Poster Session C
Systemic lupus erythematosus (SLE)
Session: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
2319: Changes in the Causes and Predictors of Lupus Mortality in Spain Through the Last Decades: Data from the RELESSER Registry
Tuesday, November 14, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- JC
Jaime Calvo Alén, MD, PhD
Hospital Universitario Araba
Vitoria, SpainDisclosure information not submitted.
Abstract Poster Presenter(s)
Clara Moriano Morales1, Jaime Calvo- Alén2, Iñigo Rúa-Figueroa3, MARIA ELVIRA DIEZ ALVAREZ1, Cristina Bermúdez4, JULIA MARTINEZ BARRIO5, Maria Galindo-Izquierdo6, Alejandro Olivé-Marqués7, Eva Tomero Muriel8, Antonio Fernandez-Nebro9, Mercedes Freire González10, Olaia Fernandez-Berrizbeitia11, Ana Pérez Gómez12, Esther Uriarte Isacelaya13, carlos Marras Fernández-Cid14, Carlos Montilla-Morales15, Gregorio Santos Soler16, Ricardo Blanco17, Manuel Rodríguez-Gómez18, PALOMA VELA19, Alina Boteanu20, Javier Narvaez21, Victor Martinez-Taboada22, Blanca Hernández-Cruz23, Jose Luis Andreu-Sánchez24, José Ángel Hernández Beriain25, Lorena Expósito26, Raúl Menor-Almagro27, Mónica Ibáñez-Barceló28, Ivan Castellvi29, Carles Galisteo30, Enrique Raya31, Víctor Quevedo-Vila32, Tomás Vazquez-Rodriguez33, jesús Ibáñez34 and Jose-Maria Pego-Reigosa35, 1Rheumatology, Hospital Universitario de León, León, Spain, 2Rheumatology, Bioaraba Research Unit, Hospital Universitario Araba, Vitoria, Spain, 3Rheumatology, Hospital de Gran Canaria Doctor Negrin, Las Palmas de Gran Canaria, Spain, 4Bioaraba Research Unit, Vitoria, Spain, 5Rheumatology, Gregorio Marañon University Hospital, Madrid, Spain, 6Rheumatology, University Hospital of 12 de Octubre, Madrid, Spain, 7Rheumatology, Private Practice, Barcelona, Spain, 8Rheumatology, Hospital La Princesa, Madrid, Spain, 9Hospital Regional Universitario de Málaga, Malaga, Spain, 10Rheumatology department, Complexo Hospitalario Universitario A Coruña (CHUAC). Instituto de Investigación Biomédica A Coruña (INIBIC), A Coruña, Spain, 11Spanish Health Care Service, Bilbao, Spain, 12Rheumatology, Hospital Principe de Asturias, Alcalá de Henares, Spain, 13Rheumatology, University Hospital of Donosti, San Sebastián, Spain, 14Rheumatology, Hospital Virgen Arrixaca, Murcia, Spain, 15Rheumatology, University Hospital of Salamanca, Salamanca, Spain, 16Rheumatology, Hospital Marina Baixa Villajoyosa, Alicante, Spain, 17Hospital Universitario Marqués de Valdecilla, IDIVAL, Santander, Spain, 18Rheumatology, Hospital Ourense, Ourense, Spain, 19Rheumatology, Hospital General Universitario Alicante, Alicante, Spain, 20Hospital Universitario Ramón y Cajal, Departamento de Reumatología, Madrid, Spain, 21Hospital Universitario de Bellvitge, Barcelona, Spain, 22Rheumatology, Hospital Marqués de Valdecilla, Santander, Spain, 23Rheumatology, Hospital Virgen de la Macarena, Sevilla, Spain, 24Rheumatology, Hospital Universitario Puerta de Hierro, Majadahonda, Spain, 25Rheumatology, Hospital Insular de Gran Canaria, Las Palmas de Gran Canaria, Spain, 26Rheumatology, Hospital de Canarias, Tenerife, Spain, 27Rheumatology, Hospital Jerez, Puerto De Santa María, Spain, 28Rheumatology, Hospital Universitari Son Llàtzer, Palma de Mallorca, Spain, 29Rheumatology, Hospital Universitari de la Santa Creu i Sant Pau, Sant Just Desvern, Spain, 30Hospital Universitario Parc Taulí, Sabadell, Spain, 31Rheumatology, Hospital San Cecilio, Granada, Spain, 32Rheumatology, Hospital Monforte de Lemos, Lugo, Spain, 33Rheumatology, Complejo Hospitalario Universitario de Ferrol, A Coruña, Spain, 34Rheumatology, Hospital Ribera Povisa, Vigo, Spain, 35Rheumatology, Hospital do Meixoeiro, Vigo, Spain
Background/Purpose: The mortality in Systemic Lupus Erythematosus (SLE) varies largely across different countries most probably due to social, healthcare and ethnic differences. We need to identify demographic, clinical and serological predictors of mortality in SLE in our country, to improve the prognosis of SLE patients.
