Poster Session B
Session: (1256–1263) Psychology/Social Science – Interprofessional Poster
1260: Optimal Approaches for Reducing Depressive Symptoms in Rheumatoid Arthritis Patients Based on Psychological Interventions: A Systematic Review and Network Meta-analysis
Monday, November 13, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- ZL
Zhang Lijuan, PhD
Shanghai jiaotong university
shanghai, Shanghai, ChinaDisclosure information not submitted.
Abstract Poster Presenter(s)
Zhang Lijuan and Wu Beiwen, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Background/Purpose: In recent years, numerous psychological interventions for rheumatoid arthritis (RA) patients have been developed. However, it remains unclear which psychological interventions are effective and preferred for their depressive symptoms. The purpose of this study was to identify the optimal psychological interventions approach for reducing depressive symptoms in RA patients.
Methods: The PubMed, Embase, PsycINFO, the Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang databases, and grey literature were searched between inception and 31 December 2022. Pairs of reviewers screened studies, abstracted aggregate level data, and appraised risk of bias with the Cochrane risk of bias tool. The network meta-analysis was conducted using STATA software version 14.0.
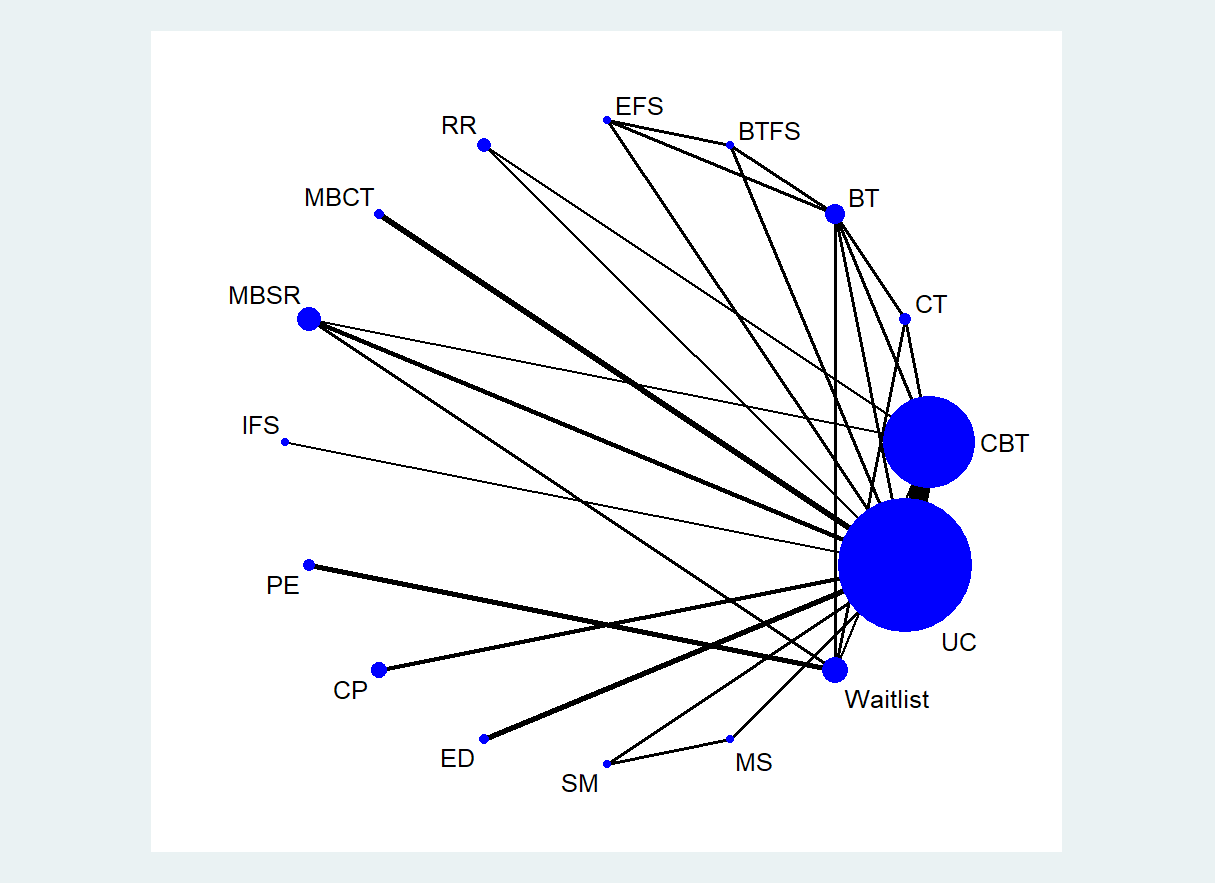
Results: A total of 23 randomized controlled trials, involving 1885 participants and 16 psychological interventions were included in our analyses. In this network meta-analysis, two interventions were associated with a greater reduction in symptoms of depression compared with treatment as usual care group: mindfulness-based cognitive therapy (MBCT) (standardized mean difference −1.67, 95% credible interval -2.23 to -1.10) and combined psychological intervention (CP) (−0.72, −1.16 to −0.28). Although most psychological interventions showed non-significant effects, the surface under the cumulative ranking curve (SUCRA) values revealed that the best psychological intervention for depression was MBCT (99.9%), followed by CP (85.6%), and Internal Family Systems (IFS) psychotherapeutic intervention (69.0%).
