Poster Session C
Vasculitis
Session: (2387–2424) Vasculitis – Non-ANCA-Associated & Related Disorders Poster III
2401: A Study Defining the Optimal Sonographic Parameters for Intima-Media Thickness in Diagnosing Giant Cell Arteritis
Tuesday, November 14, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- SC
Sharon Cowley, MRCP, MBBCH
Tallaght University Hospital, Dublin
Dublin, Dublin, IrelandDisclosure information not submitted.
Abstract Poster Presenter(s)
Colm Kirby1, Sharon Cowley2, Rachael Flood1, Ronan Mullan1, Grainne Murphy3 and David Kane4, 1Tallaght University Hospital, Dublin, Ireland, 2Tallaght University Hospital, Dublin, Dublin, Ireland, 3Cork University Hospital, Cork, Ireland, 4Tallaght University Hospital & Trinity College Dublin, Dublin, Ireland
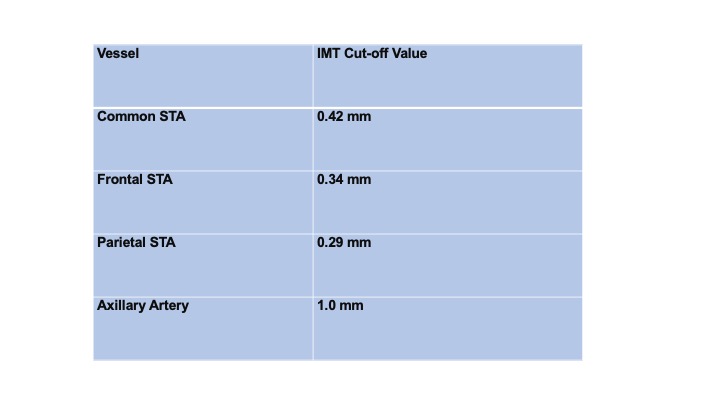
Background/Purpose: In recent years, Temporal Artery US (TAUS) incorporating Axillary Artery US (AAUS) has become a reliable alternative to biopsy for diagnosing GCA but studies have shown heterogenous results for its' diagnostic performance for this purpose (1,2). Published values for Intima-Media Thickness (IMT) exist which can differentiate an inflamed vessel from a normal one but have not yet been validated (Table 1). We aimed to establish what IMT values in each vascular territory could reliably support or refute a diagnosis of GCA.
Methods: We performed a prospective study of all newly diagnosed GCA patients (clinical diagnosis, verified by 2 rheumatologists after 6 months) who had a positive baseline vascular US (n= 57) presenting to our Rapid Access GCA clinic over 18 months. US of all 6 branches of the Superficial Temporal Arteries (STA) and both Axillary Arteries (AA) were performed on all patients using a GE P9 device. Sonographic abnormalities considered indicative of vasculitis in the temporal arteries included the halo sign and non-compressible arteries with a thickened IMT (3). In the axillary arteries, a halo sign and an intima-media thickness of >1.0mm was considered positive. We performed Chi-Square test with ROC analysis to determine the sensitivity and specificity of each measured IMT value in each branch of the STA and AA.
Results: 66/124 patients had a clinical diagnosis of GCA at 6 months. 57 of these patients had a positive baseline vascular US. Our cohort consisted of 61% males (n=35) with a mean age of 74.4 years. Overall, US had a sensitivity of 86.4% and a specificity of 82.8% for a clinical diagnosis of GCA. Table 2 demonstrates the sonographically-defined IMT values in our cohort for each branch of the STA and AA which can irrefutably exclude (i.e. sensitivity 100%) or diagnose (i.e. specificity 100%) GCA.
Conclusion: Our data provides a template which can guide clinician-sonographers when interpreting vascular US images in cases of suspected GCA. The conventional method of identifying a halo with a non-compressible artery is somewhat limited due to conflicting results of its diagnostic performance in clinical studies to date. By incorporating IMT measurement into the routine US protocol for GCA, clinicians can attain increased diagnostic accuracy if the above thresholds are met.
