Poster Session B
Systemic lupus erythematosus (SLE)
Session: (1488–1512) SLE – Treatment Poster II
1506: Prescribing Patterns in Lupus Nephritis: Analyzing Time from Proteinuria to Prescription of ACE/ARB
Monday, November 13, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- JJ
Jacqueline Jansz, MD (she/her/hers)
University of Illinois at Chicago Hospital
Chicago, IL, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
JM JANSZ1, WL GALLANTER1, EM Adams2, Nadera Sweiss3 and Huan Chang4, 1University of Illinois at Chicago, Chicago, IL, 2Jesse Brown VA Medical Center, Chicago, IL, 3University of Illinois, Chicago, IL, 4University of Illinois at Chicago; Jesse Brown VA Medical Center, Chicago, IL
Background/Purpose: Black patients with lupus nephritis have worse renal outcomes compared with their White counterparts. Currently, there is a paucity of data evaluating the use of angiotensin-converting enzyme inhibitors (ACE) and angiotensin receptor blockers (ARB) in lupus patients with proteinuria despite their well-established benefits. The objective of this study was to examine the prescribing patterns of ACE/ARB in lupus patients with laboratory evidence of proteinuria, focusing on demographic factors such as race/ethnicity, gender and age.
Methods: The study population comprised patients seen in an urban academic medical center from January 1, 2000 through September 12, 2020 with at least one ambulatory encounter and a diagnosis code associated with either lupus or lupus nephritis. Proteinuria was defined according to the American College of Rheumatology (ACR) definition of renal disease, which includes a urine protein 3+ or above (300 mg/dL or greater), a urine protein creatinine ratio > 0.5, a 24-hour urine protein excretion greater than 0.5g, or a urine microalbumin/creatinine ratio greater than 50. The time interval from the first laboratory result indicating proteinuria in patients naive to an ACE/ARB to the day of ACE/ARB prescription was measured in days.
