Poster Session C
Vasculitis
Session: (2387–2424) Vasculitis – Non-ANCA-Associated & Related Disorders Poster III
2405: Role of Mitochondria in Activation of Platelets in Giant Cell Arteritis
Tuesday, November 14, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- DM
Despina Michailidou, MD (she/her/hers)
University of Oklahoma and VA Medical Center
Oklahoma, OK, United StatesDisclosure(s): Chemocentryx: Advisor or Review Panel Member (Terminated, September 29, 2021)
Abstract Poster Presenter(s)
Despoina Michailidou1, Peter Grayson2, Payton Hermanson1, Jorge Armando Gonzalez-Chapa1, David Cuthbertson3, Nader A. Khalidi4, Curry Koening5, Carol Langford6, Carol McAlear7, Larry Moreland8, Christian Pagnoux9, Philip Seo10, Antoine G Sreih11, Kenneth Warrington12, Paul Monach13, Peter Merkel7 and Christian Lood1, 1University of Washington, Seattle, WA, 2National Institutes of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), National Institutes of Health (NIH), Chevy Chase, MD, 3University of South Florida, Tampa, FL, 4McMaster University, Hamilton, ON, Canada, 5University of Texas Dell Medical School, Austin, TX, 6Cleveland Clinic, Cleveland, OH, 7University of Pennsylvania, Philadelphia, PA, 8University of Colorado, Denver, CO, 9Mount Sinai Hospital, Toronto, ON, Canada, 10Johns Hopkins University, Baltimore, MD, 11Bristol Myers Squibb, Princeton Pike, NJ, 12Mayo Clinic, Rochester, MN, 13VA Boston Healthcare System, Boston, MA
