Poster Session B
Vasculitis
Session: (1534–1553) Vasculitis – ANCA-Associated Poster II: Epidemiology, Outcomes, & Classification
1553: Central Nervous System Involvement and Mimickers in ANCA Associated Vasculitis
Monday, November 13, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- SE
Sinem Esatoglu, MD
Istanbul University-Cerrahpasa, Cerrahpasa Medical Faculty, Department of Internal Medicine, Division of Rheumatology
İstanbul, TurkeyDisclosure information not submitted.
Abstract Poster Presenter(s)
Yeliz Yagiz Ozogul1, Sinem Nihal Esatoglu2, Murat Ozogul3, Osman Kizilkilic4, Yesim Ozguler5, Ugur Uygunoglu6, Vedat Hamuryudan2 and Gulen Hatemi2, 1Istanbul University-Cerrahpasa, Cerrahpasa Medical School, Department of Internal Medicine, Istanbul, Turkey, 2Istanbul University-Cerrahpasa, Cerrahpasa Medical School, Department of Internal Medicine, Division of Rheumatology, Istanbul, Turkey, 3Haydarpasa Numune Training and Research Hospital, Department of Radiology, Istanbul, Turkey, 4Istanbul University-Cerrahpasa, Cerrahpasa Medical School, Department of Radiology, Istanbul, Turkey, 5Istanbul University-Cerrahpasa, Cerrahpasa Medical School, Department of Internal Medicine, Division of Rheumatology, İstanbul, Turkey, 6Istanbul University-Cerrahpasa, Cerrahpasa Medical School, Department of Neurology, Istanbul, Turkey
Background/Purpose: Central nervous system (CNS) involvement is rare in ANCA associated vasculitis (AAV). On the other hand, AAV patients may develop complications or other conditions that mimic CNS involvement. We aimed to present the clinical, laboratory and imaging features of our AAV patients with CNS involvement and conditions other than CNS involvement that caused neurologic symptoms.
Methods: We surveyed the charts of 430 AAV patients in order to identify patients who were evaluated for neurologic symptoms suggesting CNS involvement. We extracted data on their demographics, types of AAV, neurologic symptoms, final diagnoses after neurologic work-up and their outcome.
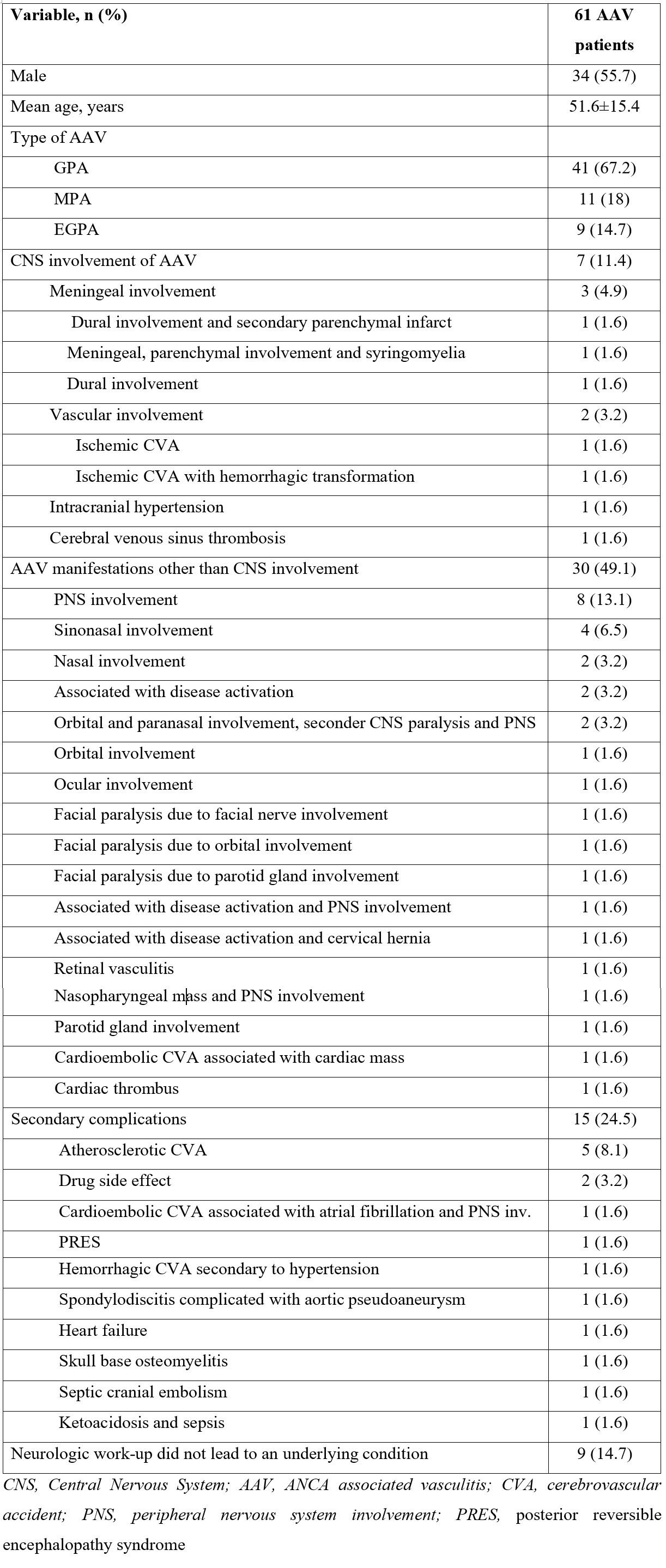
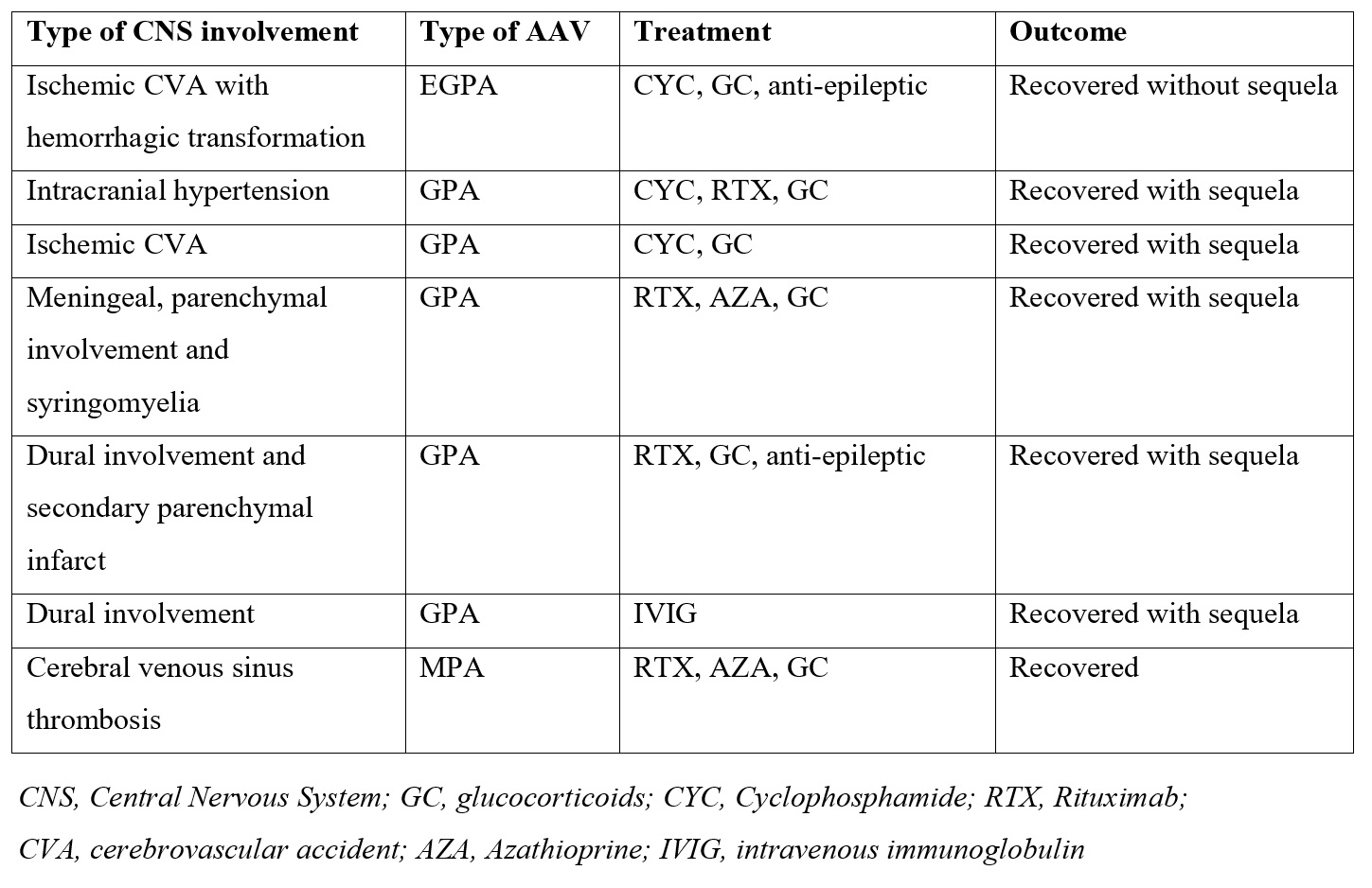