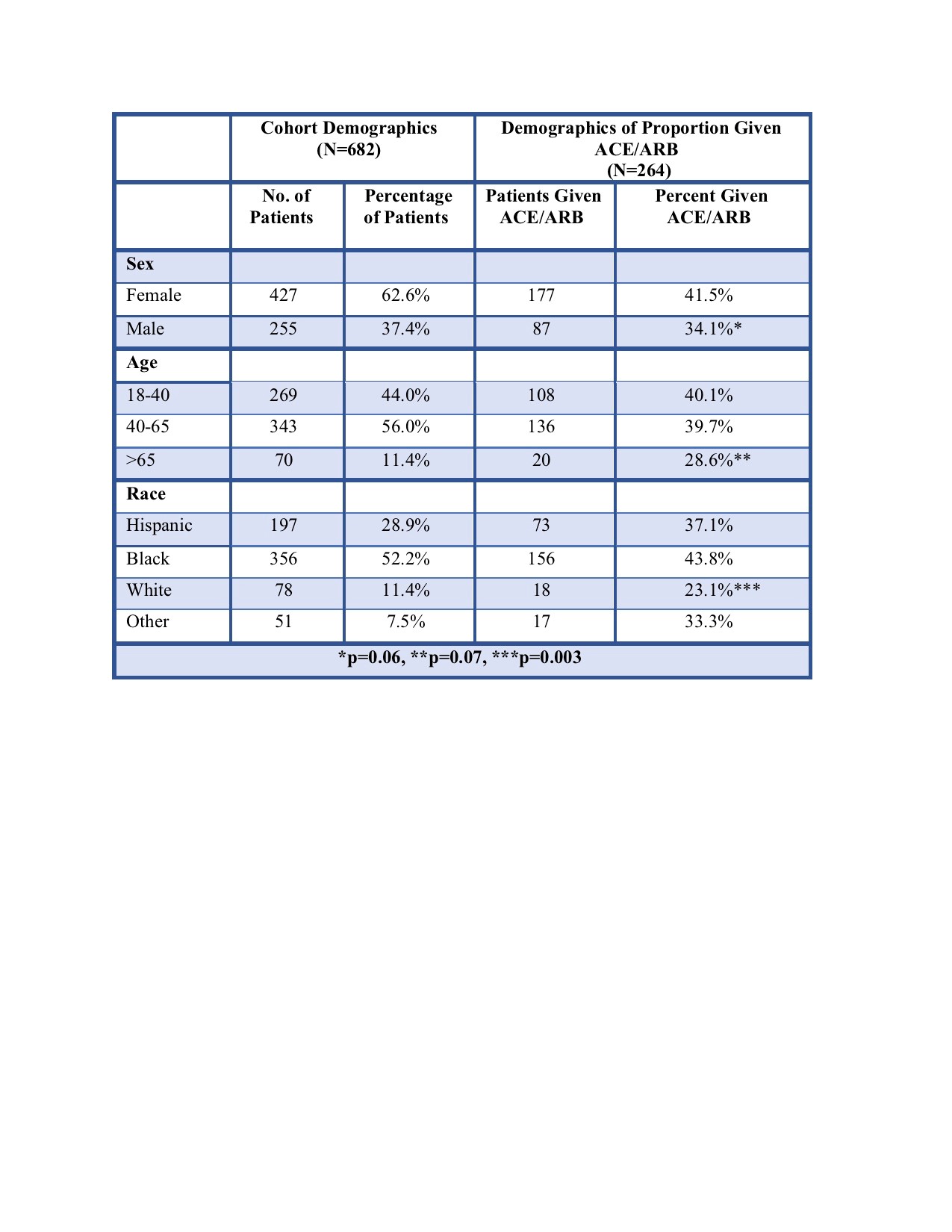
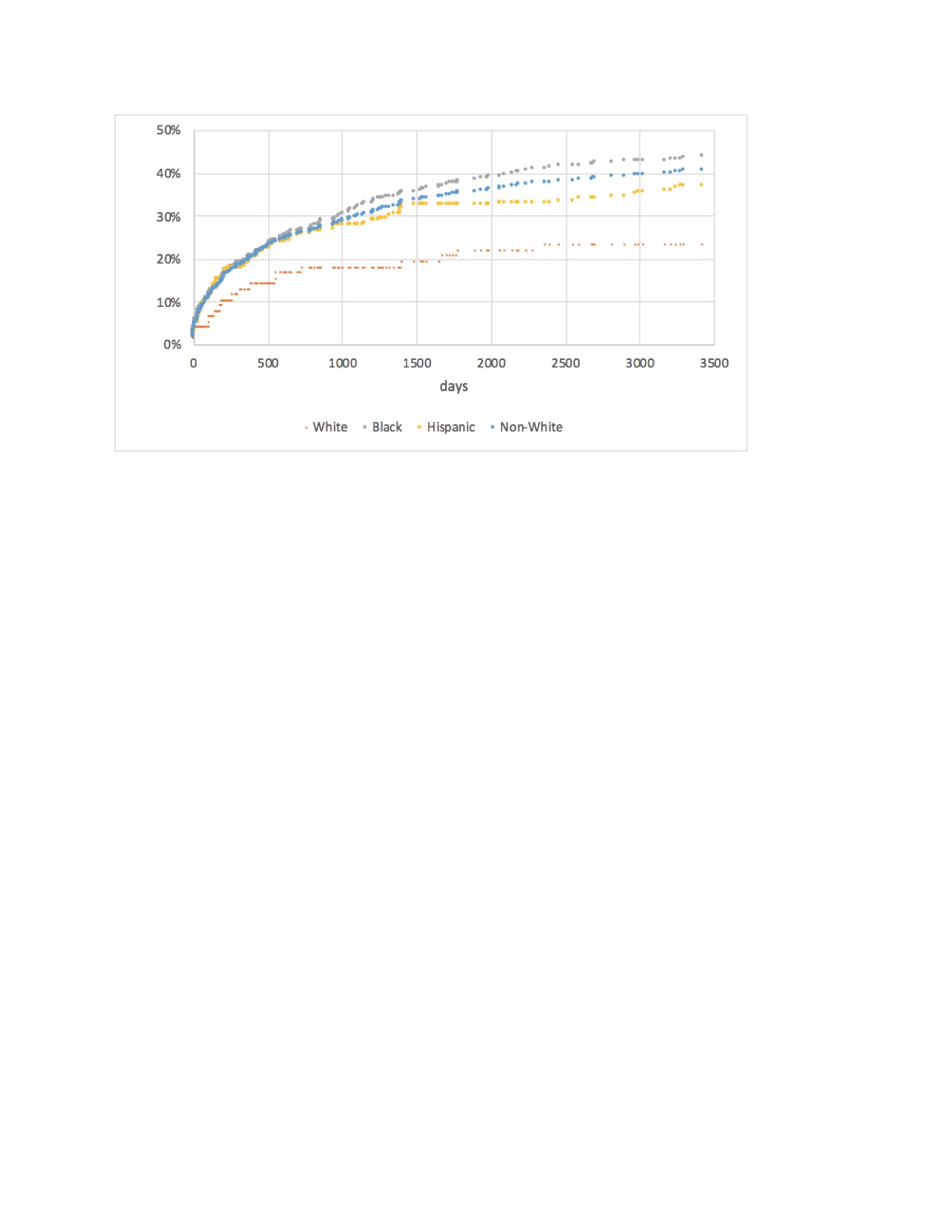
Results: Data show 39% of lupus patients with laboratory evidence of proteinuria were prescribed an ACE/ARB during the study time frame. For those who received a prescription, the median time from the detection of proteinuria to the prescription of an ACE/ARB was 382 days. Non-White patients (Black, Hispanic, and Other) were more frequently prescribed an ACE or an ARB compared with White patients (p=0.005). There was also a trend indicating higher prescription rates for female patients compared with male patients (p=0.06). There was a non-statistically significant reduction in prescription of ACE/ARB in patients greater than 65 years old.
Conclusion: Our study reveals a pattern of incomplete and delayed treatment of proteinuria with an ACE/ARB in lupus patients with evidence of proteinuria. Less than half of lupus patients with proteinuria received an ACE/ARB during the study timeframe, with Non-White patients significantly more likely to receive an ACE/ARB than White patients. The median time to ACE/ARB initiation was greater than a year. We intend to conduct further analysis to investigate hypertension as a potential confounding factor in the earlier initiation of an ACE/ARB among Non-White patients. Additionally, we plan to examine the time elapsed from proteinuria diagnosis to the prescription of immunosuppressive medications. These additional analyses will provide insight into optimizing timely evidence-based management of lupus nephritis patients.
J. JANSZ: None; W. GALLANTER: None; E. Adams: None; N. Sweiss: None; H. Chang: None.