Background/Purpose: We recently found extracellular mitochondrial-derived N-formyl methionine in patients with giant cell arteritis (GCA. Extracellular mitochondria can be extruded by several mechanisms, including platelet activation, and are highly immunogenic, leading to formation of anti-mitochondrial antibodies (AMAs), such as anti-cardiolipin antibodies that have also been observed in GCA. The purpose of this study was to determine the presence of additional AMAs, including anti-mitofusin 1 (MFN1) antibodies, in patients with GCA. We also sought to determine whether extracellular mitochondria are capable of mediating platelet activation in patients with GCA.
Methods: Anti-MFN1 IgG levels were measured using an in-house ELISA in the plasma from patients with GCA (n=65 in remission, n=14 with active disease), and 30 healthy controls (HC). Ultrapure mitochondria, isolated from HepG2 cells, were incubated with plasma from 65 patients with GCA in remission, and 16 HC, and assessed for IgA and IgG binding to the mitochondrial outer membrane using flow cytometry. Mitochondria were also opsonized with patient (n=58) or healthy control (n=10) plasma (6%), and subsequently incubated with platelets to determine the capacity of plasma factors, including AMAs, to promote mitochondrial-mediated platelet activation.
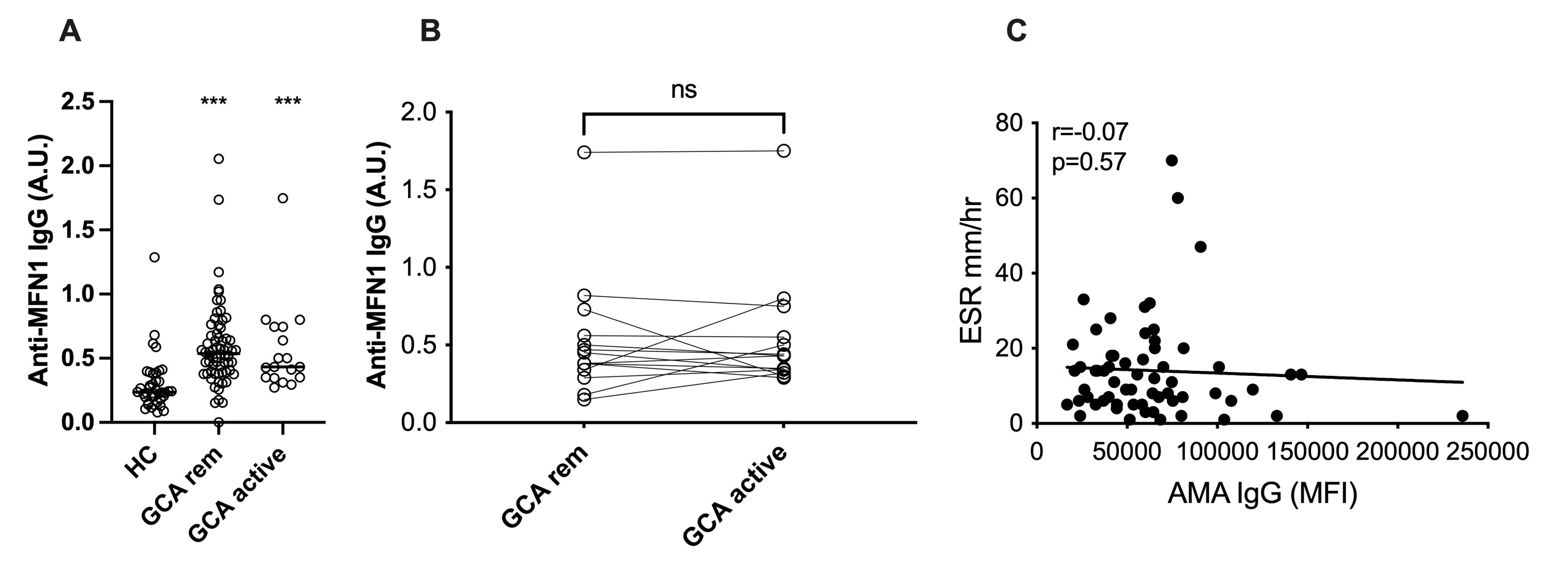
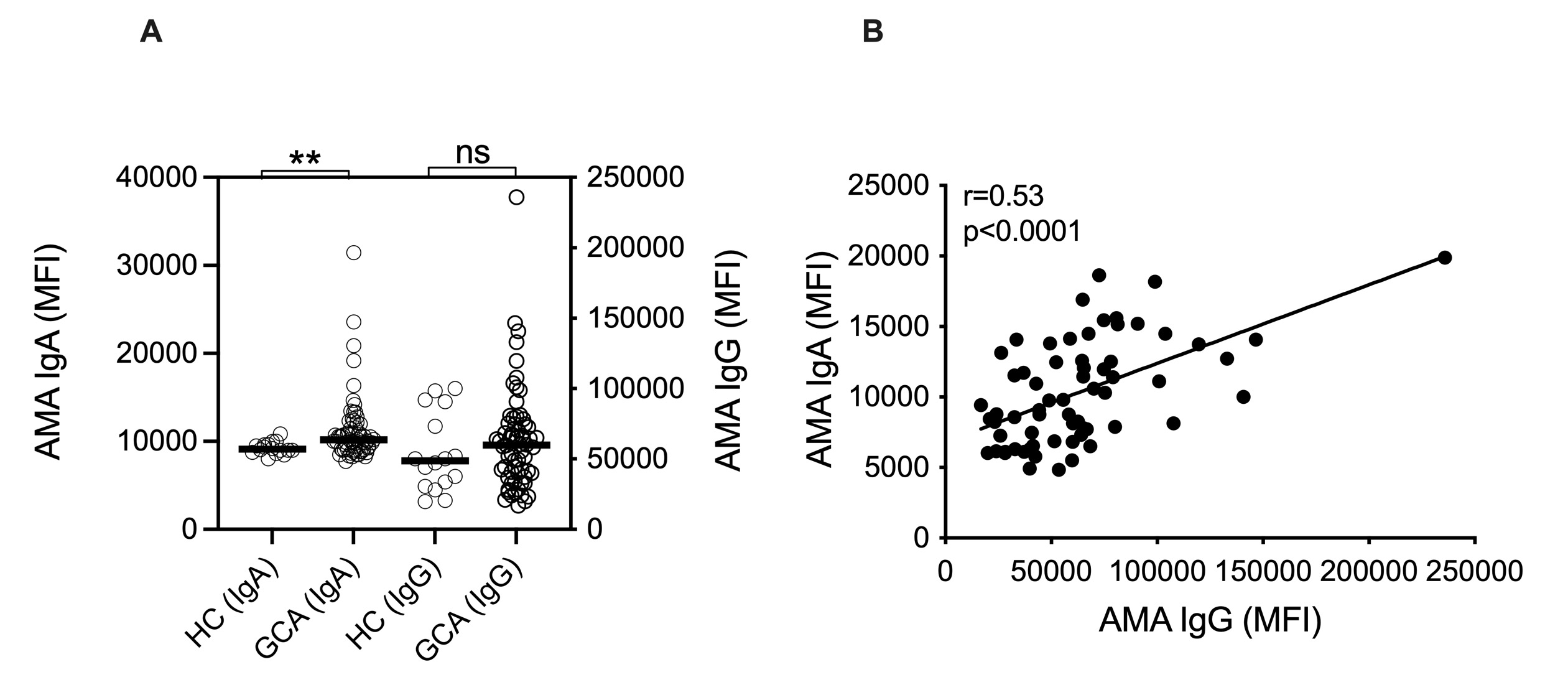
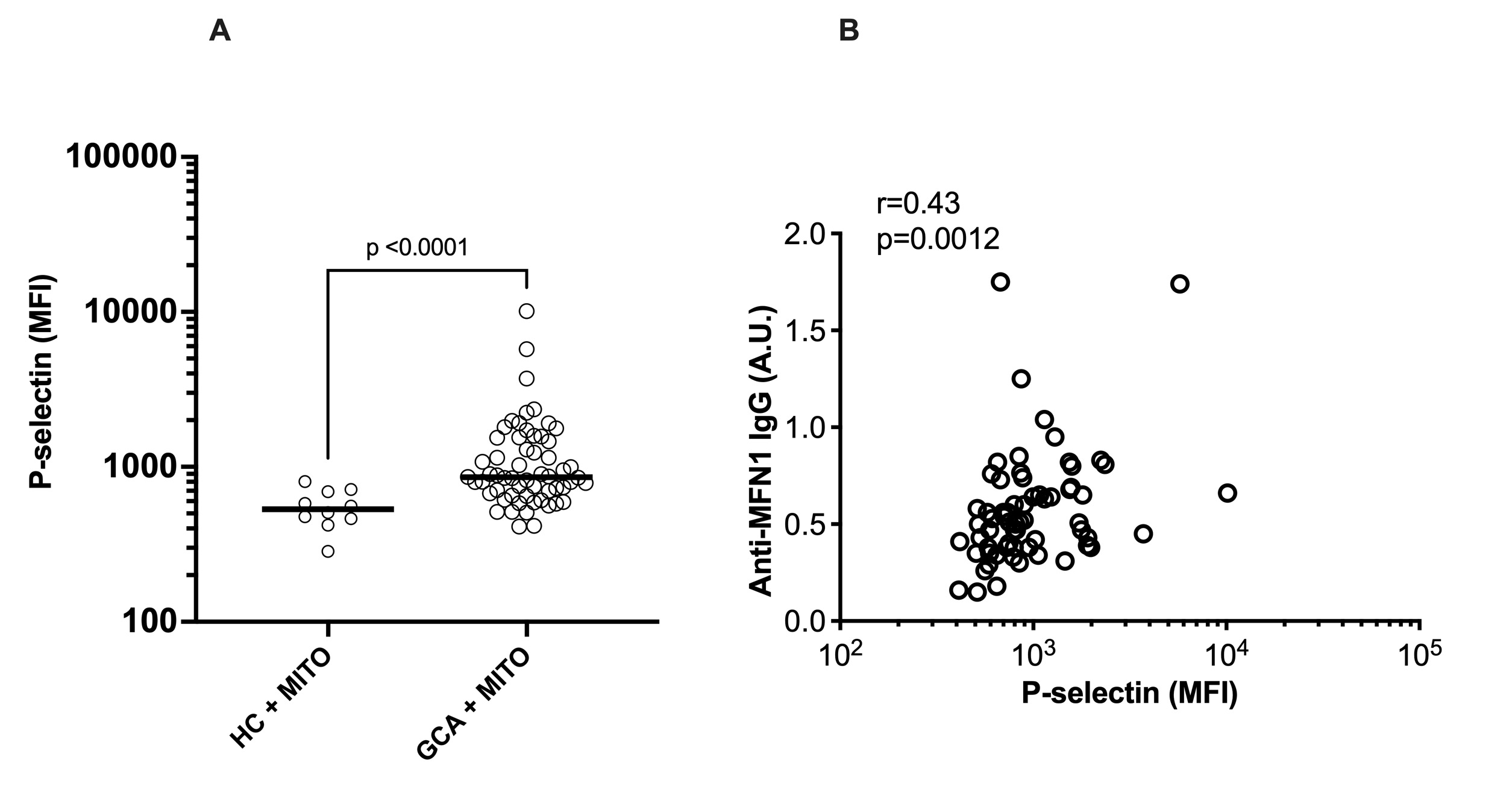
Results: Levels of anti-MFN1 IgG antibodies, a specific AMA, were elevated both in active disease (p< 0.0001) and in remission (p< 0.0001) in patients with GCA (Figure 1A). No differences in levels of anti-MFN1 antibodies were found between patients