Poster Session B
Vasculitis
Session: (1534–1553) Vasculitis – ANCA-Associated Poster II: Epidemiology, Outcomes, & Classification
1538: Large Vessel Involvement in Antineutrophil Cytoplasmic Antibody- Associated Vasculitis: A Single Center Experience over Two Decades
Monday, November 13, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- MK
Abstract Poster Presenter(s)
Mahmut Kaymakci1, Mohanad Elfishawi1, Hannah Langenfeld2, Andrew Hanson2, Cynthia Crowson1, Melanie Bois1, Umar Ghaffar1, Ulrich Specks1, Matthew Koster1 and Kenneth Warrington1, 1Mayo Clinic, Rochester, MN, 2Department of Quantitative Health Sciences, Mayo Clinic, Rochester, MN
Background/Purpose: Anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV) is currently categorized under the small vessel vasculitides and includes granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA). There is limited knowledge about large vessel involvement in AAV (L-AAV), which is mainly described in case reports and small series. L-AAV can involve temporal arteries (TA-AAV), aorta (A-AAV), and periaortic soft tissue (PA-AAV). The objective of this study was to investigate the characteristics of L-AAV.
Methods: Patients older than 18 years at diagnosis of TA-AAV, A-AAV and PA-AAV seen at a single institution between January 1, 2000, and December 31, 2021, were identified through a proprietary medical text search algorithm. Patients were included if diagnosed with L-AAV by the treating physician, fulfilled 2022 American College of Rheumatology/ European Alliance of Associations for Rheumatology classification criteria for GPA, MPA or EGPA, had positive ANCA, and had more than one outpatient or inpatient visit. Arteritis of the temporal artery was based on histopathology whereas the diagnosis of aortitis and periaortitis could be either based on radiology or histopathology. Descriptive statistics were used to summarize patient characteristics and clinical manifestations. Survival rates were estimated using Kaplan-Meier methods. Overall observed survival was compared with lifetable rates from the US population. The standardized mortality ratio was estimated as the ratio of the observed and expected number of deaths.
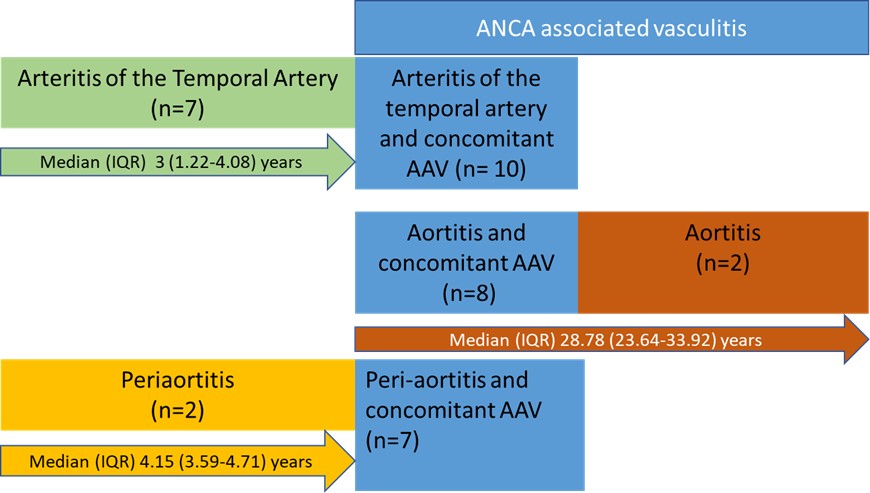
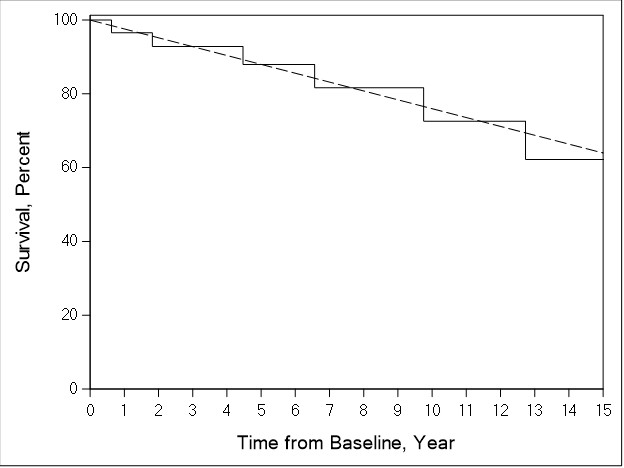
Results: The study cohort consists of 36 patients with L-AAV. Of those, 23 had p-ANCA/ MPO-ANCA and 13 had c-ANCA/ PR3- ANCA. Mean (SD) age at AAV diagnosis was 63.4 (12.79); 20 (56%) were male. Seventeen patients had TA-AAV, 10 had A-AAV and 9 had PA-AAV (Table 1). Most of the patients (n=25, 69%) were diagnosed with large vessel involvement and AAV within a one-year timespan (Figure 1). Inflammatory markers were elevated at the time of diagnosis of large vessel involvement. Twenty-five (69%) patients had histopathologic confirmation of AAV diagnosis. There