Background/Purpose: Black patients with lupus nephritis have worse renal outcomes compared with their White counterparts. Currently, there is a paucity of data evaluating the use of angiotensin-converting enzyme inhibitors (ACE) and angiotensin receptor blockers (ARB) in lupus patients with proteinuria despite their well-established benefits. The objective of this study was to examine the prescribing patterns of ACE/ARB in lupus patients with laboratory evidence of proteinuria, focusing on demographic factors such as race/ethnicity, gender and age.
Methods: The study population comprised patients seen in an urban academic medical center from January 1, 2000 through September 12, 2020 with at least one ambulatory encounter and a diagnosis code associated with either lupus or lupus nephritis. Proteinuria was defined according to the American College of Rheumatology (ACR) definition of renal disease, which includes a urine protein 3+ or above (300 mg/dL or greater), a urine protein creatinine ratio > 0.5, a 24-hour urine protein excretion greater than 0.5g, or a urine microalbumin/creatinine ratio greater than 50. The time interval from the first laboratory result indicating proteinuria in patients naive to an ACE/ARB to the day of ACE/ARB prescription was measured in days.
Results: Data show 39% of lupus patients with laboratory evidence of proteinuria were prescribed an ACE/ARB during the study time frame. For those who received a prescription, the median time from the detection of proteinuria to the prescription of an ACE/ARB was 382 days. Non-White patients (Black, Hispanic, and Other) were more frequently prescribed an ACE or an ARB compared with White patients (p=0.005). There was also a trend indicating higher prescription rates for female patients compared with male patients (p=0.06). There was a non-statistically significant reduction in prescription of ACE/ARB in patients greater than 65 years old.
