Poster Session C
Professional development and education
Session: (2061–2088) Professional Education Poster
2061: Evaluation of a Tool to Enhance Training of the Physical Examination of the Temporomandibular Joint (TM Joint) in Juvenile Idiopathic Arthritis (JIA)
Tuesday, November 14, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- TR
Tova Ronis, MD
Children's National Hospital
Washington, DC, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Tova Ronis1, Nancy Pan2, Rebecca Sadun3, Melissa Lerman4, Cory Resnick5, James Bost6, Peter Stoustrup7, Marinka Twilt8 and for the CARRA TMJ Arthritis Workgroup9, 1Children's National Hospital, Chevy Chase, MD, 2Hospital for Special Surgery, New York, NY, 3Duke University, Durham, NC, 4Children's Hospital of Philadelphia, Philadelphia, PA, 5Harvard Medical School, Boston, MA, 6Children's Health Center, Children's National Medical Center, Washington, DC, 7Aarhus University, Aarhus, Denmark, 8Alberta Children's Hospital, Calgary, AB, Canada, 9Childhood Arthritis and Rheumatology Research Alliance, Washington, DC
Background/Purpose: Arthritis of the TM joint is a frequent finding in patients with JIA, potentially leading to dentofacial deformities, pain, and lower quality of life.1 Orofacial examination enables early detection of TM joint involvement.2 The TM Joint Juvenile Arthritis Work Group published a standardized physical exam (article) to assess for JIA-induced orofacial manifestations.2 Training programs do not routinely teach a standardized TM joint exam. The aim of the study was to demonstrate the effectiveness of a novel e-learning module in teaching the physical exam of the TM joint in JIA.
Methods: A 20-minute e-learning module consisting of instructive videos and interactive questions was created. Pediatric rheumatology fellows participated in a study to assess the module. Block randomization was performed, and fellows were stratified by post-graduate year. One group received the article while the second group received both the article and access to the e-learning module. All participants completed a written pre-test before the learning intervention andthen