Poster Session B
Vasculitis
Session: (1554–1578) Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
1574: The Role of 18F-FDG PET/CT Scans in Takayasu Arteritis
Monday, November 13, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- SS
Shirish Sangle, MD, MBBS
Guy's and St Thomas' Hospital NHS FoundationTrust
London, United KingdomDisclosure information not submitted.
Abstract Poster Presenter(s)
Sahil Jain1, Abdulrahman Khormi2, Marcela Munoz-Urbano3, Shirish Sangle1 and David D'Cruz4, 1Louise Coote Lupus Unit, Guy's and St Thomas' Hospital NHS Foundation Trust, London, United Kingdom, 2Prince Sattam University Medical College, Al-Kharj, Saudi Arabia, 3Clínica Imbanaco, Cali, Colombia, 4Guy’s Hospital, Louise Coote Lupus Unit, London, United Kingdom
Background/Purpose: Takayasu arteritis (TA) is a large-vessel vasculitis which primarily affects the aorta and its main branches. Accurate assessment of disease activity has always been challenging and inadequate treatment may result in irreversible damage. The Indian Takayasu Clinical Arteritis Scores (ITAS 2010, ITAS.A) are validated and reliable measures of disease activity. Positron-emission tomography (PET) and 18F-FDG PET with computed tomography (PET/CT) are non-invasive metabolic imaging modalities that have been proposed as important tools to assess disease activity.
Methods: We retrospectively studied 26 TA patients between January 2008 – March 2023. The diagnosis was confirmed on clinical, laboratory and imaging criteria. Disease activity as assessed by the ITAS 2010, clinical, laboratory and imaging techniques (including magnetic resonance imaging, Doppler ultrasound and/or digital subtraction angiography) was compared with the results of the PET/CT scans.
Results: Median age at TA diagnosis was 33 years (13-57). There were 22 females (84.6%), 4 males and Caucasians (61.5%), Asians (30.8%) and Afro-Caribbean (7.7%). Median follow up was 156 months (20 – 444). Thirteen of 26 patients (50%) had positive antiphospholipid antibodies (aPL). Two of the patients were diagnosed with obstetric anti-phospholipid syndrome (APS) and 1 with both thrombotic and obstetric APS.
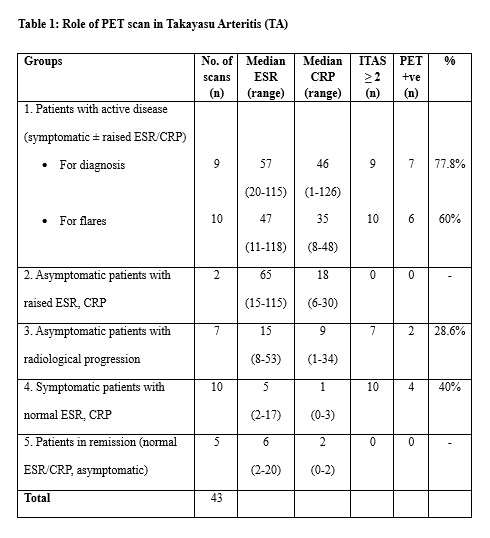
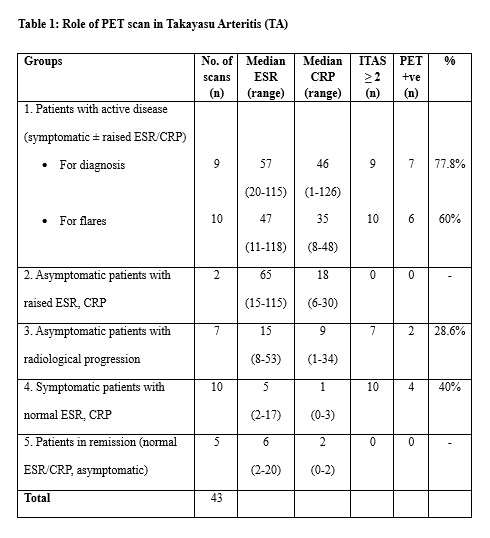
Of 26 patients, there were 43 PET/CT scans performed in 22 patients. Ten patients had a single scan and 12 patients had 2 or more scans (maximum 4 scans). Nine scans were done for diagnosis and 34 during follow up. Of the 9 diagnostic scans, all 9 had clinically active disease (ITAS score ≥ 2), 8 (88.9%) had raised inflammatory markers (median ESR 57 (20 -115), median CRP 46 (1-126)) and 7 (77.8%) had a positive PET scan (suggestive of active vasculitis). Of the 34 follow up scans, 27 scans (in 17 patients) had clinically active disease (ITAS score ≥ 2) and 7 scans (in 6 patients) were in remission (ITAS score 0). Of the 27 scans with clinically active disease, 12 scans were positive (44.4%). In the remaining 15 scans, 11 (73.3%) were done while on steroids and/or immunosuppression (median prednisolone dose 5mg (2.5 - 10mg)). The 7 follow up scans in clinical remission and had no FDG uptake.
