Poster Session C
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (2195–2226) Spondyloarthritis Including Psoriatic Arthritis – Diagnosis, Manifestations, & Outcomes Poster III: SpA
2209: Prevalence and Clinical Characteristics of Late Onset Axial Spondyloarthritis: Results from a Multicentre Nationwide Study
Tuesday, November 14, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- SR
Sofia Ramiro, MD, PhD
Leiden University Medical Center
Bunde, NetherlandsDisclosure information not submitted.
Abstract Poster Presenter(s)
Margarida Lucas Rocha1, Rita Torres2, Sofia Ramiro3, Alice Morais Castro4, Alice Neves5, Ana Martins6, Ana Teodósio Chícharo1, Beatriz Mendes7, Carolina Ochôa Matos8, Catarina Soares9, Cláudia Miguel10, Cláudia Pinto Oliveira11, Hugo Parente12, J. A. Melo Gomes13, Mariana Luís14, Mariana Santos15, Maura Couto16, Miguel Bernardes17, Paula Valente18, Roberto Costa19, Sandra Sousa4, Jaime Branco20, Fernando Pimentel-Santos21 and Alexandre Sepriano22, 1Rheumatology Department, Centro Hospitalar Universitário do Algarve, Faro, Portugal, 2Hospital Egas Moniz, Lisboa, Portugal, 3Department of Rheumatology, Leiden University Medical Center, Leiden, Netherlands, 4Departamento de Reumatologia, Hospital Garcia de Orta, Almada, Portugal, 5Instituto Português de Reumatologia, Lisboa, Portugal, 6Serviço de Reumatologia, Centro Hospitalar Universitário São João; Serviço de Medicina, Faculdade de Medicina da Universidade do Porto, Porto, Portugal, 7Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal, 8Centro Académico de Medicina de Lisboa, Lisbon, Portugal, 9Centro Unidade Local de Saúde do Alto Minho, Viana do Castelo, Portugal, 10Instituto Português de Reumatologia, Lisbon, Portugal, 11Serviço de Reumatologia, Centro Hospitalar do Baixo Vouga, Aveiro, Portugal, 12Serviço de Reumatologia do Centro Unidade Local de Saúde do Alto Minho, Viana do Castelo, Portugal, 13Clínica Reumatológica Dr. Melo Gomes, Lisboa, Portugal, 14Serviço de Reumatologia – Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal, 15Serviço de Reumatologia do Centro Hospitalar Lisboa Ocidental, Hospital de Egas Moniz EPE, Lisboa, Portugal, 16Unidade de Reumatologia, Centro Hospitalar Tondela-Viseu, Viseu, Portugal, 17Rheumatology Department, Centro Hospitalar e Universitário de São João, Porto, Portugal, 18Serviço de Reumatologia, Centro Hospitalar Entre o Douro e o Vouga, Santa Maria da Feira, Portugal, 19Centro Hospitalar Lisboa Norte, Lisboa, Portugal, 20CHLO, EPE - Hospital Egas Moniz, Lisbon, Portugal, 21NOVA Medical School; Universidade NOVA e Lisboa, Lisboa, Portugal, 22Leiden University Medical Centre, Portela Loures, Portugal
Background/Purpose: Axial spondyloarthritis (axSpA) typically starts before the fourth decade of life. Consistent with that, the Assessment of SpondyloArthritis international Society (ASAS) classification criteria for axSpA should be applied only in patients with chronic back pain starting before 45 years of age. It has, however, been suggested that axSpA can sometimes start later in life with a distinctive phenotype, the so-called 'late onset axSpA' (lo-axSpA). There is, nevertheless, only limited data in support of the existence of such phenotype. We aimed to evaluate the occurrence of lo-axSpA and if these patients differ from those with early onset axSpA (eo-axSpA).