underwent both: an in-person objective structured clinical examination (OSCE)during the Childhood Arthritis and Rheumatology Research Alliance Scientific Meeting inMarch 2023; and a written post-test. The maximum OSCE score was 18. Crosstab tables and Chi-squared tests were used to assess categorical variables across groups. For continuous measures when comparing the two groups, Wilcoxon Rank Sum tests were used due to the small sample size.
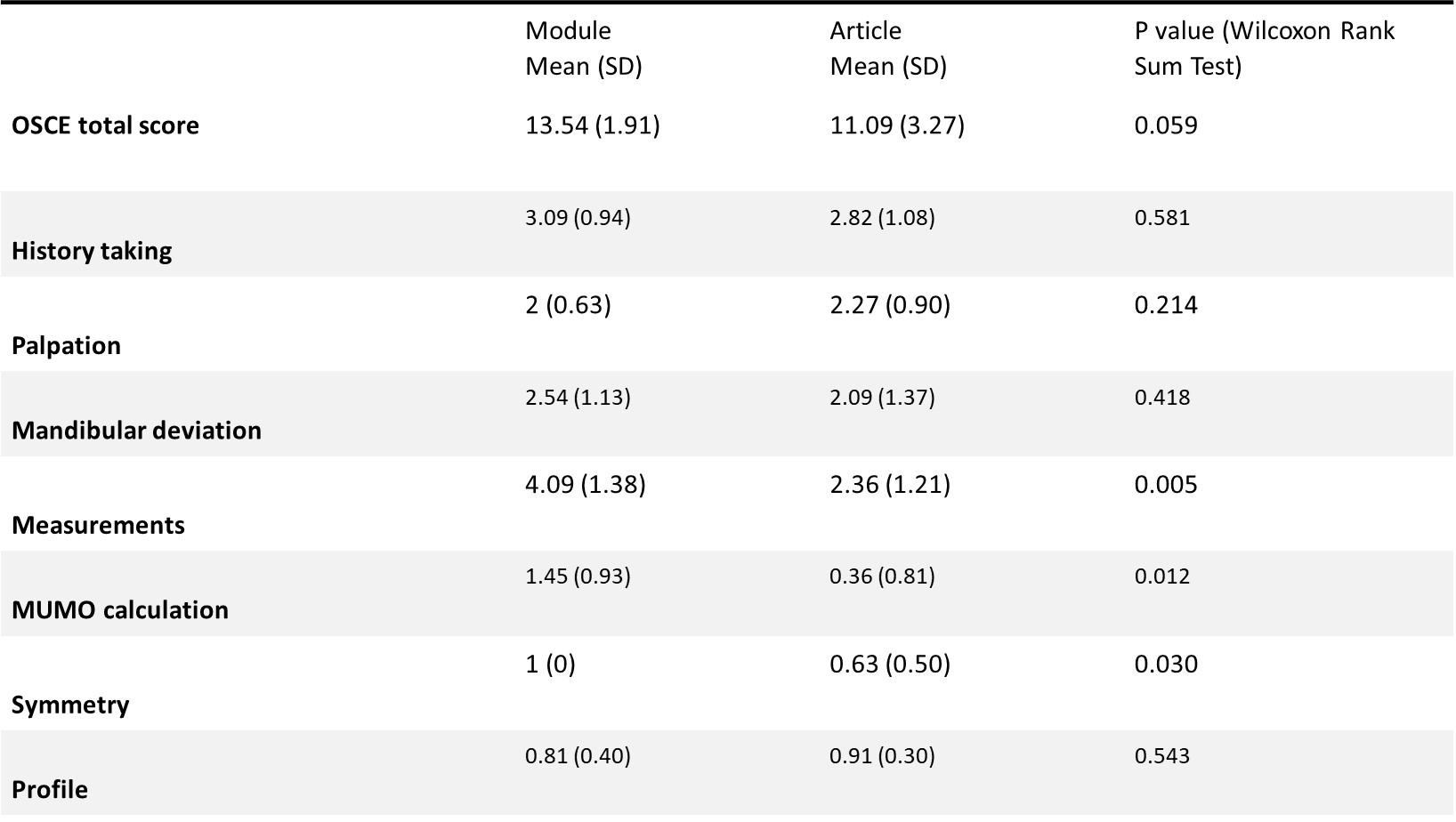
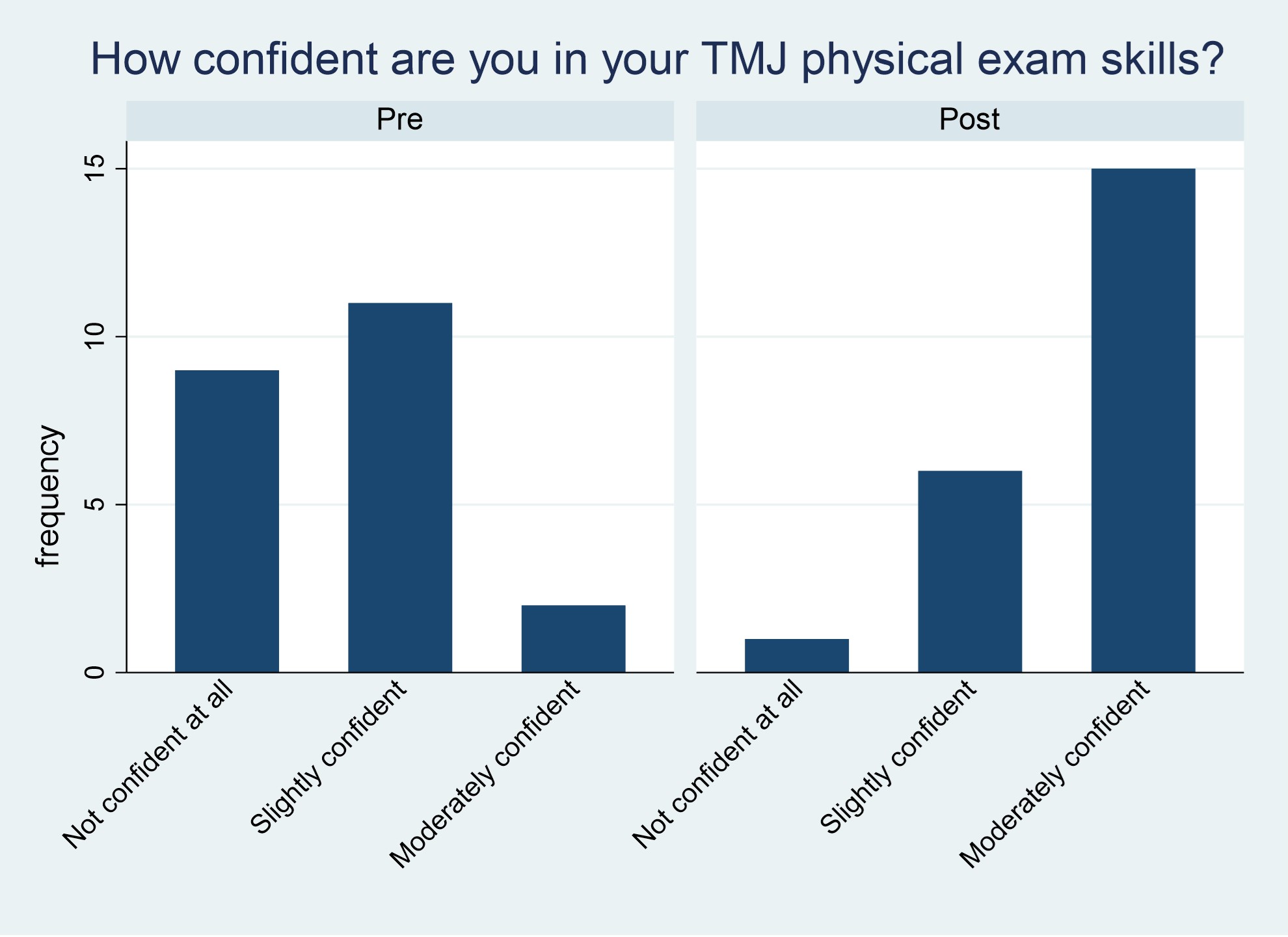
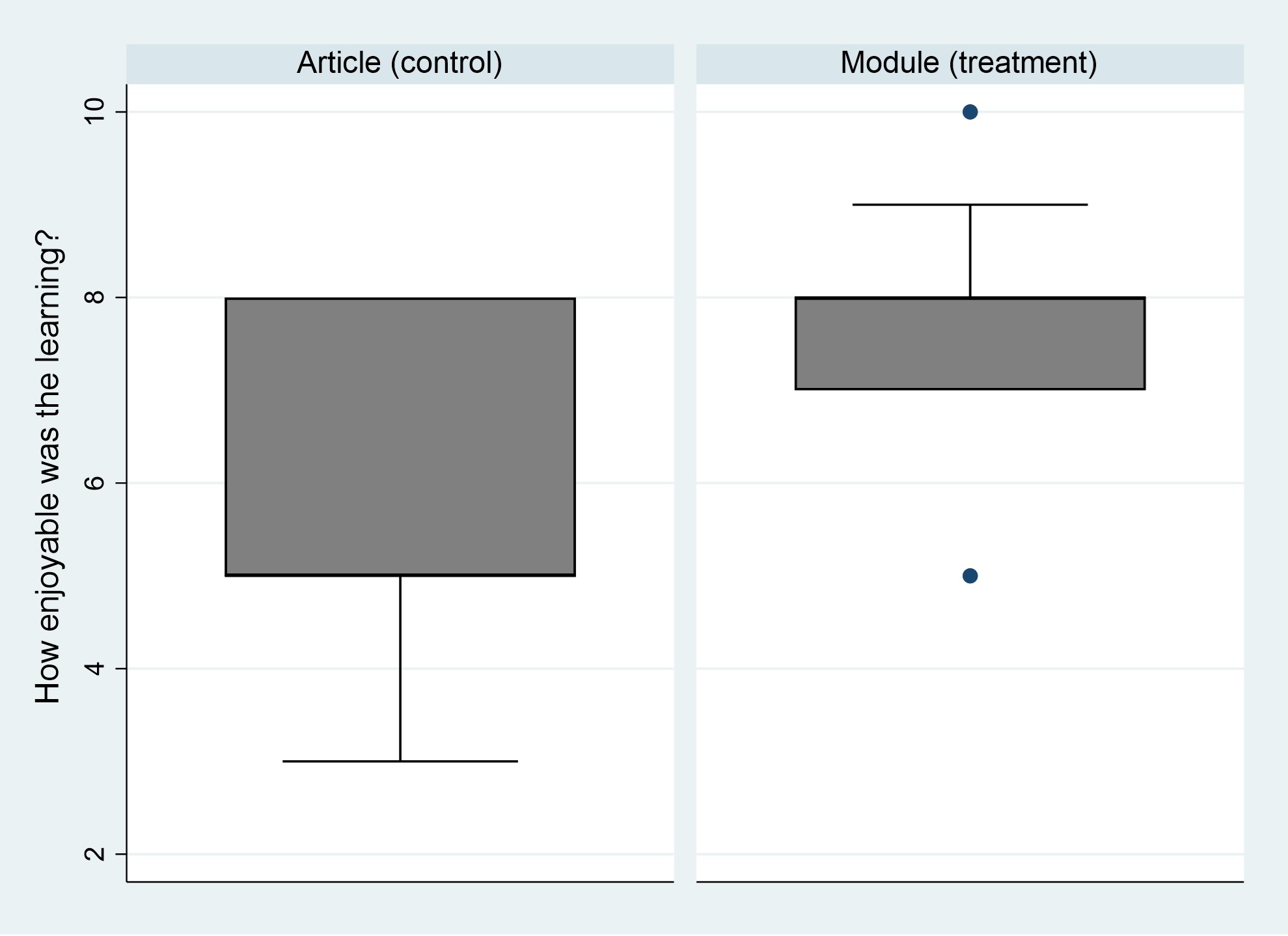
Results: Twenty-two pediatric rheumatology fellows enrolled, with 11 in each group. Both reported an equal amount of time spent preparing for the OSCE (mean 34.8 mins). Written test: The two groups performed equally. There was a trend toward significance in defining maximal incisal opening (MIO) on the written test in the module group. Both groups had a trend towards improvement in recognition of patient profiles and facial asymmetry. OSCE: The mean OSCE score was 11.1 (SD 3.3) in the article group and 13.5 (SD 1.9) in the module group, with a trend towards significance (p=0.059). Significant differences were seen on the OSCE in learning domains related to measuring MIO, calculating maximal unassisted mouth opening (MUMO), and assessment of facial symmetry. There were no differences in other domains (see Table 1). Confidence in TM joint exam skills was increased in all fellows after the intervention with no difference between groups (Figure 1). Enjoyment scores in the module group were higher than in the article group (mean 7.7/10 vs 5.9/10, p=0.017) (Figure 2).
Conclusion: This study demonstrated effectiveness of a novel e-learning module in teaching the physical exam of the TM joint in JIA. Learners who viewed the module were more adept at obtaining quantitative TM joint measurements than those who read the article. Both groups showed improvement in overall skill and confidence level, although the module group enjoyed the learning experience more.
References:
1.Stoll ML et al. TM joint arthritis in JIA, now what? Pediatr Rheumatol. 2018;16(1):32.
