Abstract Session
Epidemiology, health policy and outcomes
Session: Abstracts: Epidemiology & Public Health I (0739–0744)
0740: Renal Arteriosclerosis in Index Lupus Nephritis Biopsies Predicts Future Cardiovascular Disease
Sunday, November 12, 2023
2:15 PM - 2:25 PM PT
Location: Room 33A-C
- SG
Shivani Garg, MD, MS
University of Madison, School of Medicine and Public Health
Madison, WI, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Presenting Author(s)
Shivani Garg1, Brad Astor2, S. Sam Lim3, Amish Raval2, Weixiong Zhong2, Sarah Panzer2, Brad Rovin4 and Christie M. Bartels2, 1Department of Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI, 2University of Wisconsin, School of Medicine and Public Health, Madison, WI, 3Emory University, Atlanta, GA, 4Ohio State University, Columbus, OH
Background/Purpose: Patients < 40 years old with lupus nephritis (LN) face 42-fold higher risk of cardiovascular disease (CVD) compared to peers. Traditional CVD risk calculators fail to accurately predict future CVD risk in young LN patients, making decisions to prescribe empiric CVD prevention wrought with uncertainty. While a kidney biopsy is routinely performed to diagnose LN, renal arteriosclerosis (ASCL) is not routinely reported. Renal arteriosclerosis (ASCL) in kidney biopsies at LN diagnosis might represent changes in systemic arteries and could guide CVD risk stratification when most probably don't take this into account. Thus, in this study we systematically graded renal arteriosclerosis in kidney biopsies at LN diagnosis and examined its role as an early predictor of future incident CVD events.