in remission and active disease for GCA (Figure 1B).No association was observed between anti-MFN1 antibodies and ESR levels (Figure 1C). Though total levels of IgG AMA did not reach statistical significance (p=0.38) in GCA patients compared to HC, IgA AMA levels were significantly higher in patients with GCA as compared to healthy individuals (p=0.003, Figure 2A). Levels of IgA AMA correlated with levels of IgG AMA in patients with GCA (Figure 2B), but not with levels of anti-MFN1 (data not shown). Finally, to investigate a potential pathogenic role of AMAs in GCA, exogenous mitochondria, derived from HepG2 cells, were opsonized with patient plasma and, upon washing, incubated with platelets from healthy individual. Plasma from patients with GCA had enhanced capacity to promote mitochondrial-mediated platelet activation as measured by P-selectin expression on platelet cell surface by flow cytometry, as compared to plasma from HC (p< 0.0001, Figure 3A). Platelet levels of P-selectin were associated with levels of anti-MFN1 IgG in patients with GCA (r=0.43, p=0.0012, Figure 3B).
Conclusion: We report the presence of AMAs in GCA. Presence of autoantibodies targeting mitochondria supports the hypothesis of antigenic mitochondrial components being present in GCA. Our data suggest that mitochondrial targeting by AMAs results in immune complex formation, potently activating platelets, possibly partaking in the thromboembolic morbidity and mortality of the disease. Targeting key drivers of mitochondrial extrusion in GCA could lead to new therapeutic interventions, including suppression of platelet activation.