2.Stoustrup P et al. Standardizing the clinical orofacial examination in JIA: An interdisciplinary, consensus-based, short screening protocol. J Rheumatol. 2020:47(9):1397
T. Ronis: None; N. Pan: None; R. Sadun: None; M. Lerman: None; C. Resnick: AbbVie/Abbott, 2; J. Bost: None; P. Stoustrup: None; M. Twilt: None; f. the CARRA TMJ Arthritis Workgroup: None.
Background/Purpose: Arthritis of the TM joint is a frequent finding in patients with JIA, potentially leading to dentofacial deformities, pain, and lower quality of life.1 Orofacial examination enables early detection of TM joint involvement.2 The TM Joint Juvenile Arthritis Work Group published a standardized physical exam (article) to assess for JIA-induced orofacial manifestations.2 Training programs do not routinely teach a standardized TM joint exam. The aim of the study was to demonstrate the effectiveness of a novel e-learning module in teaching the physical exam of the TM joint in JIA.
Methods: A 20-minute e-learning module consisting of instructive videos and interactive questions was created. Pediatric rheumatology fellows participated in a study to assess the module. Block randomization was performed, and fellows were stratified by post-graduate year. One group received the article while the second group received both the article and access to the e-learning module. All participants completed a written pre-test before the learning intervention andthen underwent both: an in-person objective structured clinical examination (OSCE)during the Childhood Arthritis and Rheumatology Research Alliance Scientific Meeting inMarch 2023; and a written post-test. The maximum OSCE score was 18. Crosstab tables and Chi-squared tests were used to assess categorical variables across groups. For continuous measures when comparing the two groups, Wilcoxon Rank Sum tests were used due to the small sample size.
Results: Twenty-two pediatric rheumatology fellows enrolled, with 11 in each group. Both reported an equal amount of time spent preparing for the OSCE (mean 34.8 mins). Written test: The two groups performed equally. There was a trend toward significance in defining maximal incisal opening (MIO) on the written test in the module group. Both groups had a trend towards improvement in recognition of patient profiles and facial asymmetry. OSCE: The mean OSCE score was 11.1 (SD 3.3) in the article group and 13.5 (SD 1.9) in the module group, with a trend towards significance (p=0.059). Significant differences were seen on the OSCE in learning domains related to measuring MIO, calculating maximal unassisted mouth opening (MUMO), and assessment of facial symmetry. There were no differences in other domains (see Table 1). Confidence in TM joint exam skills was increased in all fellows after the intervention with no difference between groups (Figure 1). Enjoyment scores in the module group were higher than in the article group (mean 7.7/10 vs 5.9/10, p=0.017) (Figure 2).
Conclusion: This study demonstrated effectiveness of a novel e-learning module in teaching the physical exam of the TM joint in JIA. Learners who viewed the module were more adept at obtaining quantitative TM joint measurements than those who read the article. Both groups showed improvement in overall skill and confidence level, although the module group enjoyed the learning experience more.
References:
1.Stoll ML et al. TM joint arthritis in JIA, now what? Pediatr Rheumatol. 2018;16(1):32.
