Poster Session B
Reproductive health
Session: (1345–1364) Reproductive Issues in Rheumatic Disorders Poster II
1364: Both Low and High 25(OH)-Vitamin D Levels Increase Adverse Pregnancy Outcomes in Systemic Lupus Erythematosus
Monday, November 13, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- NM
Nima Madanchi, MD
Johns Hopkins University
Baltimore, MD, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Nima Madanchi1, Andrea Fava2, Daniel Goldman3, Larry Magder4, Rebecca Jacobson1 and Michelle Petri3, 1Johns Hopkins University School of Medicine, Baltimore, MD, 2Johns Hopkins University, Baltimore, MD, 3Department of Medicine, Division of Rheumatology, Johns Hopkins University School of Medicine, Timonium, MD, 4University of Maryland, Baltimore, MD
Background/Purpose: We evaluated the role of maternal 25(OH)-vitamin D in adverse pregnancy outcomes in systemic lupus erythematosus (SLE).
Methods: We used a longitudinal cohort that included visits of pregnant patients with assessment of 25(OH)-vitamin D at each visit. Pregnancies were excluded if there was no vitamin D level during pregnancy, if the outcomes of pregnancies were missing (such as data on due date, birth date, gestational age, and complications of pregnancies), or if the pregnancy was terminated. 270 pregnancies were available for the statistical analysis.
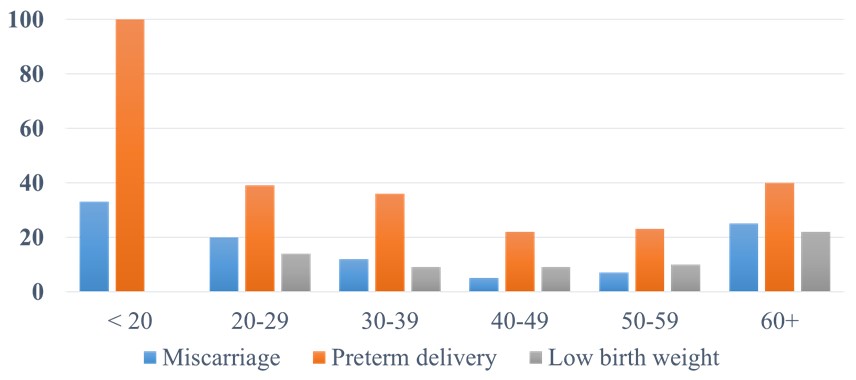
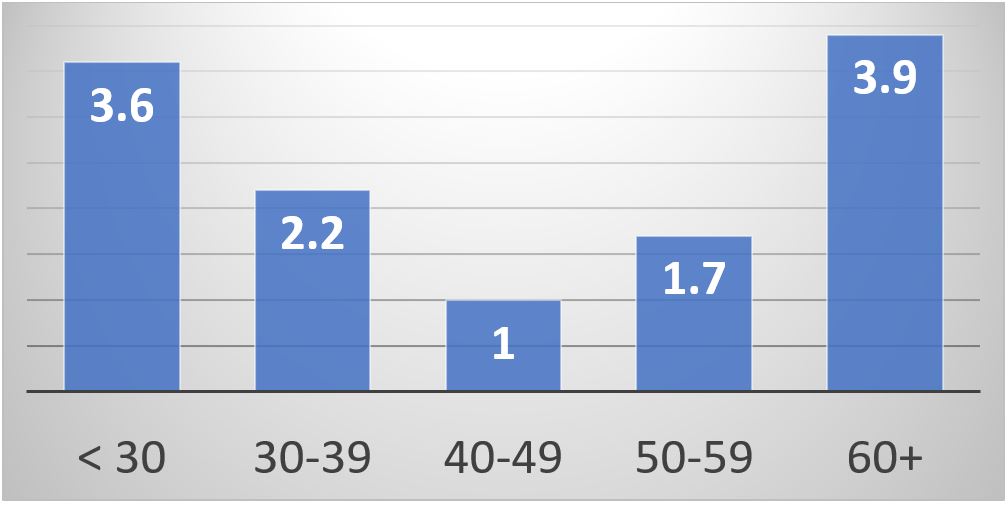
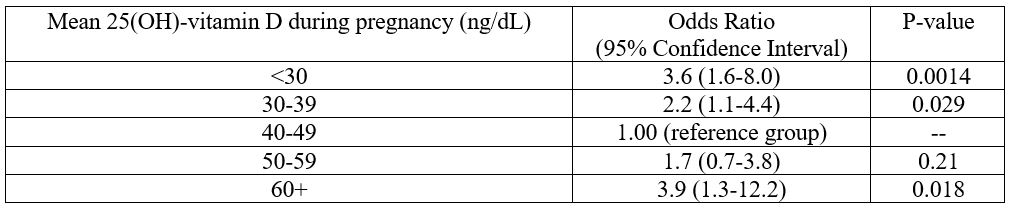
Results: We found a U-shape association between the maternal serum 25(OH)-vitamin D level and the combined adverse pregnancy outcomes (P=0.0022), miscarriage (P=0.0048), and preterm delivery (P=0.0003). We also found the same U-shape curve with the low birth weight; but it did not reach statistical significance due to the smaller number of cases. The lowest prevalence of adverse pregnancy outcomes was with 25(OH)-vitamin D in the range of 40-59 ng/dL (Figure 1). The multivariate analysis confirmed the same U-shape association controlling for age, race, and antiphospholipid antibodies (Table 1, Figure 2). The results were similar when we examined the subset in which pre-pregnancy or first trimester BMI were available.