Results: Of 430 AAV patients, 61 patients (14%) (41 GPA, 11 MPA, 9 EGPA; 27 women, 34 men; mean age: 51.6±15.4) with neurologic symptoms were identified. Among these, the cause of neurologic symptoms was CNS involvement of AAV in 7 patients (data summarized in Table 1), other AAV manifestations in 30, and secondary complications mimicking CNS involvement in 15 patients, whereas neurologic work-up did not lead to an underlying condition in 9 (Table 2). Among the 61 AAV patients with neurologic symptoms, the most common neurologic symptom suggesting CNS involvement was headache (n=20), followed by muscle weakness (n=17), numbness (n=17), and visual impairment (n=16). At the time of the occurrence of neurologic symptoms, all patients had active disease [median (IQR) BVAS=11.9 (7-15)]. 14 patients (22.9%) had accompanying peripheral nervous system (PNS) involvement. Regarding the outcomes, 6 of the 7 patients with CNS involvement of AAV recovered with sequelae, whereas one patient completely recovered. Among the 30 patients with other AAV manifestations causing neurologic symptoms, 21 recovered without sequela while the remaining 9 recovered with sequela despite treatment. Finally, among the 15 patients with conditions mimicking CNS involvement of AAV, one patient with spondylodiscitiscomplicated with aortic pseudoaneurysm, one with septic emboli and one with diabetic ketoacidosis complicated with pneumosepsis had died, one patient withskull base osteomyelitis recovered with a sequela of blindness, and the remaining patients recovered without sequela.
Conclusion: CNS involvement was uncommon, observed in only 1.6% of our 430 AAV patients. AAV manifestations other than CNS involvement such as ocular, orbital and nasopharyngeal involvement, as well as complications like infections and cardiovascular disease, may mimic CNS involvement in patients with AAV. These non-CNS entities account for almost 75% of the causes for any neurological symptom among AAV patients.
Y. Yagiz Ozogul: None; S. Esatoglu: None; M. Ozogul: None; O. Kizilkilic: None; Y. Ozguler: None; U. Uygunoglu: None; V. Hamuryudan: None; G. Hatemi: None.