2.Stoustrup P et al. Standardizing the clinical orofacial examination in JIA: An interdisciplinary, consensus-based, short screening protocol. J Rheumatol. 2020:47(9):1397
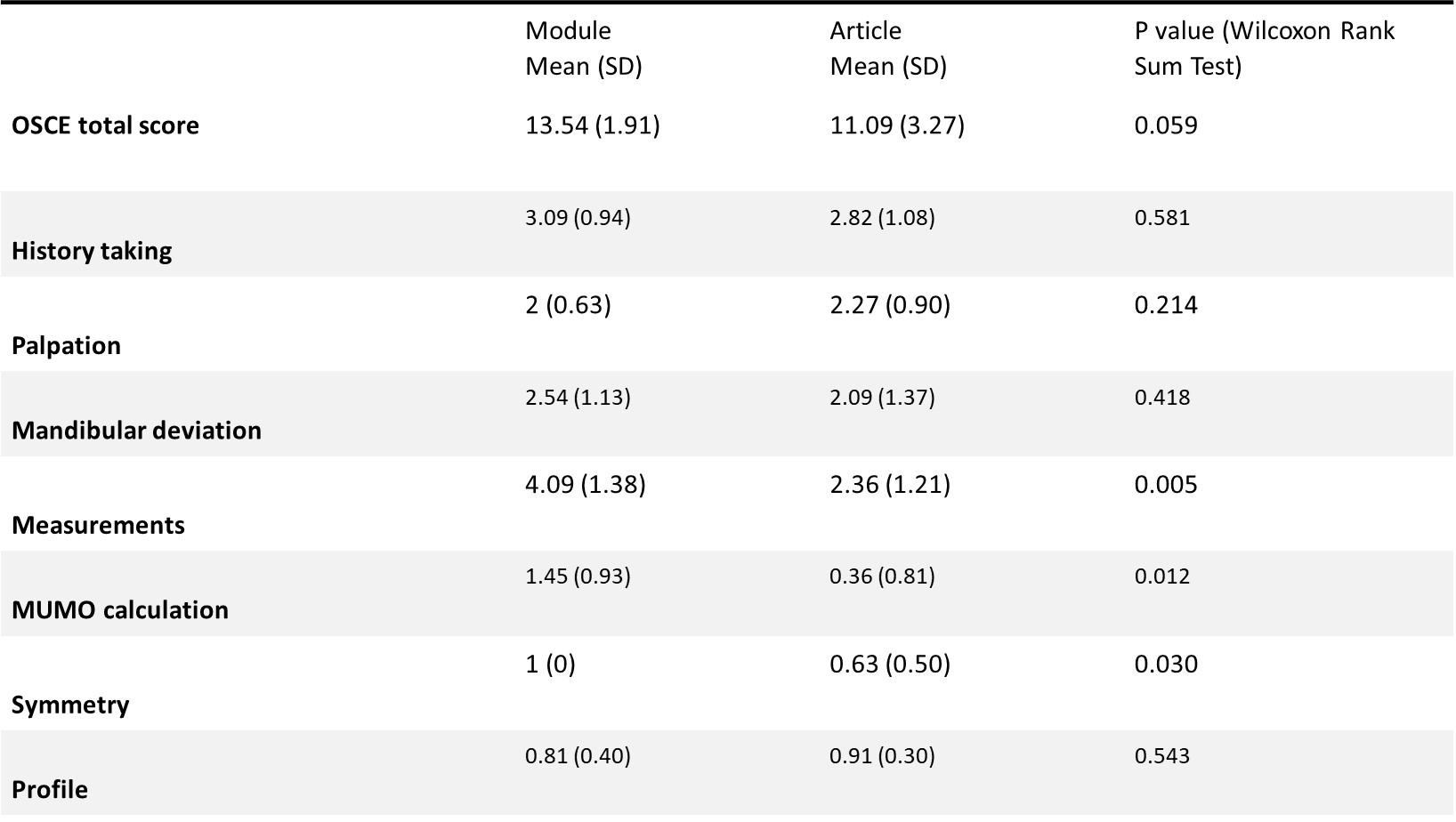
Table 1. OSCE scores by learning group. OSCE: objective structured clinical examination, MUMO: maximal unassisted mouth opening.