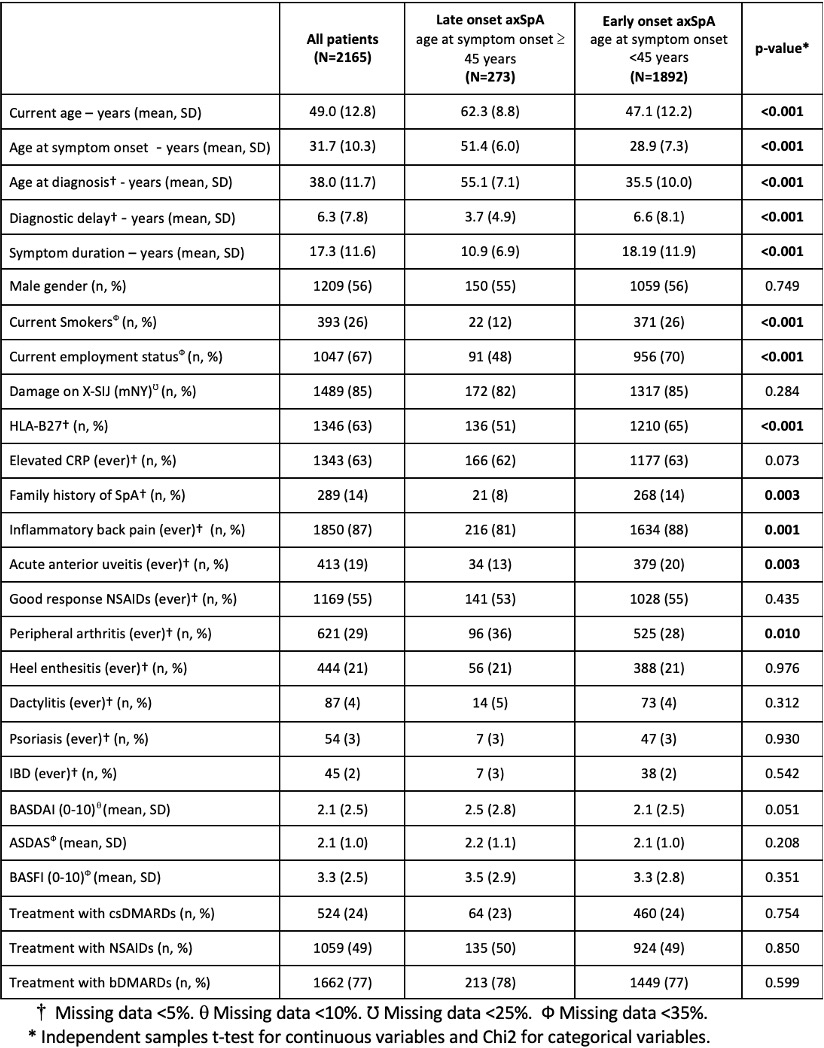
Methods: We performed a cross-sectional, multicentre, nationwide study using data from Reuma.pt, the Portuguese registry of patients with rheumatic diseases. Adult patients with the clinical diagnosis of axSpA, according to their treating rheumatologist, and with available information on the age of symptom onset were included. Lo-axSpA was defined as axSpA with a symptom onset ≥ 45 years of age. Demographic characteristics (e.g., age, gender, smoking status, and employment), SpA features [12 features (see Table) recorded as ever present, i.e., any time in the past or at the current study visit], measures of disease activity (ASDAS and BASDAI), disability (BASFI) and treatment with NSAIDs, csDMARDs and bDMARDs were compared between patients with lo-axSpA and eo-axSpA at the last available visit at the time of data extraction (13/12/2022).
Results: In total, 2165 patients with axSpA were included. The mean (standard deviation; SD) age at symptom onset was 32 (10) years and the mean (SD) symptom duration was 17 (12) years. The majority of the patients were male (56%), most had definite damage on pelvic radiographs according to the modified New York criteria (85%) and were treated with bDMARDs (77%). Out of the total 2165 patients, 273 (13%) had symptom onset ≥ 45 years and were therefore labelled as lo-axSpA. There were no differences in disease activity, disability or treatment between patients with lo-axSpA and eo-axSpA (Table). There were, however, some notable differences between the two groups. Patients with lo-axSpA were less often positive for HLA-B27 (51% vs 65%), less likely to have family history of SpA (8% vs 14%), acute anterior uveitis (13% vs 20%) and inflammatory back pain (81% vs 88%) than patients with eo-axSpA. On the contrary, patients with lo-axSpA had more peripheral arthritis (36% vs 28%) than patients with eo-axSpA.
