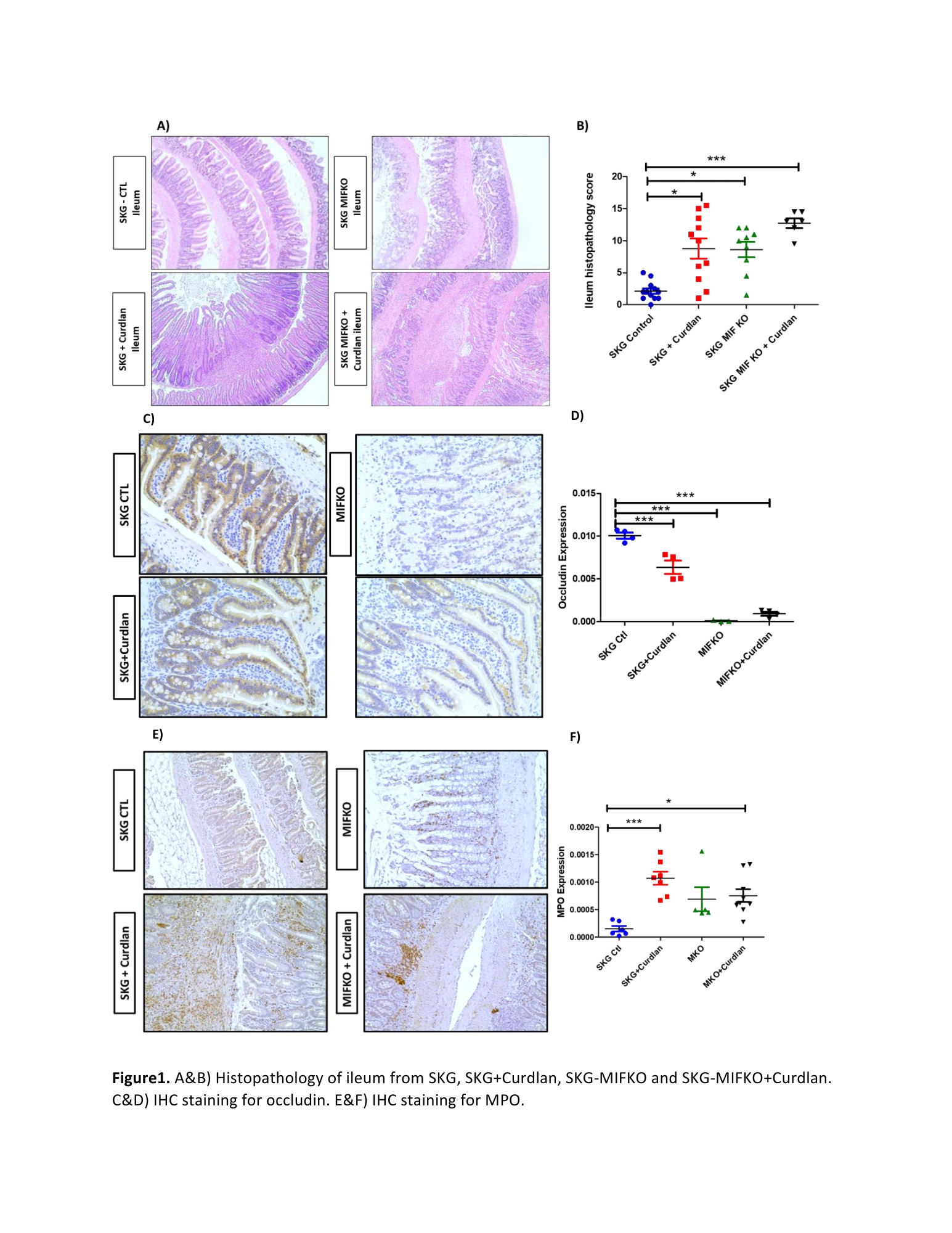
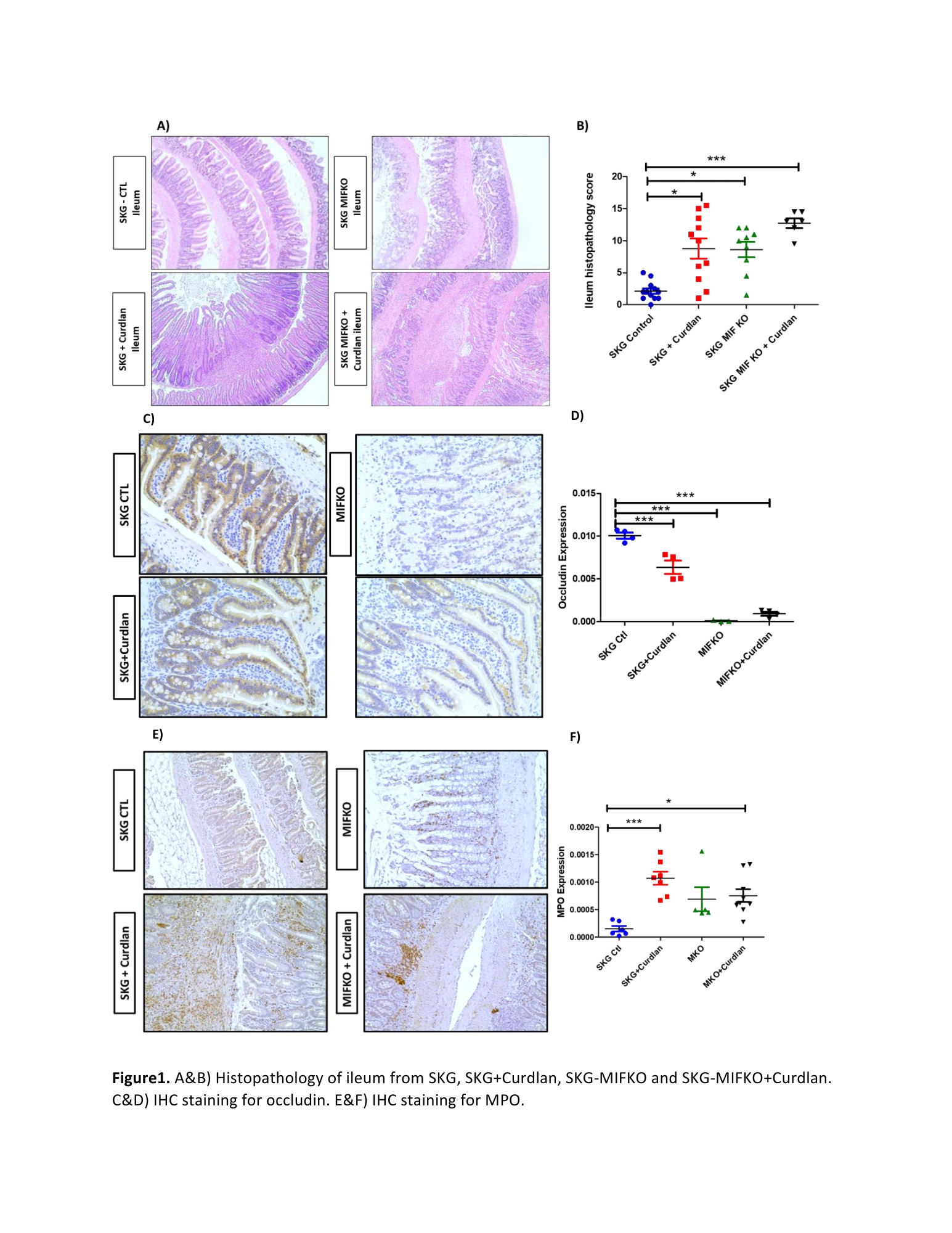
To study the effect of MIF on gut homeostasis and inflammation in the SKG mouse model of spondyloarthritis
Methods: A total of 12 SKG control mice, 11 SKG mice treated with curdlan, 9 SKG-MIF Knock Out (KO), and 6 SKG-MIFKO mice treated with curdlan that were all 16 weeks old were used for this study. H&E slides were prepared for histopathology assessment on formalin-fixed paraffin-embedded (FFPE) blocks of ileum tissue (2 individuals scored the samples independently and were blinded to the group). Immunohistochemistry (IHC) was performed for occludin and MPO antibody was used to assess neutrophil (a major source of MIF) infiltration. Kruskal–Wallis test was used to analyze the difference between the 4 groups.