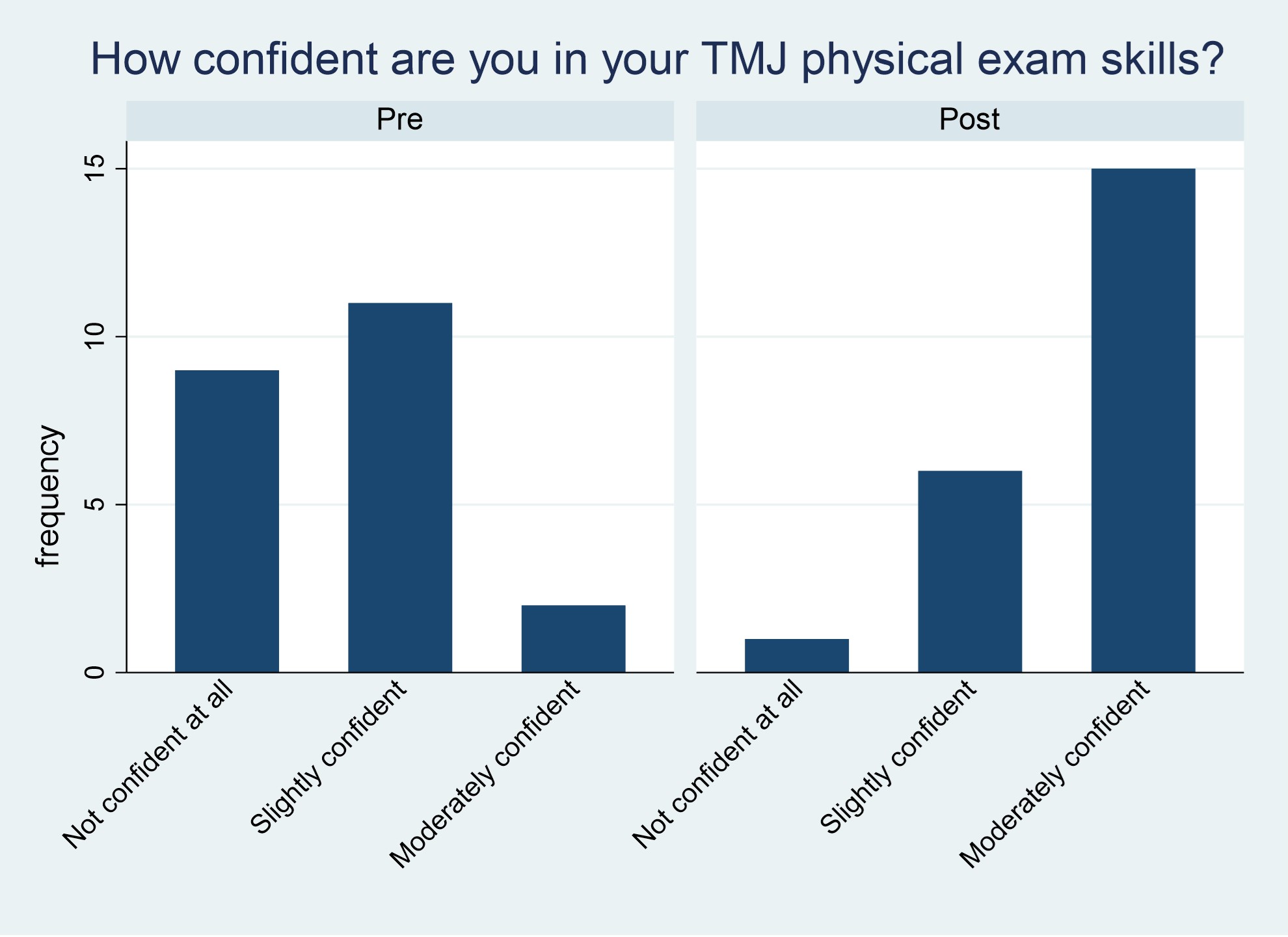
Figure 1. Self-reported confidence in TM Joint physical exam skills before and after the learning intervention for all participants. No difference was noted between groups.