.jpg)
C. Kirby: None; S. Cowley: None; R. Flood: None; R. Mullan: None; G. Murphy: None; D. Kane: None.
Background/Purpose: In recent years, Temporal Artery US (TAUS) incorporating Axillary Artery US (AAUS) has become a reliable alternative to biopsy for diagnosing GCA but studies have shown heterogenous results for its' diagnostic performance for this purpose (1,2). Published values for Intima-Media Thickness (IMT) exist which can differentiate an inflamed vessel from a normal one but have not yet been validated (Table 1). We aimed to establish what IMT values in each vascular territory could reliably support or refute a diagnosis of GCA.
Methods: We performed a prospective study of all newly diagnosed GCA patients (clinical diagnosis, verified by 2 rheumatologists after 6 months) who had a positive baseline vascular US (n= 57) presenting to our Rapid Access GCA clinic over 18 months. US of all 6 branches of the Superficial Temporal Arteries (STA) and both Axillary Arteries (AA) were performed on all patients using a GE P9 device. Sonographic abnormalities considered indicative of vasculitis in the temporal arteries included the halo sign and non-compressible arteries with a thickened IMT (3). In the axillary arteries, a halo sign and an intima-media thickness of >1.0mm was considered positive. We performed Chi-Square test with ROC analysis to determine the sensitivity and specificity of each measured IMT value in each branch of the STA and AA.
Results: 66/124 patients had a clinical diagnosis of GCA at 6 months. 57 of these patients had a positive baseline vascular US. Our cohort consisted of 61% males (n=35) with a mean age of 74.4 years. Overall, US had a sensitivity of 86.4% and a specificity of 82.8% for a clinical diagnosis of GCA. Table 2 demonstrates the sonographically-defined IMT values in our cohort for each branch of the STA and AA which can irrefutably exclude (i.e. sensitivity 100%) or diagnose (i.e. specificity 100%) GCA.
Conclusion: Our data provides a template which can guide clinician-sonographers when interpreting vascular US images in cases of suspected GCA. The conventional method of identifying a halo with a non-compressible artery is somewhat limited due to conflicting results of its diagnostic performance in clinical studies to date. By incorporating IMT measurement into the routine US protocol for GCA, clinicians can attain increased diagnostic accuracy if the above thresholds are met.
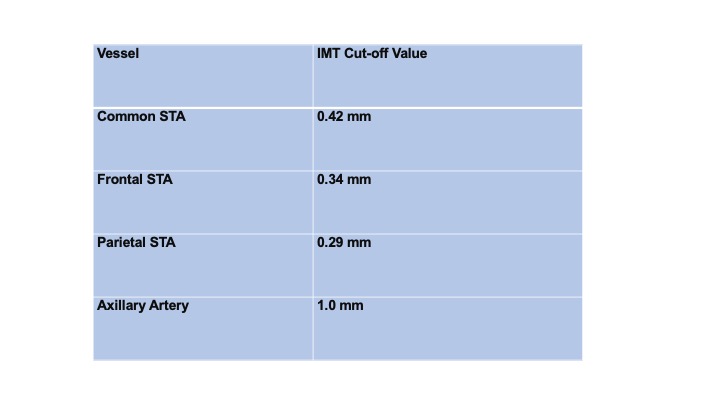
Table 1: IMT Cut-off values used to diagnose GCA on vascular US (4).
.jpg)
Table 2: Baseline Intima-Media Thickness (IMT) values in each Superficial Temporal (STA) and Axillary Artery (AA) branch that give 100%, >95% and >90% sensitivity and specificity for a clinical diagnosis of GCA. Rt=right, Lt=left.
C. Kirby: None; S. Cowley: None; R. Flood: None; R. Mullan: None; G. Murphy: None; D. Kane: None.