Objectives: To analyze the causes and identify predictive factors of mortality of SLE, and to assess the time evolution and chronological changes in Spain.
Methods: We performed a cross-sectional and retrospective study analyzing data from RELESSER cohort. Sociodemographic, clinical and serological variables, comorbidities and treatments, as well as indicators of disease activity, damage and severity were recorded. We excluded patients with lost information about the death variable and analyzed the differential features of deceased patients in comparisons with survivors through different time stages according to the date of diagnosis: until the 1980's; the 1990's and the first decade of the 21st century. Variables associated with mortality in univariate analysis were entered into different multivariate models to determine which ones were independently associated with the outcome of the disease in each decade.
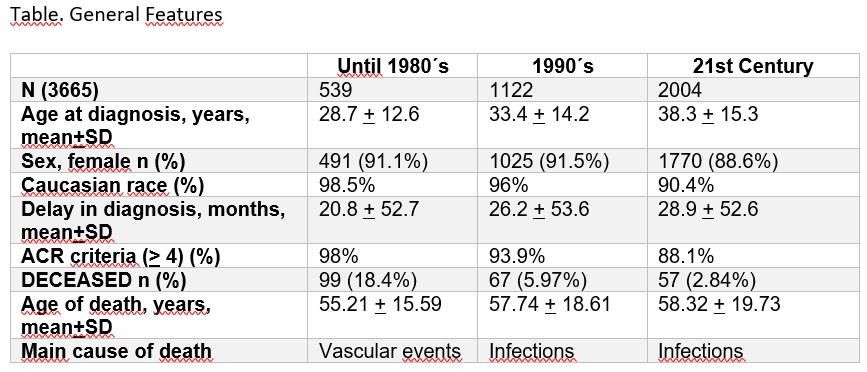
Results: A total of 3665 patients were included, mostly caucasian female with similar general features regardless of the different time stages analyzed.18.4% until the 1980´s, the 5.97% in the 1990´s and up to 2.84% of the individuals in first decade of the 21st century, had died. The main age of death was similar in the different groups, around 55-58 years old (Table). The vascular events were the leading cause of death until the 1980´s, while in the last two decades, were infections.
The older age at diagnosis was predictor of mortality. Neither gender nor delay in diagnosis was independently associated with mortality, with the exception of the female sex, which behaved as a protective factor until the 1980´s.
The mortality predictors in our cohort were the presence of hypocomplementemia and organ damage until the 1980´s; thrombocytopenia, antiphospholipid syndrome and valve disease in the 1990´s; serositis, organ damage and depression in the first decade of the 21st century. Conversely, skin involvement was related to greater survival over the last two decades and comorbidities were associated with mortality in all periods of the study. The use of high doses of corticosteroids was predictor of mortality in each time stage, as well as the use of cyclophosphamide and rituximab from the year 2000. Antimalarial treatment was linked to improved survival in all the decades analyzed.
