Poster Session B
Vasculitis
Session: (1554–1578) Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
1556: Abdominal Surgical Interventions Among Patients with Gastrointestinal Involvement of Behçet Syndrome
Monday, November 13, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- SE
Sinem Esatoglu, MD
Istanbul University-Cerrahpasa, Cerrahpasa Medical Faculty, Department of Internal Medicine, Division of Rheumatology
İstanbul, TurkeyDisclosure information not submitted.
Abstract Poster Presenter(s)
Sinem Nihal Esatoglu1, Sabriye Guner1, Sevim Guler2, Gulen Hatemi1, Nuray Kepil3, Yusuf Ziya Erzin4, Aykut Ferhat Celik4 and Ibrahim Hatemi4, 1Istanbul University-Cerrahpasa, Cerrahpasa Medical School, Department of Internal Medicine, Division of Rheumatology, Istanbul, Turkey, 2Istanbul University-Cerrahpasa, Cerrahpasa Medical School, Istanbul, Turkey, 3Istanbul University-Cerrahpasa, Cerrahpasa Medical School, Department of Pathology, Istanbul, Turkey, 4Istanbul University-Cerrahpasa, Cerrahpasa Medical School, Department of Internal Medicine, Division of Gastroenterology, Istanbul, Turkey
Background/Purpose: Gastrointestinal involvement of Behçet's syndrome (GIBS) may require surgery in up to one third of the patients. We aimed to investigate the clinical characteristics, treatments, and long-term prognosis of GIBS patients who underwent abdominal surgical interventions.
Methods: We conducted a retrospective chart review of all Behçet syndrome (BS) patients recorded between 1978 and 2022 to identify those with GIBS who had undergone abdominal surgery for GIBS. Data were collected regarding demographics, type of interventions, treatment, recurrences, and outcomes. Relapse was defined as the presence of endoscopic or clinical activity with a positive fecal calprotectin test following bowel resection.
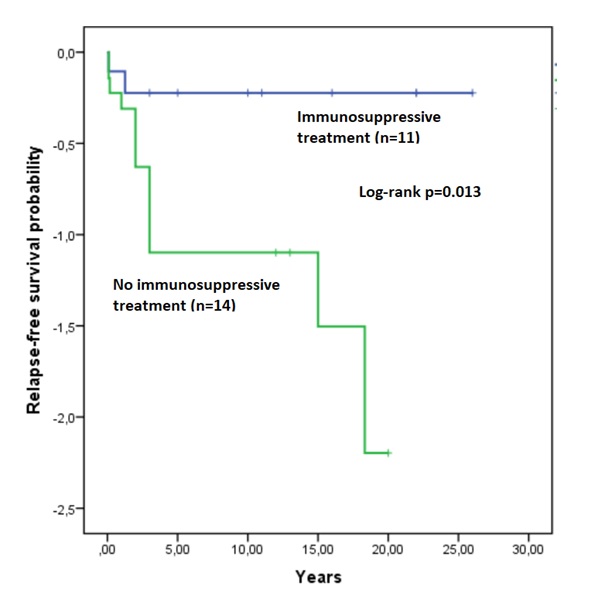
Results: Among our 11,200 BS patients, 119 (1%) had GIBS, and 27 (24%) of these GIBS patients (19 male, mean age: 49 ± 11 years) had undergone abdominal surgery (Table). BS was already diagnosed at the time of gastrointestinal involvement in 19 (65%) patients while 10 were diagnosed with BS with the development of gastrointestinal involvement. All except 1 patient who underwent ileocecal resection due to refractory disease, were diagnosed with GIBS following abdominal surgery. Perforation (n=18, 62%) and massive hematochezia (n=6, 21%) were the main reasons for surgery. The type of surgery was bowel resection in 25 patients, primary closure in 2 and diagnostic laparotomy in 2 patients. Two patients with refractory GIBS had died due to extensive vascular involvement (n=1) and secondary amyloidosis (n=1). Among the 25 patients who underwent bowel resection, 14 (56%) experienced a relapse during a median follow-up of 24 (IQR: 1.75-36) months. Of these 14 patients, 12 had only one relapse. At the time of relapse, 4 (29%) patients required a reoperation. The remaining 11 patients did not experience any relapses during a median follow-up of 13 (IQR: 10-22) months. Postoperative azathioprine treatment was initiated in 11 patients, with 3 of them also receiving a TNF inhibitor. Three of these 11 patients experienced a relapse while among the 14 patients who did not receive postoperative immunosuppressive treatment, 11 had a relapse (27% vs 79%; p=0.01). The use of postoperative immunosuppressive treatment was associated with a reduced risk of relapse (OR: 0.10; 95% CI: 0.016-0.644). Moreover, time to relapse was significantly longer in patients who received postoperative immunosuppressive treatment compared to those who did not (p=0.013, log-rank test, Figure)
Conclusion: GIBS may presently acutely with perforation or severe bleeding requiring surgery, as the first manifestation. In this cohort 24% of GIBS patients required abdominal surgery and all except one were diagnosed with GIBS following the surgical procedure. Approximately 50% of the patients experienced a relapse, with most relapses occurring within 3 years. Among the patients who relapsed, 30% required reoperation. The use of immunosuppressive treatment after surgery showed a significant protective effect, reducing the risk of relapse by 90%.