Results: We observed significantly increased inflammation levels in the ileum of SKG+curdlan mice compared to SKG control mice (Fig1a). SKG-MIFKO+curdlan mice did not have a significant benefit of reduction in inflammation levels. Interestingly, even without curdlan treatment, MIFKO mice showed inflammation in the gut. SKG-MIFKO mice (with and without curdlan) developed a disruption of ileal epithelium. There was a significant reduction in occludin expression compared to SKG control mice, suggesting a disruption of tight junctions (Fig1b). MPO expression was significantly elevated in SKG+curdlan and SKG-MIFKO+curdlan groups. However, although not significant, it seems that the MPO expression is lower in the SKG-MIFKO+curdlan compared to SKG+curdlan mice.
Conclusion: Knocking out MIF in SKG mice has shown improvement in AxSpA symptoms. However, based on our findings, MIF seems to have a protective role in the gut of SKG mice unlike what we see in joints. The absence of MIF leads to decreased expression of occludin. These findings together suggest that MIF is essential for the integrity of the gut epithelial barrier in the SKG mouse model of SpA. If this effect on the tight junction is directly related to MIF or through changes in type 3 immune response needs to be investigated.
S. Foroozan: None; N. Haroon: AbbVie, 2, Eli Lilly, 2, Janssen, 2, Novartis, 2, UCB Pharma, 2.
Background/Purpose: Axial Spondyloarthritis (AxSpA) is a chronic inflammatory disease with multifactorial origins, primarily affecting the musculoskeletal system. Gut inflammation is seen in the majority of AxSpA patients, with 60% having microscopic changes and 10% with overt Inflammatory Bowel Disease (IBD). Over the years many pathways and cell populations have been linked to the pathogenesis of gut inflammation in AxSpA. Macrophage migration inhibitory factor (MIF) plays a critical role in the pathogenesis of AxSpA. Over-expression of MIF in a mouse model of SpA (SKG mice) causes major clinical features of AxSpA while blocking or depletion of MIF significantly suppresses these symptoms. However, the role of MIF in gut inflammation in AxSpA is unknown. We hypothesized that MIF is a key player driving gut inflammation in AxSPA.
To study the effect of MIF on gut homeostasis and inflammation in the SKG mouse model of spondyloarthritis
Methods: A total of 12 SKG control mice, 11 SKG mice treated with curdlan, 9 SKG-MIF Knock Out (KO), and 6 SKG-MIFKO mice treated with curdlan that were all 16 weeks old were used for this study. H&E slides were prepared for histopathology assessment on formalin-fixed paraffin-embedded (FFPE) blocks of ileum tissue (2 individuals scored the samples independently and were blinded to the group). Immunohistochemistry (IHC) was performed for occludin and MPO antibody was used to assess neutrophil (a major source of MIF) infiltration. Kruskal–Wallis test was used to analyze the difference between the 4 groups.
Results: We observed significantly increased inflammation levels in the ileum of SKG+curdlan mice compared to SKG control mice (Fig1a). SKG-MIFKO+curdlan mice did not have a significant benefit of reduction in inflammation levels. Interestingly, even without curdlan treatment, MIFKO mice showed inflammation in the gut. SKG-MIFKO mice (with and without curdlan) developed a disruption of ileal epithelium. There was a significant reduction in occludin expression compared to SKG control mice, suggesting a disruption of tight junctions (Fig1b). MPO expression was significantly elevated in SKG+curdlan and SKG-MIFKO+curdlan groups. However, although not significant, it seems that the MPO expression is lower in the SKG-MIFKO+curdlan compared to SKG+curdlan mice.
Conclusion: Knocking out MIF in SKG mice has shown improvement in AxSpA symptoms. However, based on our findings, MIF seems to have a protective role in the gut of SKG mice unlike what we see in joints. The absence of MIF leads to decreased expression of occludin. These findings together suggest that MIF is essential for the integrity of the gut epithelial barrier in the SKG mouse model of SpA. If this effect on the tight junction is directly related to MIF or through changes in type 3 immune response needs to be investigated.
S. Foroozan: None; N. Haroon: AbbVie, 2, Eli Lilly, 2, Janssen, 2, Novartis, 2, UCB Pharma, 2.