Conclusion: In the RELESSER cohort, the main cause of death in the last decades were infections. However, until the 1980´s, vascular events were predominant. Older age at diagnosis, use of corticosteroids and comorbidities were associated with significant increase in mortality in SLE, while antimalarial treatment was linked to improved survival. Data indicate that organ damage is a risk factor and skin involvement is a protective factor against mortality. Differentially, female sex until the 1980´s was independently associated with improved survival, and depression at the beginning of the 21st century was linked to mortality.
C. Moriano Morales: None; J. Calvo- Alén: AbbVie, 2, AstraZeneca, 2, Biogen, 6, BMS, 5, Galapagos, 6, GSK, 2, 6, Lilly, 2, 6, Novartis, 2, 6, Roche, 5, Sanofi, 2; I. Rúa-Figueroa: AstraZeneca, 5, GSK, 1, 6; M. DIEZ ALVAREZ: None; C. Bermúdez: None; J. MARTINEZ BARRIO: None; M. Galindo-Izquierdo: None; A. Olivé-Marqués: None; E. Tomero Muriel: None; A. Fernandez-Nebro: None; M. Freire González: None; O. Fernandez-Berrizbeitia: None; A. Pérez Gómez: None; E. Uriarte Isacelaya: None; c. Marras Fernández-Cid: None; C. Montilla-Morales: None; G. Santos Soler: None; R. Blanco: AbbVie, 5, 6, Amgen, 6, AstraZeneca, 2, BMS, 6, Eli Lilly, 6, Galapagos, 2, 6, Janssen, 2, 6, MSD, 6, Novartis, 2, 6, Pfizer, 2, 6, Roche, 5, 6, Sanofi, 6; M. Rodríguez-Gómez: None; P. VELA: AbbVie/Abbott, 5, AstraZeneca, 5, Eli Lilly, 5, 6, GlaxoSmithKlein(GSK), 6, Novartis, 5, Pfizer, 5; A. Boteanu: GSK, 5, 6; J. Narvaez: None; V. Martinez-Taboada: None; B. Hernández-Cruz: None; J. Andreu-Sánchez: None; J. Hernández Beriain: None; L. Expósito: None; R. Menor-Almagro: None; M. Ibáñez-Barceló: None; I. Castellvi: None; C. Galisteo: None; E. Raya: None; V. Quevedo-Vila: None; T. Vazquez-Rodriguez: None; j. Ibáñez: None; J. Pego-Reigosa: None.
Background/Purpose: The mortality in Systemic Lupus Erythematosus (SLE) varies largely across different countries most probably due to social, healthcare and ethnic differences. We need to identify demographic, clinical and serological predictors of mortality in SLE in our country, to improve the prognosis of SLE patients.
Objectives: To analyze the causes and identify predictive factors of mortality of SLE, and to assess the time evolution and chronological changes in Spain.
Methods: We performed a cross-sectional and retrospective study analyzing data from RELESSER cohort. Sociodemographic, clinical and serological variables, comorbidities and treatments, as well as indicators of disease activity, damage and severity were recorded. We excluded patients with lost information about the death variable and analyzed the differential features of deceased patients in comparisons with survivors through different time stages according to the date of diagnosis: until the 1980's; the 1990's and the first decade of the 21st century. Variables associated with mortality in univariate analysis were entered into different multivariate models to determine which ones were independently associated with the outcome of the disease in each decade.