Conclusion: 18F-FDG PET/CT scanning is helpful as a diagnostic and monitoring tool to assess disease activity in TA. PET scan imaging correlates with ITAS activity. Corticosteroid therapy may negatively impact the PET scan result and results should be correlated carefully with clinical, laboratory and other radiological assessments. It remains unclear whether presence of aPL/APS is a clinically important association.
S. Jain: None; A. Khormi: None; M. Munoz-Urbano: None; S. Sangle: None; D. D'Cruz: Eli Lilly & Company, 2, GSK, 1, 2, UCB, 2, Vifor Pharma, 1.
Background/Purpose: Takayasu arteritis (TA) is a large-vessel vasculitis which primarily affects the aorta and its main branches. Accurate assessment of disease activity has always been challenging and inadequate treatment may result in irreversible damage. The Indian Takayasu Clinical Arteritis Scores (ITAS 2010, ITAS.A) are validated and reliable measures of disease activity. Positron-emission tomography (PET) and 18F-FDG PET with computed tomography (PET/CT) are non-invasive metabolic imaging modalities that have been proposed as important tools to assess disease activity.
Methods: We retrospectively studied 26 TA patients between January 2008 – March 2023. The diagnosis was confirmed on clinical, laboratory and imaging criteria. Disease activity as assessed by the ITAS 2010, clinical, laboratory and imaging techniques (including magnetic resonance imaging, Doppler ultrasound and/or digital subtraction angiography) was compared with the results of the PET/CT scans.
Results: Median age at TA diagnosis was 33 years (13-57). There were 22 females (84.6%), 4 males and Caucasians (61.5%), Asians (30.8%) and Afro-Caribbean (7.7%). Median follow up was 156 months (20 – 444). Thirteen of 26 patients (50%) had positive antiphospholipid antibodies (aPL). Two of the patients were diagnosed with obstetric anti-phospholipid syndrome (APS) and 1 with both thrombotic and obstetric APS.
Of 26 patients, there were 43 PET/CT scans performed in 22 patients. Ten patients had a single scan and 12 patients had 2 or more scans (maximum 4 scans). Nine scans were done for diagnosis and 34 during follow up. Of the 9 diagnostic scans, all 9 had clinically active disease (ITAS score ≥ 2), 8 (88.9%) had raised inflammatory markers (median ESR 57 (20 -115), median CRP 46 (1-126)) and 7 (77.8%) had a positive PET scan (suggestive of active vasculitis). Of the 34 follow up scans, 27 scans (in 17 patients) had clinically active disease (ITAS score ≥ 2) and 7 scans (in 6 patients) were in remission (ITAS score 0). Of the 27 scans with clinically active disease, 12 scans were positive (44.4%). In the remaining 15 scans, 11 (73.3%) were done while on steroids and/or immunosuppression (median prednisolone dose 5mg (2.5 - 10mg)). The 7 follow up scans in clinical remission and had no FDG uptake.
Conclusion: 18F-FDG PET/CT scanning is helpful as a diagnostic and monitoring tool to assess disease activity in TA. PET scan imaging correlates with ITAS activity. Corticosteroid therapy may negatively impact the PET scan result and results should be correlated carefully with clinical, laboratory and other radiological assessments. It remains unclear whether presence of aPL/APS is a clinically important association.
S. Jain: None; A. Khormi: None; M. Munoz-Urbano: None; S. Sangle: None; D. D'Cruz: Eli Lilly & Company, 2, GSK, 1, 2, UCB, 2, Vifor Pharma, 1.