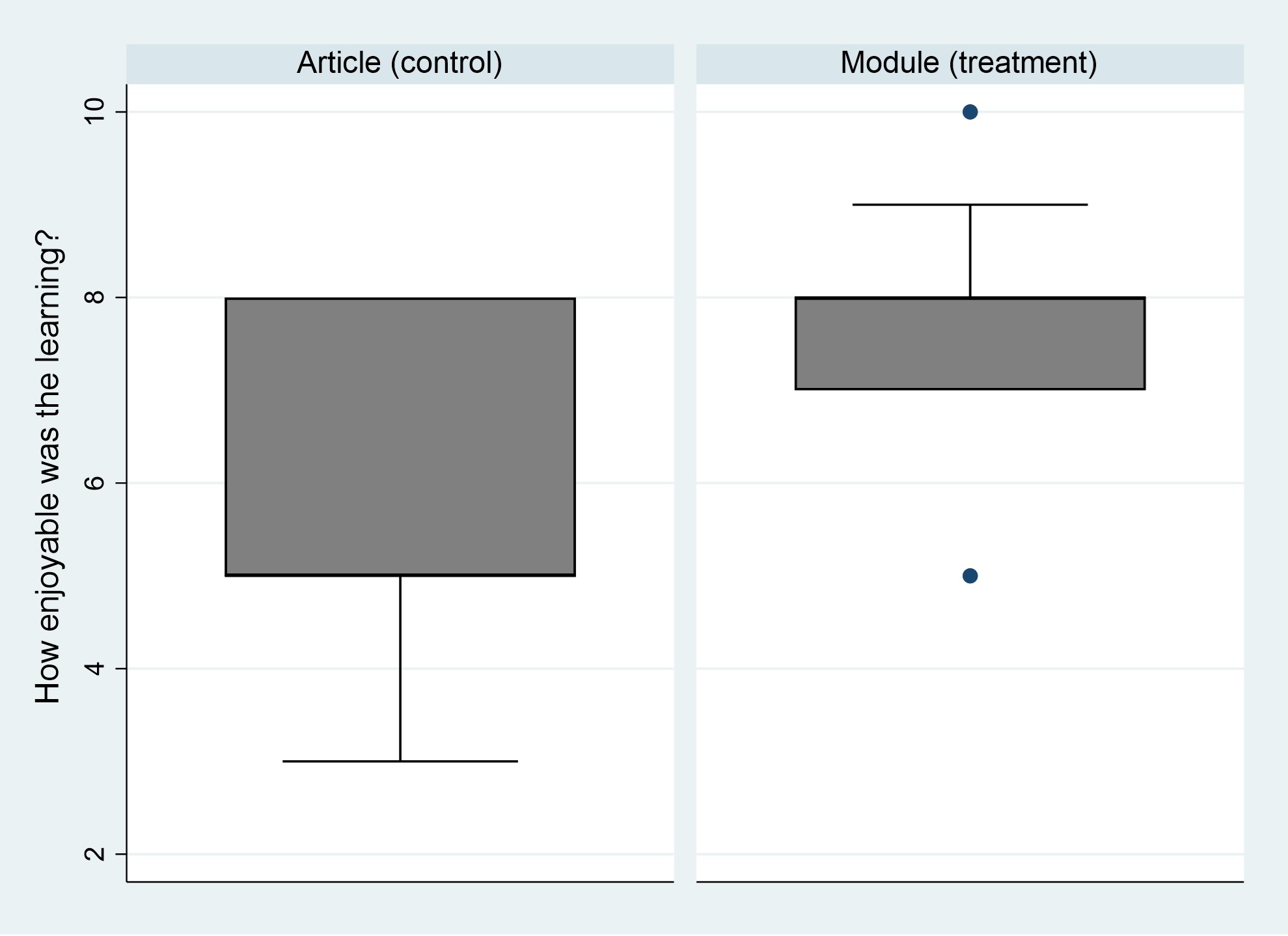
Figure 2. Participant response to “How enjoyable was the learning?”
T. Ronis: None; N. Pan: None; R. Sadun: None; M. Lerman: None; C. Resnick: AbbVie/Abbott, 2; J. Bost: None; P. Stoustrup: None; M. Twilt: None; f. the CARRA TMJ Arthritis Workgroup: None.