Conclusion: Our study design cannot prove a cause-and-effect relationship. Most of our patients were prescribed vitamin D supplementation (but obviously many did not take it). We recommend monitoring 25(OH)-vitamin D levels during SLE pregnancies. The ideal 25(OH)-vitamin D range was 40-59 ng/dL.
N. Madanchi: None; A. Fava: Annexon Biosciences, 2, Sanofi, 1; D. Goldman: None; L. Magder: None; R. Jacobson: None; M. Petri: Alexion, 1, Amgen, 1, AnaptysBio, 1, Annexon Bio, 1, Argenx, 1, Arhros-Focus Med/Ed, 6, AstraZeneca, 1, 5, Aurinia, 1, 5, 6, Axdev, 1, Biogen, 1, Boxer Capital, 2, Cabaletto Bio, 2, Caribou Biosciences, 2, CVS Health, 1, Eli Lilly, 1, 5, Emergent Biosolutions, 1, Exagen, 5, Exo Therapeutics, 2, Gilead Biosciences, 2, GlaxoSmithKlein(GSK), 1, 5, 6, Horizon Therapeutics, 2, Idorsia Pharmaceuticals, 2, IQVIA, 1, Janssen, 1, 5, Kira Pharmaceuticals, 2, MedShr, 6, Merck/EMD Serono, 1, Momenta Pharmaceuticals, 2, Nexstone Immunology, 2, Nimbus Lakshmi, 2, Proviant, 2, Sanofi, 2, Sinomab Biosciences, 2, Thermofisher, 5, UCB, 2.
Background/Purpose: We evaluated the role of maternal 25(OH)-vitamin D in adverse pregnancy outcomes in systemic lupus erythematosus (SLE).
Methods: We used a longitudinal cohort that included visits of pregnant patients with assessment of 25(OH)-vitamin D at each visit. Pregnancies were excluded if there was no vitamin D level during pregnancy, if the outcomes of pregnancies were missing (such as data on due date, birth date, gestational age, and complications of pregnancies), or if the pregnancy was terminated. 270 pregnancies were available for the statistical analysis.
Results: We found a U-shape association between the maternal serum 25(OH)-vitamin D level and the combined adverse pregnancy outcomes (P=0.0022), miscarriage (P=0.0048), and preterm delivery (P=0.0003). We also found the same U-shape curve with the low birth weight; but it did not reach statistical significance due to the smaller number of cases. The lowest prevalence of adverse pregnancy outcomes was with 25(OH)-vitamin D in the range of 40-59 ng/dL (Figure 1). The multivariate analysis confirmed the same U-shape association controlling for age, race, and antiphospholipid antibodies (Table 1, Figure 2). The results were similar when we examined the subset in which pre-pregnancy or first trimester BMI were available.
Conclusion: Our study design cannot prove a cause-and-effect relationship. Most of our patients were prescribed vitamin D supplementation (but obviously many did not take it). We recommend monitoring 25(OH)-vitamin D levels during SLE pregnancies. The ideal 25(OH)-vitamin D range was 40-59 ng/dL.
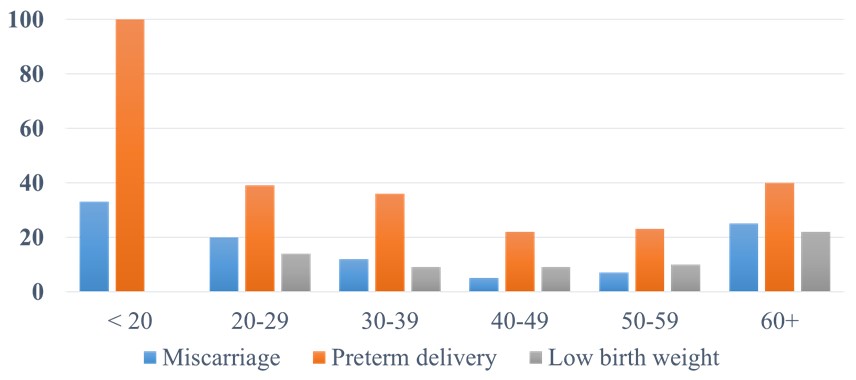
Figure 1. Adverse pregnancy outcomes occurrence (%) by mean 25(OH)-vitamin D (ng/dL) during pregnancy.