D. Michailidou: Chemocentryx, 1; P. Grayson: None; P. Hermanson: None; J. Armando Gonzalez-Chapa: None; D. Cuthbertson: None; N. Khalidi: AbbVie/Abbott, 5, Bristol-Myers Squibb(BMS), 5, GlaxoSmithKlein(GSK), 1, Otsuka, 1, 6, Roche, 1, 6; C. Koening: Amgen, 1; C. Langford: AbbVie, 12, Non-paid consultant, AstraZeneca, 5, 12, Non-paid consultant, Bristol-Myers Squibb(BMS), 5, 12, Non-paid consultant, GlaxoSmithKlein(GSK), 5; C. McAlear: None; L. Moreland: Boehringer-Ingelheim, 12, member of independent Data Safety Monitoring Board, Celltrion, 12, member of independent Data Safety Monitoring Board; C. Pagnoux: AstraZeneca, 1, 2, 6, GlaxoSmithKlein(GSK), 1, 6, Otsuka, 1, 2, 5, 6, Pfizer, 5, Roche, 2; P. Seo: Amgen, 1, Janssen, 1; A. Sreih: Bristol Myers Squibb, 3; K. Warrington: Bristol-Myers Squibb(BMS), 5, Chemocentryx, 1, 6, Eli Lilly, 5, kiniksa, 5; P. Monach: Genentech, 12, Lecture with honorarium, HI-Bio, 2; P. Merkel: AbbVie/Abbott, 5, Amgen, 2, 5, ArGenx, 2, AstraZeneca, 2, 5, Boehringer-Ingelheim, 2, 5, Bristol-Myers Squibb(BMS), 2, 5, Cabaletta, 2, CSL Behring, 2, Eicos, 5, Electra, 5, Genentech, 5, GlaxoSmithKlein(GSK), 2, 5, HiBio, 2, InflaRx, 2, 5, Janssen, 2, Jubilant, 2, Kyverna, 2, 11, MiroBio, 2, Neutrolis, 5, Novartis, 2, NS Pharma, 2, Q32, 2, Regeneron, 2, Sanofi, 2, Sparrow, 2, Takeda, 2, 5, UpToDate, 9, Visterra, 2; C. Lood: Amytryx, 5, Boehringer-Ingelheim, 5, Bristol-Myers Squibb(BMS), 5, Citryll, 2, Eli Lilly, 5, Gilead, 5, Horizon Therapeutics, 5, Pfizer, 5, Redd Pharma, 5, 11.