was no overlap between TA-AAV, A-AAV and PA-AAV groups. Of the 17 patients with TA-AAV, 6 had inflammation of a temporal artery branch vessel. The most frequent site of involvement in the A-AAV group was the ascending thoracic aorta, whereas in the PA-AAV group, the abdominal aorta was most frequently involved. Glucocorticoids (36/36), rituximab (19/36), and methotrexate (18/36) were the most frequent treatments. During the study period 8 patients died (4 in TA-AAV, 3 in A-AAV, and 1 in PAAAV). There was no difference in mortality between this cohort of L-AAV patients and the general population (standardized mortality ratio: 0.99; 95% CI, 0.43- 1.95) (Figure 2).
Conclusion: This is the largest single-center cohort of patients with L-AAV to date. Clinicians should consider L-AAV in the differential diagnosis of vasculitides especially in the context of positive ANCA and atypical organ manifestations.
.jpg)
M. Kaymakci: None; M. Elfishawi: None; H. Langenfeld: None; A. Hanson: None; C. Crowson: None; M. Bois: None; U. Ghaffar: None; U. Specks: Amgen, 2, AstraZeneca, 2, 5, Boehringer-Ingelheim, 1, Bristol-Myers Squibb(BMS), 5, ChemoCentryx, 2, Genentech, 5, GlaxoSmithKlein(GSK), 5; M. Koster: None; K. Warrington: Bristol-Myers Squibb(BMS), 5, Chemocentryx, 1, 6, Eli Lilly, 5, kiniksa, 5.
Background/Purpose: Anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV) is currently categorized under the small vessel vasculitides and includes granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA). There is limited knowledge about large vessel involvement in AAV (L-AAV), which is mainly described in case reports and small series. L-AAV can involve temporal arteries (TA-AAV), aorta (A-AAV), and periaortic soft tissue (PA-AAV). The objective of this study was to investigate the characteristics of L-AAV.
Methods: Patients older than 18 years at diagnosis of TA-AAV, A-AAV and PA-AAV seen at a single institution between January 1, 2000, and December 31, 2021, were identified through a proprietary medical text search algorithm. Patients were included if diagnosed with L-AAV by the treating physician, fulfilled 2022 American College of Rheumatology/ European Alliance of Associations for Rheumatology classification criteria for GPA, MPA or EGPA, had positive ANCA, and had more than one outpatient or inpatient visit. Arteritis of the temporal artery was based on histopathology whereas the diagnosis of aortitis and periaortitis could be either based on radiology or histopathology. Descriptive statistics were used to summarize patient characteristics and clinical manifestations. Survival rates were estimated using Kaplan-Meier methods. Overall observed survival was compared with lifetable rates from the US population. The standardized mortality ratio was estimated as the ratio of the observed and expected number of deaths.