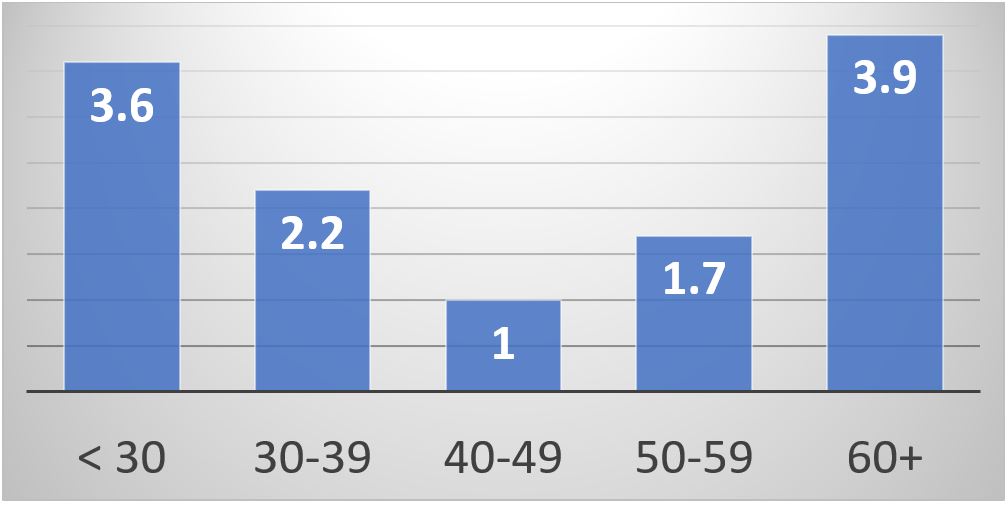
Figure 2. Odds ratios of combined adverse pregnancy outcomes with different mean 25(OH)-vitamin D levels controlling for age, race, and antiphospholipid antibodies.
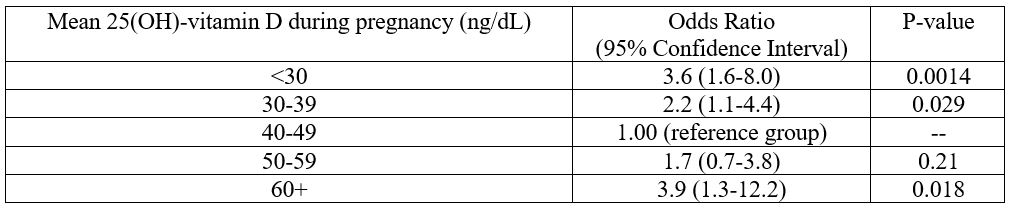
Table 1. Odds ratios of adverse pregnancy outcomes with different mean maternal 25(OH)-vitamin D levels controlling for age, race, and antiphospholipid antibodies.
N. Madanchi: None; A. Fava: Annexon Biosciences, 2, Sanofi, 1; D. Goldman: None; L. Magder: None; R. Jacobson: None; M. Petri: Alexion, 1, Amgen, 1, AnaptysBio, 1, Annexon Bio, 1, Argenx, 1, Arhros-Focus Med/Ed, 6, AstraZeneca, 1, 5, Aurinia, 1, 5, 6, Axdev, 1, Biogen, 1, Boxer Capital, 2, Cabaletto Bio, 2, Caribou Biosciences, 2, CVS Health, 1, Eli Lilly, 1, 5, Emergent Biosolutions, 1, Exagen, 5, Exo Therapeutics, 2, Gilead Biosciences, 2, GlaxoSmithKlein(GSK), 1, 5, 6, Horizon Therapeutics, 2, Idorsia Pharmaceuticals, 2, IQVIA, 1, Janssen, 1, 5, Kira Pharmaceuticals, 2, MedShr, 6, Merck/EMD Serono, 1, Momenta Pharmaceuticals, 2, Nexstone Immunology, 2, Nimbus Lakshmi, 2, Proviant, 2, Sanofi, 2, Sinomab Biosciences, 2, Thermofisher, 5, UCB, 2.