Background/Purpose: Central nervous system (CNS) involvement is rare in ANCA associated vasculitis (AAV). On the other hand, AAV patients may develop complications or other conditions that mimic CNS involvement. We aimed to present the clinical, laboratory and imaging features of our AAV patients with CNS involvement and conditions other than CNS involvement that caused neurologic symptoms.
Methods: We surveyed the charts of 430 AAV patients in order to identify patients who were evaluated for neurologic symptoms suggesting CNS involvement. We extracted data on their demographics, types of AAV, neurologic symptoms, final diagnoses after neurologic work-up and their outcome.
Results: Of 430 AAV patients, 61 patients (14%) (41 GPA, 11 MPA, 9 EGPA; 27 women, 34 men; mean age: 51.6±15.4) with neurologic symptoms were identified. Among these, the cause of neurologic symptoms was CNS involvement of AAV in 7 patients (data summarized in Table 1), other AAV manifestations in 30, and secondary complications mimicking CNS involvement in 15 patients, whereas neurologic work-up did not lead to an underlying condition in 9 (Table 2). Among the 61 AAV patients with neurologic symptoms, the most common neurologic symptom suggesting CNS involvement was headache (n=20), followed by muscle weakness (n=17), numbness (n=17), and visual impairment (n=16). At the time of the occurrence of neurologic symptoms, all patients had active disease [median (IQR) BVAS=11.9 (7-15)]. 14 patients (22.9%) had accompanying peripheral nervous system (PNS) involvement. Regarding the outcomes, 6 of the 7 patients with CNS involvement of AAV recovered with sequelae, whereas one patient completely recovered. Among the 30 patients with other AAV manifestations causing neurologic symptoms, 21 recovered without sequela while the remaining 9 recovered with sequela despite treatment. Finally, among the 15 patients with conditions mimicking CNS involvement of AAV, one patient with spondylodiscitiscomplicated with aortic pseudoaneurysm, one with septic emboli and one with diabetic ketoacidosis complicated with pneumosepsis had died, one patient withskull base osteomyelitis recovered with a sequela of blindness, and the remaining patients recovered without sequela.