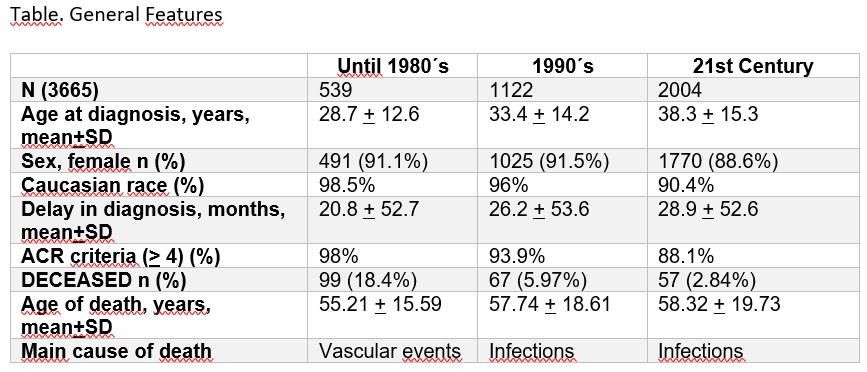
Results: A total of 3665 patients were included, mostly caucasian female with similar general features regardless of the different time stages analyzed.18.4% until the 1980´s, the 5.97% in the 1990´s and up to 2.84% of the individuals in first decade of the 21st century, had died. The main age of death was similar in the different groups, around 55-58 years old (Table). The vascular events were the leading cause of death until the 1980´s, while in the last two decades, were infections.
The older age at diagnosis was predictor of mortality. Neither gender nor delay in diagnosis was independently associated with mortality, with the exception of the female sex, which behaved as a protective factor until the 1980´s.
The mortality predictors in our cohort were the presence of hypocomplementemia and organ damage until the 1980´s; thrombocytopenia, antiphospholipid syndrome and valve disease in the 1990´s; serositis, organ damage and depression in the first decade of the 21st century. Conversely, skin involvement was related to greater survival over the last two decades and comorbidities were associated with mortality in all periods of the study. The use of high doses of corticosteroids was predictor of mortality in each time stage, as well as the use of cyclophosphamide and rituximab from the year 2000. Antimalarial treatment was linked to improved survival in all the decades analyzed.
Conclusion: In the RELESSER cohort, the main cause of death in the last decades were infections. However, until the 1980´s, vascular events were predominant. Older age at diagnosis, use of corticosteroids and comorbidities were associated with significant increase in mortality in SLE, while antimalarial treatment was linked to improved survival. Data indicate that organ damage is a risk factor and skin involvement is a protective factor against mortality. Differentially, female sex until the 1980´s was independently associated with improved survival, and depression at the beginning of the 21st century was linked to mortality.
C. Moriano Morales: None; J. Calvo- Alén: AbbVie, 2, AstraZeneca, 2, Biogen, 6, BMS, 5, Galapagos, 6, GSK, 2, 6, Lilly, 2, 6, Novartis, 2, 6, Roche, 5, Sanofi, 2; I. Rúa-Figueroa: AstraZeneca, 5, GSK, 1, 6; M. DIEZ ALVAREZ: None; C. Bermúdez: None; J. MARTINEZ BARRIO: None; M. Galindo-Izquierdo: None; A. Olivé-Marqués: None; E. Tomero Muriel: None; A. Fernandez-Nebro: None; M. Freire González: None; O. Fernandez-Berrizbeitia: None; A. Pérez Gómez: None; E. Uriarte Isacelaya: None; c. Marras Fernández-Cid: None; C. Montilla-Morales: None; G. Santos Soler: None; R. Blanco: AbbVie, 5, 6, Amgen, 6, AstraZeneca, 2, BMS, 6, Eli Lilly, 6, Galapagos, 2, 6, Janssen, 2, 6, MSD, 6, Novartis, 2, 6, Pfizer, 2, 6, Roche, 5, 6, Sanofi, 6; M. Rodríguez-Gómez: None; P. VELA: AbbVie/Abbott, 5, AstraZeneca, 5, Eli Lilly, 5, 6, GlaxoSmithKlein(GSK), 6, Novartis, 5, Pfizer, 5; A. Boteanu: GSK, 5, 6; J. Narvaez: None; V. Martinez-Taboada: None; B. Hernández-Cruz: None; J. Andreu-Sánchez: None; J. Hernández Beriain: None; L. Expósito: None; R. Menor-Almagro: None; M. Ibáñez-Barceló: None; I. Castellvi: None; C. Galisteo: None; E. Raya: None; V. Quevedo-Vila: None; T. Vazquez-Rodriguez: None; j. Ibáñez: None; J. Pego-Reigosa: None.