Background/Purpose: We recently found extracellular mitochondrial-derived N-formyl methionine in patients with giant cell arteritis (GCA. Extracellular mitochondria can be extruded by several mechanisms, including platelet activation, and are highly immunogenic, leading to formation of anti-mitochondrial antibodies (AMAs), such as anti-cardiolipin antibodies that have also been observed in GCA. The purpose of this study was to determine the presence of additional AMAs, including anti-mitofusin 1 (MFN1) antibodies, in patients with GCA. We also sought to determine whether extracellular mitochondria are capable of mediating platelet activation in patients with GCA.
Methods: Anti-MFN1 IgG levels were measured using an in-house ELISA in the plasma from patients with GCA (n=65 in remission, n=14 with active disease), and 30 healthy controls (HC). Ultrapure mitochondria, isolated from HepG2 cells, were incubated with plasma from 65 patients with GCA in remission, and 16 HC, and assessed for IgA and IgG binding to the mitochondrial outer membrane using flow cytometry. Mitochondria were also opsonized with patient (n=58) or healthy control (n=10) plasma (6%), and subsequently incubated with platelets to determine the capacity of plasma factors, including AMAs, to promote mitochondrial-mediated platelet activation.
Results: Levels of anti-MFN1 IgG antibodies, a specific AMA, were elevated both in active disease (p< 0.0001) and in remission (p< 0.0001) in patients with GCA (Figure 1A). No differences in levels of anti-MFN1 antibodies were found between patients in remission and active disease for GCA (Figure 1B).No association was