Conclusion: CNS involvement was uncommon, observed in only 1.6% of our 430 AAV patients. AAV manifestations other than CNS involvement such as ocular, orbital and nasopharyngeal involvement, as well as complications like infections and cardiovascular disease, may mimic CNS involvement in patients with AAV. These non-CNS entities account for almost 75% of the causes for any neurological symptom among AAV patients.
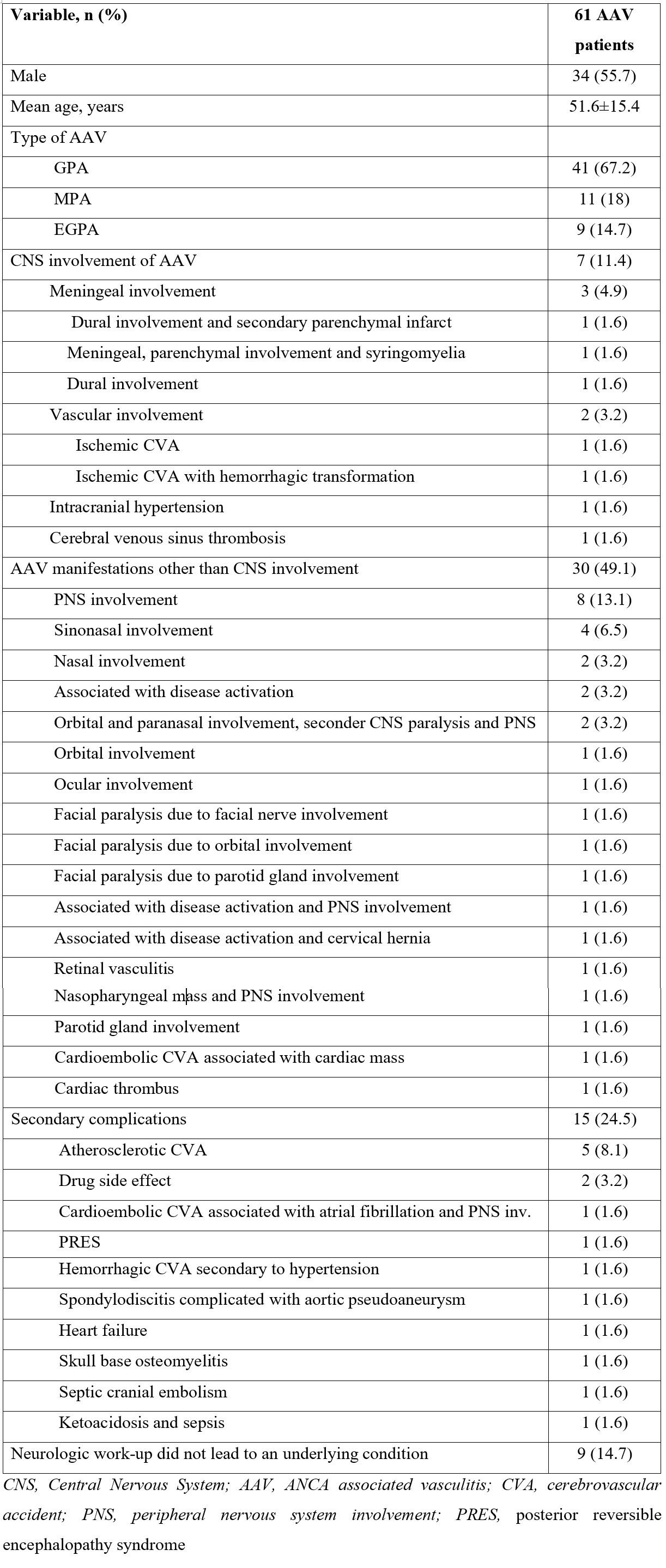
Table 1. Demographic features of the patients and causes for neurologic sign or symptoms
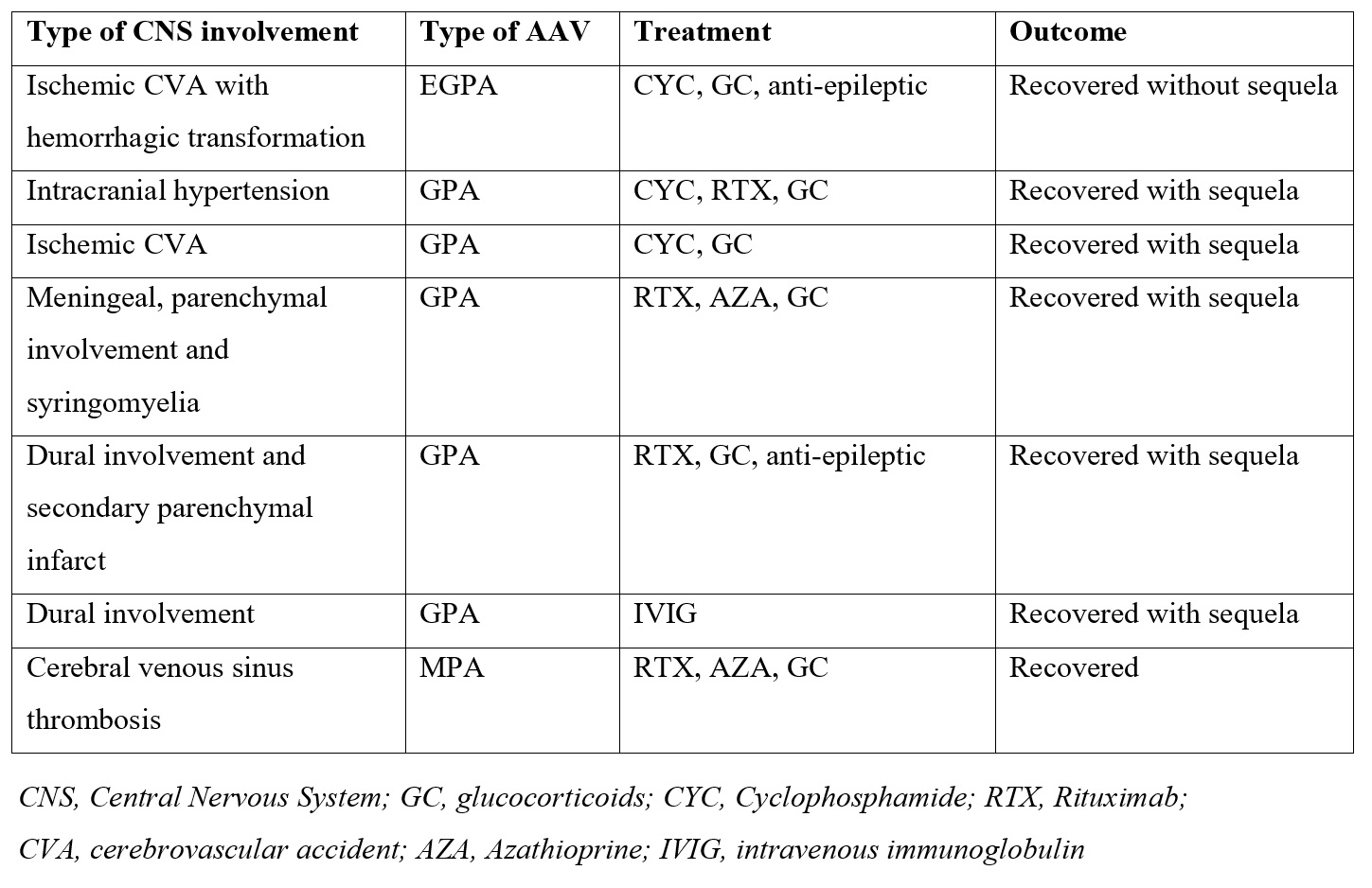
Table 2. Management and outcome of 7 AAV patients with CNS involvement
Y. Yagiz Ozogul: None; S. Esatoglu: None; M. Ozogul: None; O. Kizilkilic: None; Y. Ozguler: None; U. Uygunoglu: None; V. Hamuryudan: None; G. Hatemi: None.