Conclusion: MBCT was the most recommended psychological intervention to accompany the depression among RA patients according to our network meta-analysis results.
.jpg)
.jpg)
Z. Lijuan: None; W. Beiwen: None.
Background/Purpose: In recent years, numerous psychological interventions for rheumatoid arthritis (RA) patients have been developed. However, it remains unclear which psychological interventions are effective and preferred for their depressive symptoms. The purpose of this study was to identify the optimal psychological interventions approach for reducing depressive symptoms in RA patients.
Methods: The PubMed, Embase, PsycINFO, the Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang databases, and grey literature were searched between inception and 31 December 2022. Pairs of reviewers screened studies, abstracted aggregate level data, and appraised risk of bias with the Cochrane risk of bias tool. The network meta-analysis was conducted using STATA software version 14.0.
Results: A total of 23 randomized controlled trials, involving 1885 participants and 16 psychological interventions were included in our analyses. In this network meta-analysis, two interventions were associated with a greater reduction in symptoms of depression compared with treatment as usual care group: mindfulness-based cognitive therapy (MBCT) (standardized mean difference −1.67, 95% credible interval -2.23 to -1.10) and combined psychological intervention (CP) (−0.72, −1.16 to −0.28). Although most psychological interventions showed non-significant effects, the surface under the cumulative ranking curve (SUCRA) values revealed that the best psychological intervention for depression was MBCT (99.9%), followed by CP (85.6%), and Internal Family Systems (IFS) psychotherapeutic intervention (69.0%).
