Poster Session C
Periodic fever syndromes, autoinflammatory diseases, Still’s disease and MAS/HLH
Session: (1913–1944) Miscellaneous Rheumatic & Inflammatory Diseases Poster III
1924: Impact of the COVID-19 Pandemic on Clinical and Psychosocial Features of Patients with UCTD
Tuesday, November 14, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- LM
Lucy Masto, BS
Hospital for Special Surgery
New York, NY, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Caroline Siegel1, Lucy Masto1, Amaya Smole1, Bessie Stamm1, JoAnn Vega1, Dongmei Sun1, Deanna Jannat-Khah1, Michael Lockshin2, Lisa Sammaritano2 and Medha Barbhaiya2, 1Hospital for Special Surgery, New York, NY, 2Hospital for Special Surgery, Weill Cornell Medicine, New York, NY
Background/Purpose: The early COVID-19 pandemic led to physical and psychological burdens for patients with systemic rheumatic diseases, whether or not they had had COVID-19. To assess the impact of this public health crisis on people with UCTD, we compared demographic, clinical and psychosocial features between patients enrolled in our UCTD registry before versus after the initial wave of the COVID-19 pandemic in New York City.
Methods: This retrospective cohort study included patients enrolled in an academic hospital-based UCTD registry with positive ANA, ≥1 sign/symptom of a CTD, who do not meet ACR/EULAR-endorsed classification criteria for SLE, RA, SSc, Primary Sjögren's, Idiopathic Inflammatory Myopathy, or 2006 Revised Sapporo Criteria for APS. We collected demographic information from patients and clinical characteristics from chart review. Upon enrollment, participants completed the 36-Item Short Form Health Survey (SF-36) to assess health-related quality of life (HRQoL), General Anxiety Disorder-7 (GAD-7), Beck Depression Inventory (BDI), and Fatigue Severity Scale (FSS). We compared demographic, clinical, and psychosocial variables between participants enrolled April 2018-February 2020 ("pre-COVID-19") to those enrolled March 2020-May 2023 ("post-COVID-19"). We used multivariable linear regression to evaluate the association between enrollment date (before vs. after pandemic onset) and HRQoL (i.e. SF-36 physical component summary [PCS] and mental component summary [MCS] scores).
Results: There were 78 patients with UCTD: median age 49.5 years [IQR 34.3, 57.8], 96% female, 74% White race, 74% non-Hispanic/Latino ethnicity. There were no differences in demographics, CTD manifestations, comorbidities, or medications between groups [Table 1].
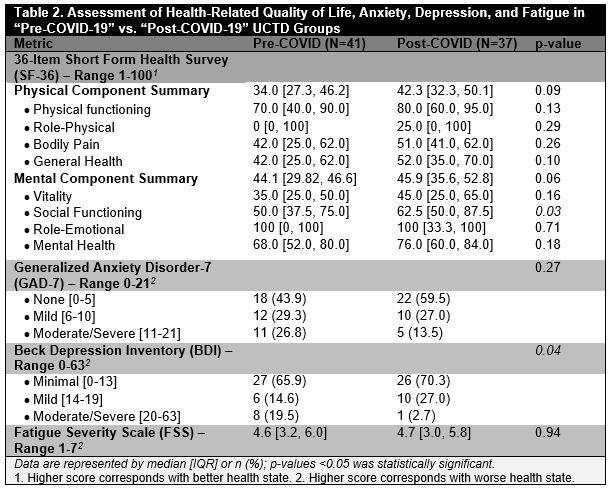
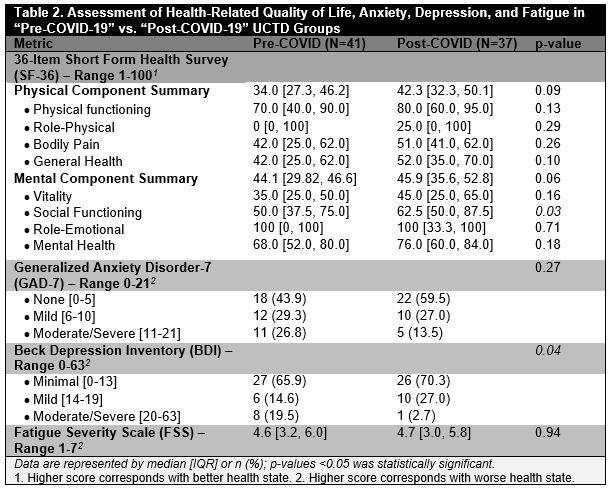
In the post-COVID-19 group, the SF-36 'social functioning' score was higher (i.e. better) than in the pre-COVID-19 group (median [IQR] 62.5 [50.0, 87.5] vs. 50.0 [37.5, 75.0], p=0.03). The post-COVID-19 PCS and MCS scores were numerically higher (PCS: 42.3 [32.3, 50.1] vs. 34.0 [27.3, 46.2], p=0.09; MCS: 45.9 [35.6, 52.8] vs. 44.1 [29.8, 46.6], p=0.06). The post-COVID-19 vs. pre-COVID-19 group had a higher frequency of BDI-defined mild depression and a lower frequency of moderate/severe depression (p=0.04); GAD-7 and FSS scores did not differ between groups [Table 2].