observed between anti-MFN1 antibodies and ESR levels (Figure 1C). Though total levels of IgG AMA did not reach statistical significance (p=0.38) in GCA patients compared to HC, IgA AMA levels were significantly higher in patients with GCA as compared to healthy individuals (p=0.003, Figure 2A). Levels of IgA AMA correlated with levels of IgG AMA in patients with GCA (Figure 2B), but not with levels of anti-MFN1 (data not shown). Finally, to investigate a potential pathogenic role of AMAs in GCA, exogenous mitochondria, derived from HepG2 cells, were opsonized with patient plasma and, upon washing, incubated with platelets from healthy individual. Plasma from patients with GCA had enhanced capacity to promote mitochondrial-mediated platelet activation as measured by P-selectin expression on platelet cell surface by flow cytometry, as compared to plasma from HC (p< 0.0001, Figure 3A). Platelet levels of P-selectin were associated with levels of anti-MFN1 IgG in patients with GCA (r=0.43, p=0.0012, Figure 3B).
Conclusion: We report the presence of AMAs in GCA. Presence of autoantibodies targeting mitochondria supports the hypothesis of antigenic mitochondrial components being present in GCA. Our data suggest that mitochondrial targeting by AMAs results in immune complex formation, potently activating platelets, possibly partaking in the thromboembolic morbidity and mortality of the disease. Targeting key drivers of mitochondrial extrusion in GCA could lead to new therapeutic interventions, including suppression of platelet activation.
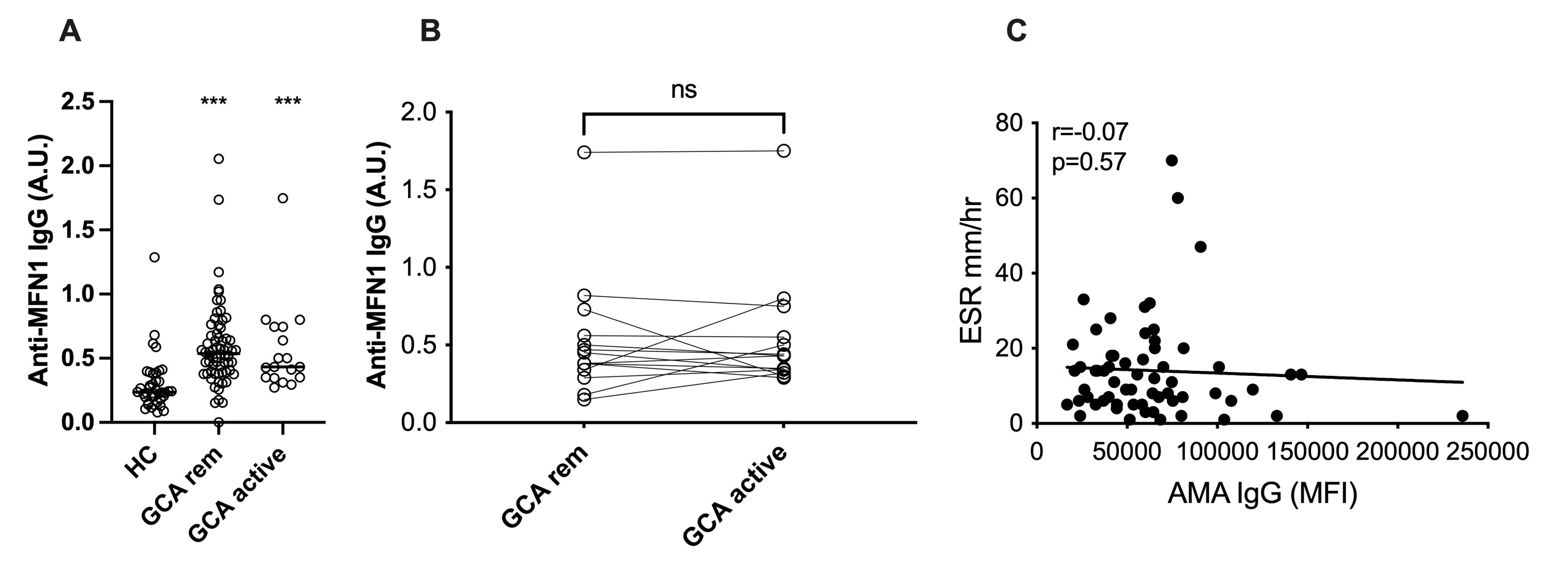