Results: The study cohort consists of 36 patients with L-AAV. Of those, 23 had p-ANCA/ MPO-ANCA and 13 had c-ANCA/ PR3- ANCA. Mean (SD) age at AAV diagnosis was 63.4 (12.79); 20 (56%) were male. Seventeen patients had TA-AAV, 10 had A-AAV and 9 had PA-AAV (Table 1). Most of the patients (n=25, 69%) were diagnosed with large vessel involvement and AAV within a one-year timespan (Figure 1). Inflammatory markers were elevated at the time of diagnosis of large vessel involvement. Twenty-five (69%) patients had histopathologic confirmation of AAV diagnosis. There was no overlap between TA-AAV, A-AAV and PA-AAV groups. Of the 17 patients with TA-AAV, 6 had inflammation of a temporal artery branch vessel. The most frequent site of involvement in the A-AAV group was the ascending thoracic aorta, whereas in the PA-AAV group, the abdominal aorta was most frequently involved. Glucocorticoids (36/36), rituximab (19/36), and methotrexate (18/36) were the most frequent treatments. During the study period 8 patients died (4 in TA-AAV, 3 in A-AAV, and 1 in PAAAV). There was no difference in mortality between this cohort of L-AAV patients and the general population (standardized mortality ratio: 0.99; 95% CI, 0.43- 1.95) (Figure 2).
Conclusion: This is the largest single-center cohort of patients with L-AAV to date. Clinicians should consider L-AAV in the differential diagnosis of vasculitides especially in the context of positive ANCA and atypical organ manifestations.
.jpg)
Table 1. Features of the study cohort.
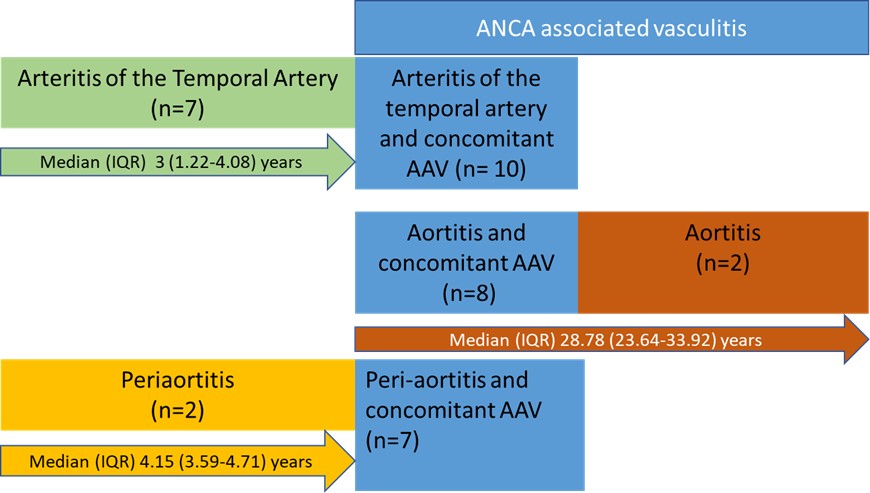
Figure 1. Timeline for the diagnosis of arteritis of temporal artery, aortitis, and periaortitis in relation to AAV diagnosis.
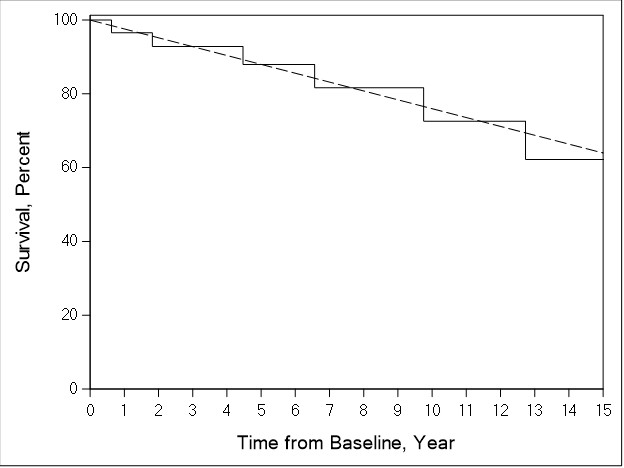
Figure 2. Overall survival of patients with L-AAV compared to expected rates from United States total lifetables (observed: solid line; expected: dashed line).
M. Kaymakci: None; M. Elfishawi: None; H. Langenfeld: None; A. Hanson: None; C. Crowson: None; M. Bois: None; U. Ghaffar: None; U. Specks: Amgen, 2, AstraZeneca, 2, 5, Boehringer-Ingelheim, 1, Bristol-Myers Squibb(BMS), 5, ChemoCentryx, 2, Genentech, 5, GlaxoSmithKlein(GSK), 5; M. Koster: None; K. Warrington: Bristol-Myers Squibb(BMS), 5, Chemocentryx, 1, 6, Eli Lilly, 5, kiniksa, 5.