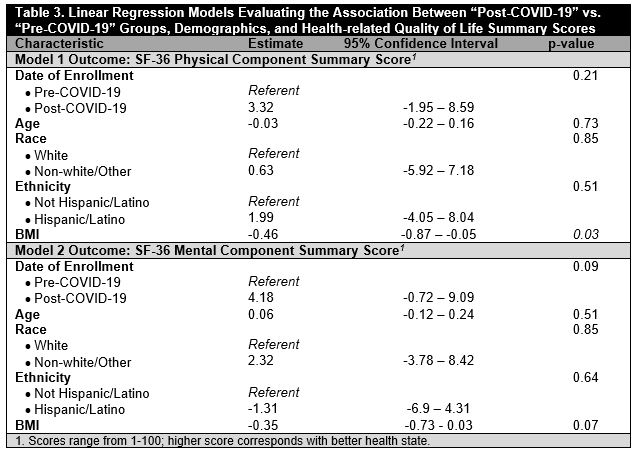
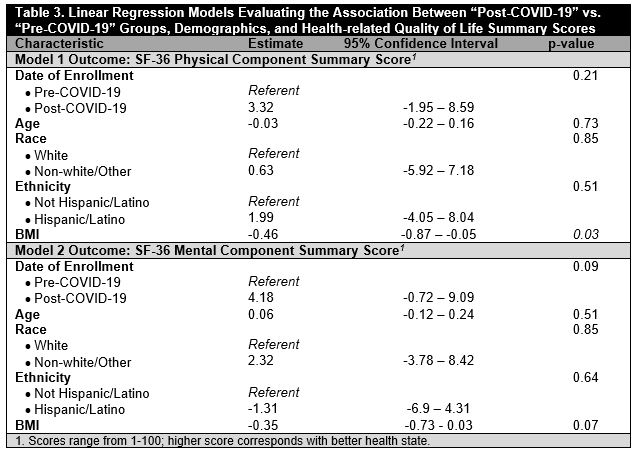
After adjustment, the post-COVID-19 group had slightly but not significantly increased PCS (Estimate: 3.32, 95% CI: -1.95 – 8.59, p=0.21) and MCS (Estimate:4.18, 95% CI -0.72 – 9.09, p=0.09) scores compared to the pre-COVID-19 group. BMI was inversely associated with PCS score (Estimate -0.46; 95% CI -0.87 – -0.05, p=0.03) [Table 3].
Conclusion: Comparing demographically and clinically similar patients with UCTD enrolled in our registry before and after March 2020, we found that those assessed after the onset of the COVID-19 pandemic had decreased moderate/severe depression and increased social functioning with a trend toward improved HRQoL. Our results suggest that circumstances of the "post-COVID-19" era may have contributed to unexpected improvement in some aspects of UCTD patients' wellbeing; further research with a larger sample is needed to confirm and elucidate these findings.