Conclusion: MBCT was the most recommended psychological intervention to accompany the depression among RA patients according to our network meta-analysis results.
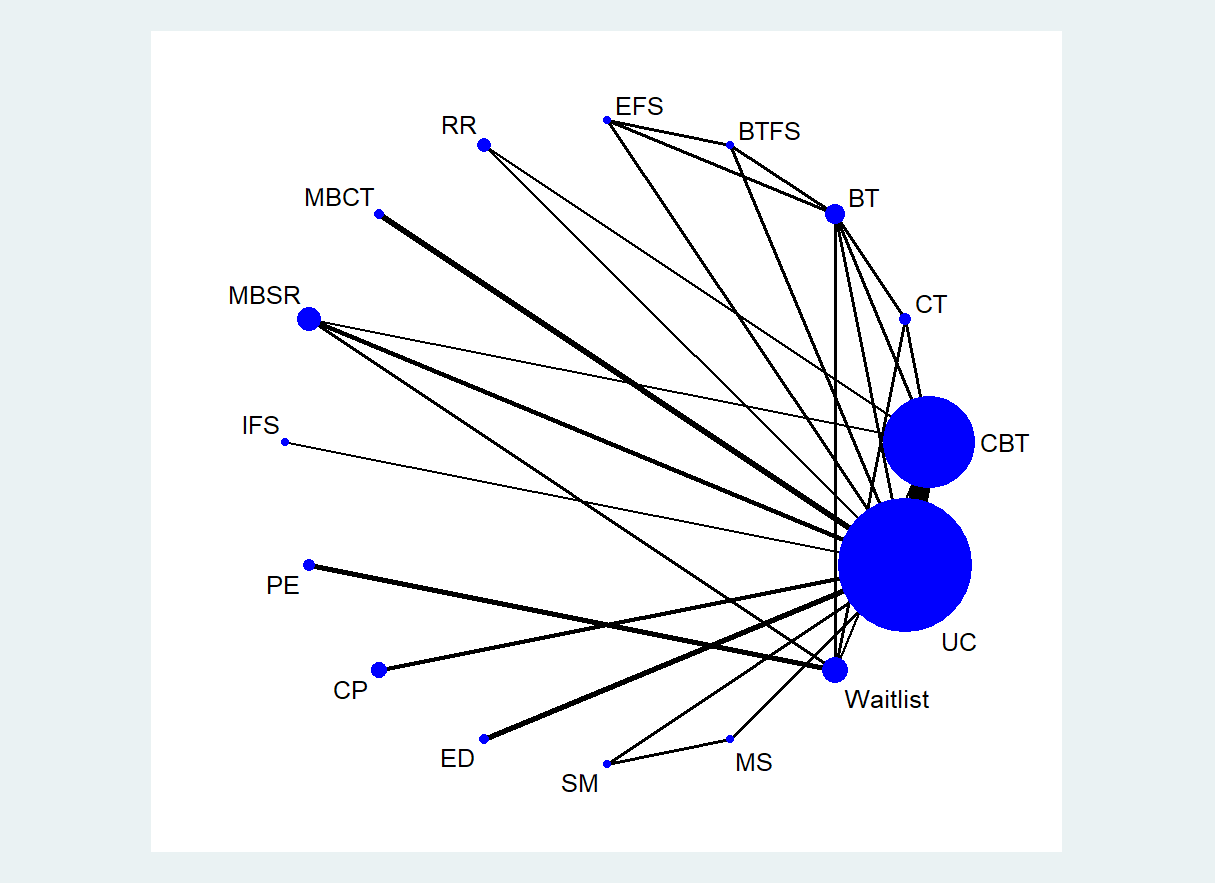
Figure 1 Network plots of depression at post-intervention. CBT: Cognitive behavioral Therapy; CT: the cognitive therapy; BT: the behavior therapy; BTFS: the behavior therapy with family support group; EFS: the education family support group; RR: Relaxation response training; MBCT: Mindfulness-Based Cognitive Therapy; MBSR: Mindfulness-Based Stress Reduction; IFS: Internal Family Systems; PE: Patients education; CP: Combined psychological intervention; ED: Emotional disclosure; SM: Stress Management; MS: Mutual Support; UC: Usual care.
.jpg)
Figure 2 Efficacy of different psychological intervention approaches compared to UC group. CBT: Cognitive behavioral Therapy; CT: the cognitive therapy; BT: the behavior therapy; BTFS: the behavior therapy with family support group; EFS: the education family support group; RR: Relaxation response training; MBCT: Mindfulness-Based Cognitive Therapy; MBSR: Mindfulness-Based Stress Reduction; IFS: Internal Family Systems; PE: Patients education; CP: Combined psychological intervention; ED: Emotional disclosure; SM: Stress Management; MS: Mutual Support; UC: Usual care.
.jpg)
Figure 3 The SUCRA plot and values based on cumulative probabilities of interventions. AUC: Area under curve; CBT: Cognitive behavioral Therapy; CT: the cognitive therapy; BT: the behavior therapy; BTFS: the behavior therapy with family support group; EFS: the education family support group; RR: Relaxation response training; MBCT: Mindfulness-Based Cognitive Therapy; MBSR: Mindfulness-Based Stress Reduction; IFS: Internal Family Systems; PE: Patients education; CP: Combined psychological intervention; ED: Emotional disclosure; SM: Stress Management; MS: Mutual Support; UC: Usual care.
Z. Lijuan: None; W. Beiwen: None.