Conclusion: Our study reveals a pattern of incomplete and delayed treatment of proteinuria with an ACE/ARB in lupus patients with evidence of proteinuria. Less than half of lupus patients with proteinuria received an ACE/ARB during the study timeframe, with Non-White patients significantly more likely to receive an ACE/ARB than White patients. The median time to ACE/ARB initiation was greater than a year. We intend to conduct further analysis to investigate hypertension as a potential confounding factor in the earlier initiation of an ACE/ARB among Non-White patients. Additionally, we plan to examine the time elapsed from proteinuria diagnosis to the prescription of immunosuppressive medications. These additional analyses will provide insight into optimizing timely evidence-based management of lupus nephritis patients.
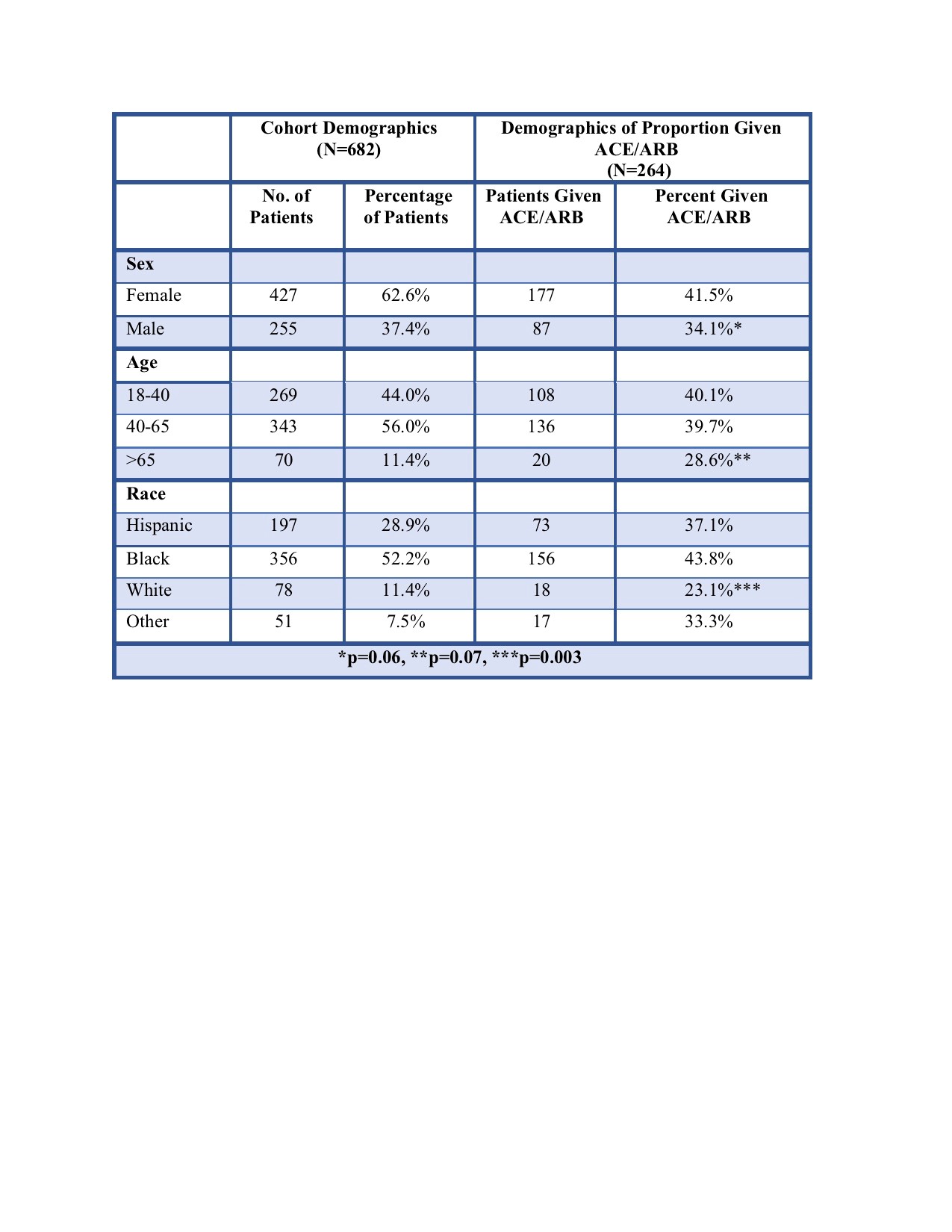
Table 1. Cohort and Treatment Cohort Demographics
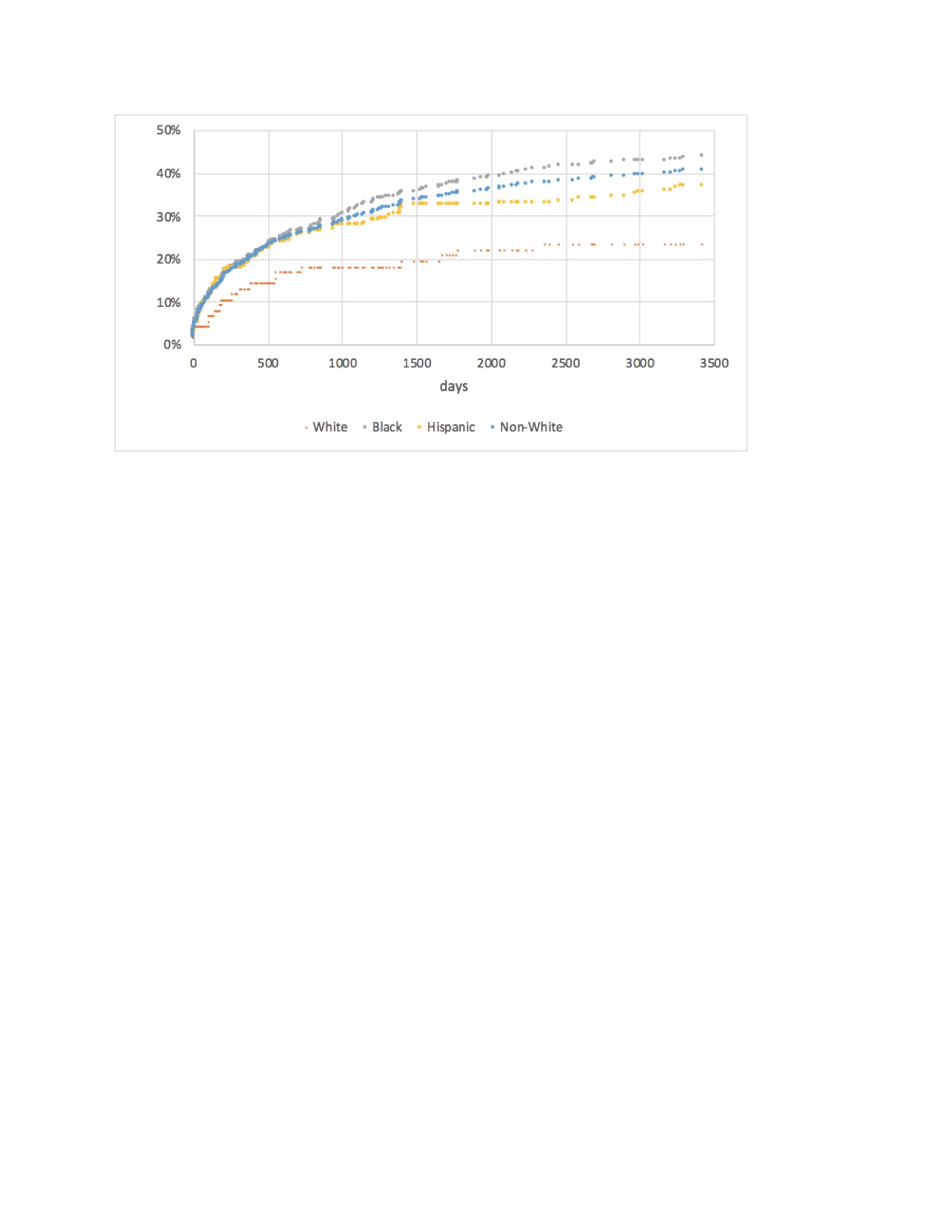
Figure 1. Percentage of Patients with Proteinuria Prescribed an ACE/ARB Over Time in Days
J. JANSZ: None; W. GALLANTER: None; E. Adams: None; N. Sweiss: None; H. Chang: None.