.jpg)
C. Siegel: UCB, 12, fellowship training is supported by UCB Women's Health Fellowship Program; L. Masto: None; A. Smole: None; B. Stamm: None; J. Vega: None; D. Sun: None; D. Jannat-Khah: AstraZeneca, 12, stock ownership, Cytodyn, 12, stock ownershil[, Walgreens Boots Alliance, 12, stock ownership; M. Lockshin: None; L. Sammaritano: None; M. Barbhaiya: None.
Background/Purpose: The early COVID-19 pandemic led to physical and psychological burdens for patients with systemic rheumatic diseases, whether or not they had had COVID-19. To assess the impact of this public health crisis on people with UCTD, we compared demographic, clinical and psychosocial features between patients enrolled in our UCTD registry before versus after the initial wave of the COVID-19 pandemic in New York City.
Methods: This retrospective cohort study included patients enrolled in an academic hospital-based UCTD registry with positive ANA, ≥1 sign/symptom of a CTD, who do not meet ACR/EULAR-endorsed classification criteria for SLE, RA, SSc, Primary Sjögren's, Idiopathic Inflammatory Myopathy, or 2006 Revised Sapporo Criteria for APS. We collected demographic information from patients and clinical characteristics from chart review. Upon enrollment, participants completed the 36-Item Short Form Health Survey (SF-36) to assess health-related quality of life (HRQoL), General Anxiety Disorder-7 (GAD-7), Beck Depression Inventory (BDI), and Fatigue Severity Scale (FSS). We compared demographic, clinical, and psychosocial variables between participants enrolled April 2018-February 2020 ("pre-COVID-19") to those enrolled March 2020-May 2023 ("post-COVID-19"). We used multivariable linear regression to evaluate the association between enrollment date (before vs. after pandemic onset) and HRQoL (i.e. SF-36 physical component summary [PCS] and mental component summary [MCS] scores).
Results: There were 78 patients with UCTD: median age 49.5 years [IQR 34.3, 57.8], 96% female, 74% White race, 74% non-Hispanic/Latino ethnicity. There were no differences in demographics, CTD manifestations, comorbidities, or medications between groups [Table 1].
In the post-COVID-19 group, the SF-36 'social functioning' score was higher (i.e. better) than in the pre-COVID-19 group (median [IQR] 62.5 [50.0, 87.5] vs. 50.0 [37.5, 75.0], p=0.03). The post-COVID-19 PCS and MCS scores were numerically higher (PCS: 42.3 [32.3, 50.1] vs. 34.0 [27.3, 46.2], p=0.09; MCS: 45.9 [35.6, 52.8] vs. 44.1 [29.8, 46.6], p=0.06). The post-COVID-19 vs. pre-COVID-19 group had a higher frequency of BDI-defined mild depression and a lower frequency of moderate/severe depression (p=0.04); GAD-7 and FSS scores did not differ between groups [Table 2].
After adjustment, the post-COVID-19 group had slightly but not significantly increased PCS (Estimate: 3.32, 95% CI: -1.95 – 8.59, p=0.21) and MCS (Estimate:4.18, 95% CI -0.72 – 9.09, p=0.09) scores compared to the pre-COVID-19 group. BMI was inversely associated with PCS score (Estimate -0.46; 95% CI -0.87 – -0.05, p=0.03) [Table 3].
Conclusion: Comparing demographically and clinically similar patients with UCTD enrolled in our registry before and after March 2020, we found that those assessed after the onset of the COVID-19 pandemic had decreased moderate/severe depression and increased social functioning with a trend toward improved HRQoL. Our results suggest that circumstances of the "post-COVID-19" era may have contributed to unexpected improvement in some aspects of UCTD patients' wellbeing; further research with a larger sample is needed to confirm and elucidate these findings.
.jpg)
C. Siegel: UCB, 12, fellowship training is supported by UCB Women's Health Fellowship Program; L. Masto: None; A. Smole: None; B. Stamm: None; J. Vega: None; D. Sun: None; D. Jannat-Khah: AstraZeneca, 12, stock ownership, Cytodyn, 12, stock ownershil[, Walgreens Boots Alliance, 12, stock ownership; M. Lockshin: None; L. Sammaritano: None; M. Barbhaiya: None.