Figure 1. Anti-mitochondrial antibodies in giant cell arteritis. A) Levels of anti-MFN1 IgG antibodies were analyzed in the plasma of patients with giant cell arteritis (GCA) both in active disease and in remission (rem) and compared to healthy controls (HC). B) Anti-MFN1 IgG levels in patients at time-point of remission (rem) as well as matched active disease (active) as assessed by physician global assessment (PGA) in GCA. C) Correlation between levels of anti-MFN1 IgG antibodies and ESR. For statistical analyses, Mann-Whitney U test (A), Wilcoxon (B), and Spearman’s correlation (C) were used. *** p<0.001.
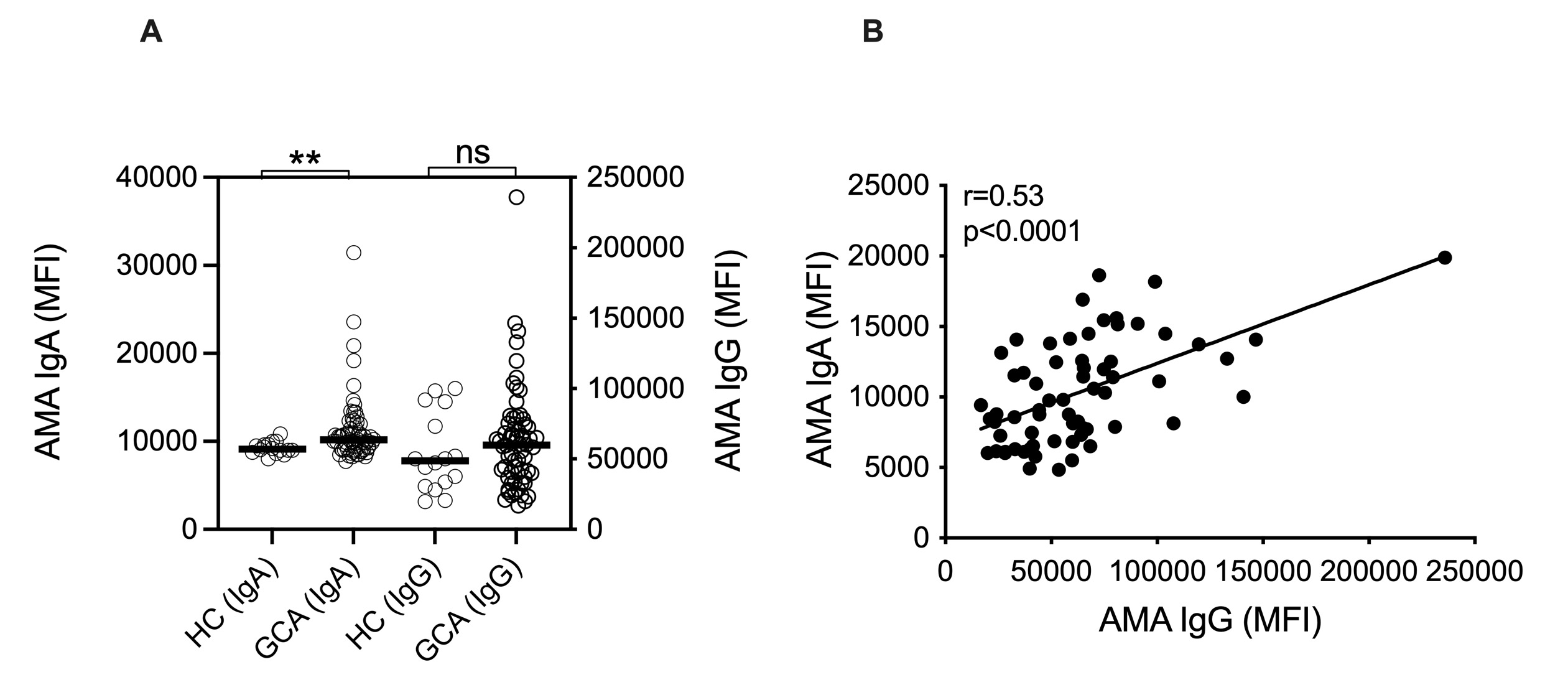
Figure 2. IgA and IgG anti-mitochondrial antibodies in giant cell arteritis. A) Levels of IgA and IgG anti-mitochondrial antibodies (AMA) were measured in the plasma of patients with giant cell arteritis (GCA) and health controls (HC) by flow cytometry. Results are presented as the mean fluorescence intensity (MFI). B) Correlation analysis between IgA AMA levels and IgG AMA levels in patients with GCA. Statistical analyses were done by Mann-Whitney U test (A) and Spearman’s correlation (B). ** p<0.01.
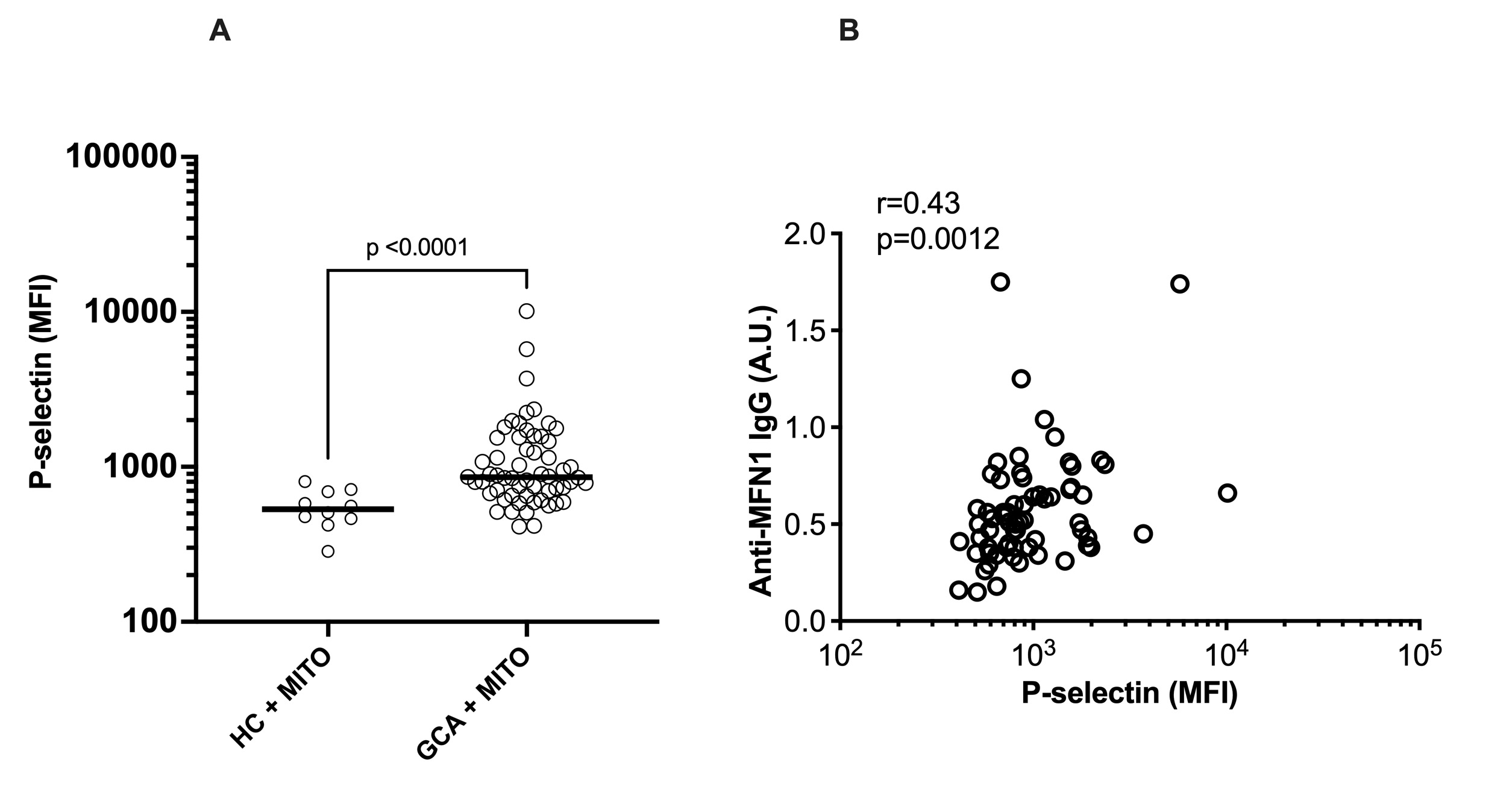
Figure 3. Mitochondrial-mediated platelet activation in giant cell arteritis. A) Platelet rich plasma (PRP) from a healthy individual was exposed to mitochondria (mito) in the presence of plasma of patients with giant cell arteritis (GCA, (n=58) and healthy controls (HC, n=10), and P-selectin expression on platelet measured by flow cytometry. Results are presented as the mean fluorescence intensity (MFI). B) Correlation analysis between levels of anti-MFN1 IgG and in vitro-induction of P-selectin on platelets in patients with GCA. Statistical analyses by Mann-Whitney U test (A) and Spearman’s correlation (B).