Conclusion: This study shows that axSpA indeed starts before 45 years of age in the vast majority of the patients. Even though recall bias cannot be entirely ruled out, clinicians should however be aware that late-onset disease, though infrequent, may in some cases exist. This minority phenotype has a weaker association with HLA-B27, a lower probability of family history, inflammatory back pain or uveitis but more peripheral involvement.
M. Lucas Rocha: None; R. Torres: None; S. Ramiro: AbbVie, 2, 5, Eli Lilly, 2, Galapagos, 5, MSD, 2, 5, Novartis, 2, 5, Pfizer, 2, 5, Sanofi, 2, UCB Pharma, 2, 5; A. Morais Castro: None; A. Neves: None; A. Martins: None; A. Teodósio Chícharo: None; B. Mendes: None; C. Ochôa Matos: None; C. Soares: None; C. Miguel: None; C. Pinto Oliveira: None; H. Parente: None; J. A. Melo Gomes: None; M. Luís: None; M. Santos: None; M. Couto: None; M. Bernardes: None; P. Valente: None; R. Costa: None; S. Sousa: None; J. Branco: None; F. Pimentel-Santos: None; A. Sepriano: None.
Background/Purpose: Axial spondyloarthritis (axSpA) typically starts before the fourth decade of life. Consistent with that, the Assessment of SpondyloArthritis international Society (ASAS) classification criteria for axSpA should be applied only in patients with chronic back pain starting before 45 years of age. It has, however, been suggested that axSpA can sometimes start later in life with a distinctive phenotype, the so-called 'late onset axSpA' (lo-axSpA). There is, nevertheless, only limited data in support of the existence of such phenotype. We aimed to evaluate the occurrence of lo-axSpA and if these patients differ from those with early onset axSpA (eo-axSpA).
Methods: We performed a cross-sectional, multicentre, nationwide study using data from Reuma.pt, the Portuguese registry of patients with rheumatic diseases. Adult patients with the clinical diagnosis of axSpA, according to their treating rheumatologist, and with available information on the age of symptom onset were included. Lo-axSpA was defined as axSpA with a symptom onset ≥ 45 years of age. Demographic characteristics (e.g., age, gender, smoking status, and employment), SpA features [12 features (see Table) recorded as ever present, i.e., any time in the past or at the current study visit], measures of disease activity (ASDAS and BASDAI), disability (BASFI) and treatment with NSAIDs, csDMARDs and bDMARDs were compared between patients with lo-axSpA and eo-axSpA at the last available visit at the time of data extraction (13/12/2022).
Results: In total, 2165 patients with axSpA were included. The mean (standard deviation; SD) age at symptom onset was 32 (10) years and the mean (SD) symptom duration was 17 (12) years. The majority of the patients were male (56%), most had definite damage on pelvic radiographs according to the modified New York criteria (85%) and were treated with bDMARDs (77%). Out of the total 2165 patients, 273 (13%) had symptom onset ≥ 45 years and were therefore labelled as lo-axSpA. There were no differences in disease activity, disability or treatment between patients with lo-axSpA and eo-axSpA (Table). There were, however, some notable differences between the two groups. Patients with lo-axSpA were less often positive for HLA-B27 (51% vs 65%), less likely to have family history of SpA (8% vs 14%), acute anterior uveitis (13% vs 20%) and inflammatory back pain (81% vs 88%) than patients with eo-axSpA. On the contrary, patients with lo-axSpA had more peripheral arthritis (36% vs 28%) than patients with eo-axSpA.