.jpg)
S. Esatoglu: None; S. Guner: None; S. Guler: None; G. Hatemi: None; N. Kepil: None; Y. Erzin: None; A. Celik: None; I. Hatemi: None.
Background/Purpose: Gastrointestinal involvement of Behçet's syndrome (GIBS) may require surgery in up to one third of the patients. We aimed to investigate the clinical characteristics, treatments, and long-term prognosis of GIBS patients who underwent abdominal surgical interventions.
Methods: We conducted a retrospective chart review of all Behçet syndrome (BS) patients recorded between 1978 and 2022 to identify those with GIBS who had undergone abdominal surgery for GIBS. Data were collected regarding demographics, type of interventions, treatment, recurrences, and outcomes. Relapse was defined as the presence of endoscopic or clinical activity with a positive fecal calprotectin test following bowel resection.
Results: Among our 11,200 BS patients, 119 (1%) had GIBS, and 27 (24%) of these GIBS patients (19 male, mean age: 49 ± 11 years) had undergone abdominal surgery (Table). BS was already diagnosed at the time of gastrointestinal involvement in 19 (65%) patients while 10 were diagnosed with BS with the development of gastrointestinal involvement. All except 1 patient who underwent ileocecal resection due to refractory disease, were diagnosed with GIBS following abdominal surgery. Perforation (n=18, 62%) and massive hematochezia (n=6, 21%) were the main reasons for surgery. The type of surgery was bowel resection in 25 patients, primary closure in 2 and diagnostic laparotomy in 2 patients. Two patients with refractory GIBS had died due to extensive vascular involvement (n=1) and secondary amyloidosis (n=1). Among the 25 patients who underwent bowel resection, 14 (56%) experienced a relapse during a median follow-up of 24 (IQR: 1.75-36) months. Of these 14 patients, 12 had only one relapse. At the time of relapse, 4 (29%) patients required a reoperation. The remaining 11 patients did not experience any relapses during a median follow-up of 13 (IQR: 10-22) months. Postoperative azathioprine treatment was initiated in 11 patients, with 3 of them also receiving a TNF inhibitor. Three of these 11 patients experienced a relapse while among the 14 patients who did not receive postoperative immunosuppressive treatment, 11 had a relapse (27% vs 79%; p=0.01). The use of postoperative immunosuppressive treatment was associated with a reduced risk of relapse (OR: 0.10; 95% CI: 0.016-0.644). Moreover, time to relapse was significantly longer in patients who received postoperative immunosuppressive treatment compared to those who did not (p=0.013, log-rank test, Figure)
Conclusion: GIBS may presently acutely with perforation or severe bleeding requiring surgery, as the first manifestation. In this cohort 24% of GIBS patients required abdominal surgery and all except one were diagnosed with GIBS following the surgical procedure. Approximately 50% of the patients experienced a relapse, with most relapses occurring within 3 years. Among the patients who relapsed, 30% required reoperation. The use of immunosuppressive treatment after surgery showed a significant protective effect, reducing the risk of relapse by 90%.
.jpg)
Table. Demographic and characteristics of the patients
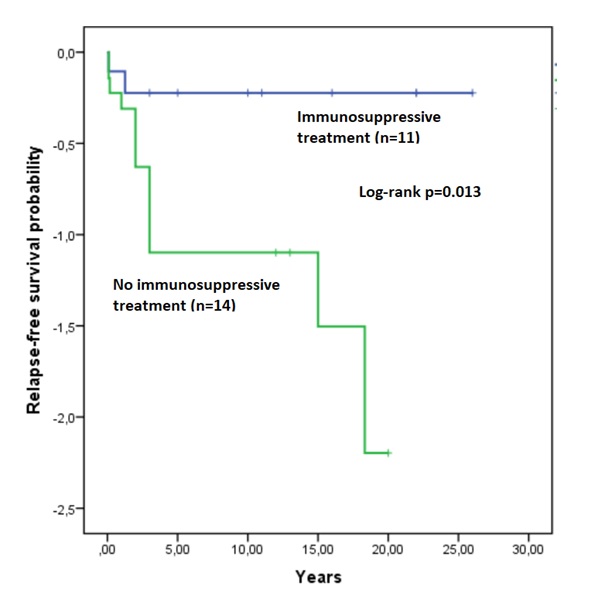
Figure. Relapse-free survival of patients who used postoperative immunosuppressive vs who did not
S. Esatoglu: None; S. Guner: None; S. Guler: None; G. Hatemi: None; N. Kepil: None; Y. Erzin: None; A. Celik: None; I. Hatemi: None.