D. Michailidou: Chemocentryx, 1; P. Grayson: None; P. Hermanson: None; J. Armando Gonzalez-Chapa: None; D. Cuthbertson: None; N. Khalidi: AbbVie/Abbott, 5, Bristol-Myers Squibb(BMS), 5, GlaxoSmithKlein(GSK), 1, Otsuka, 1, 6, Roche, 1, 6; C. Koening: Amgen, 1; C. Langford: AbbVie, 12, Non-paid consultant, AstraZeneca, 5, 12, Non-paid consultant, Bristol-Myers Squibb(BMS), 5, 12, Non-paid consultant, GlaxoSmithKlein(GSK), 5; C. McAlear: None; L. Moreland: Boehringer-Ingelheim, 12, member of independent Data Safety Monitoring Board, Celltrion, 12, member of independent Data Safety Monitoring Board; C. Pagnoux: AstraZeneca, 1, 2, 6, GlaxoSmithKlein(GSK), 1, 6, Otsuka, 1, 2, 5, 6, Pfizer, 5, Roche, 2; P. Seo: Amgen, 1, Janssen, 1; A. Sreih: Bristol Myers Squibb, 3; K. Warrington: Bristol-Myers Squibb(BMS), 5, Chemocentryx, 1, 6, Eli Lilly, 5, kiniksa, 5; P. Monach: Genentech, 12, Lecture with honorarium, HI-Bio, 2; P. Merkel: AbbVie/Abbott, 5, Amgen, 2, 5, ArGenx, 2, AstraZeneca, 2, 5, Boehringer-Ingelheim, 2, 5, Bristol-Myers Squibb(BMS), 2, 5, Cabaletta, 2, CSL Behring, 2, Eicos, 5, Electra, 5, Genentech, 5, GlaxoSmithKlein(GSK), 2, 5, HiBio, 2, InflaRx, 2, 5, Janssen, 2, Jubilant, 2, Kyverna, 2, 11, MiroBio, 2, Neutrolis, 5, Novartis, 2, NS Pharma, 2, Q32, 2, Regeneron, 2, Sanofi, 2, Sparrow, 2, Takeda, 2, 5, UpToDate, 9, Visterra, 2; C. Lood: Amytryx, 5, Boehringer-Ingelheim, 5, Bristol-Myers Squibb(BMS), 5, Citryll, 2, Eli Lilly, 5, Gilead, 5, Horizon Therapeutics, 5, Pfizer, 5, Redd Pharma, 5, 11.