Conclusion: This study shows that axSpA indeed starts before 45 years of age in the vast majority of the patients. Even though recall bias cannot be entirely ruled out, clinicians should however be aware that late-onset disease, though infrequent, may in some cases exist. This minority phenotype has a weaker association with HLA-B27, a lower probability of family history, inflammatory back pain or uveitis but more peripheral involvement.
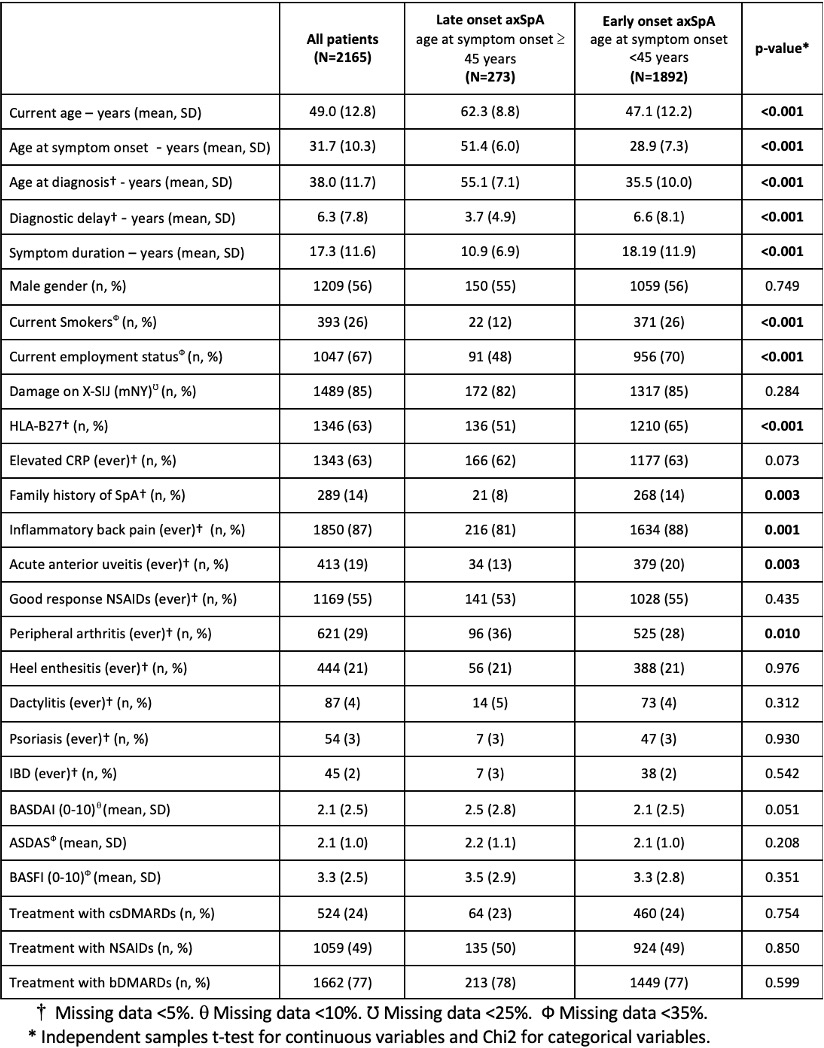
Comparison of patient and disease characteristics between patients with late and early onset axSpA.
M. Lucas Rocha: None; R. Torres: None; S. Ramiro: AbbVie, 2, 5, Eli Lilly, 2, Galapagos, 5, MSD, 2, 5, Novartis, 2, 5, Pfizer, 2, 5, Sanofi, 2, UCB Pharma, 2, 5; A. Morais Castro: None; A. Neves: None; A. Martins: None; A. Teodósio Chícharo: None; B. Mendes: None; C. Ochôa Matos: None; C. Soares: None; C. Miguel: None; C. Pinto Oliveira: None; H. Parente: None; J. A. Melo Gomes: None; M. Luís: None; M. Santos: None; M. Couto: None; M. Bernardes: None; P. Valente: None; R. Costa: None; S. Sousa: None; J. Branco: None; F. Pimentel-Santos: None; A. Sepriano: None.