Methods: Data were abstracted from adult LN patients who underwent diagnostic kidney biopsy between 1994-2021, including socio-demographics, traditional CVD risk factors, and pathology reports. Incident CVD-related deaths and non-fatal CVD events (ischemic heart disease, cerebrovascular accident, transient ischemic attack, and peripheral vascular disease) were adjudicated using published guidelines. Index standard of care kidney biopsies performed to diagnose LN were re-read by a pathologist to grade renal arteriosclerosis (ASCL) by calculating percent luminal narrowing of renal arteries using the Banff criteria. We examined the role of renal ASCL in diagnostic LN biopsies as an early predictor of future CVD using a Cox proportional hazards model in: a) all LN patients; b) those with preserved kidney function defined as chronic kidney disease stages 1-2.
Results: Among 173 adult patients with incident LN, 75% were female and 35% were of Black race or Hispanic ethnicity, and mean age at diagnosis was 38±17 years. Mean eGFR was 79±38 ml/min/1.73m2; 65% of patients had preserved kidney function. We noted 47% and 32% of patients had renal ASCL ≥15% and 25%.
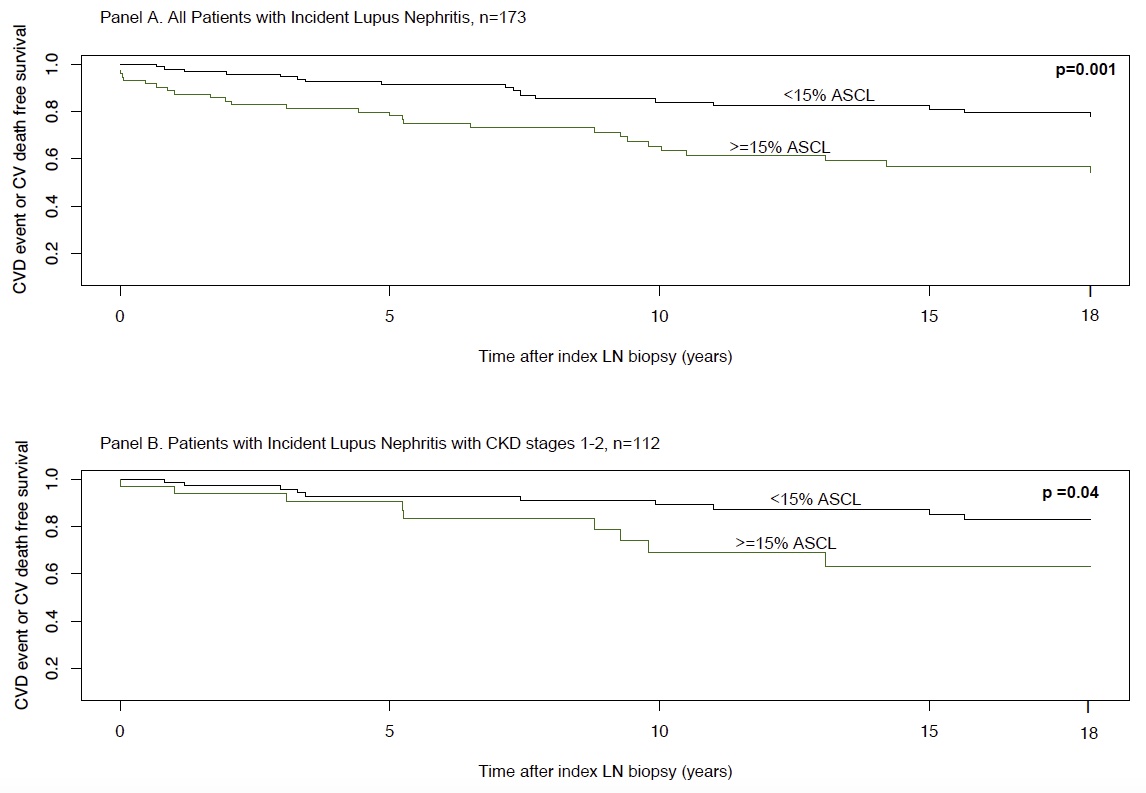
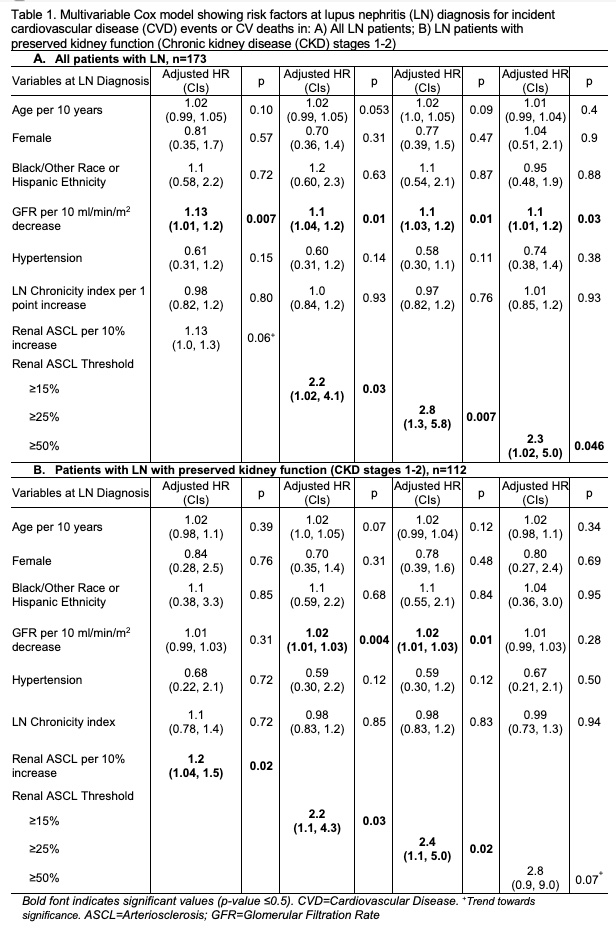
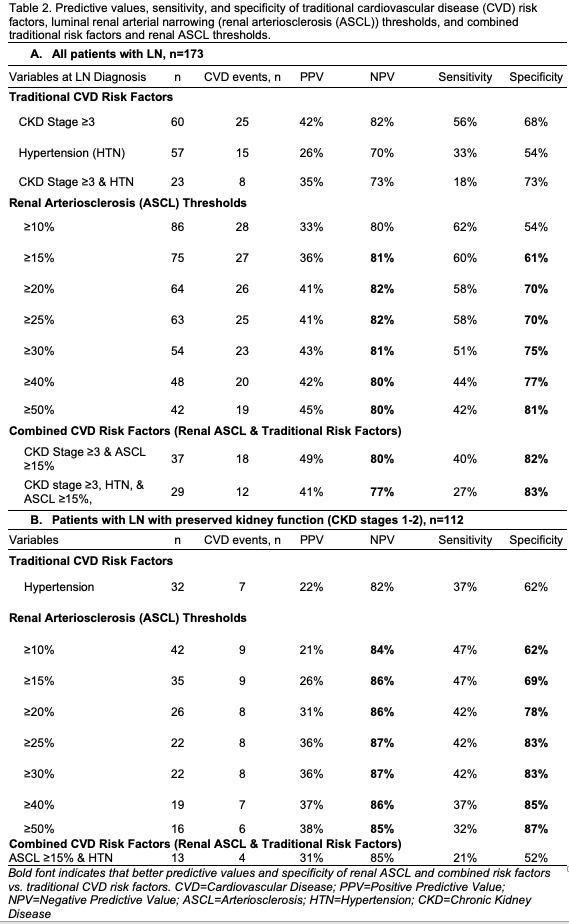
A total of 45 CVD-related deaths and events were observed during up to 18 years of follow-up after LN diagnosis. Mild renal ASCL changes (15% and 25% luminal narrowing) were associated with 2-3-fold higher risk of future CVD (Adjusted HR 2.2 & HR 2.8; Table 1A). The Cox proportional hazard model highlighted accelerated CVD events in patients with renal ASCL ≥15% compared to those without renal ASCL (Fig. 1A). Renal ASCL had higher specificity compared to traditional CV risk factors (Table 2A).
In those with persevered kidney function (n=112), mild renal ASCL predicted 2-fold higher risk of CVD (Adjusted HR 2.2 & HR 2.4; Table 1B). Again, patients with renal ASCL had accelerated CVD events even in this low-risk group (Fig. 1B). Renal ASCL was an early independent risk factor of future CVD with higher specificity than traditional CV risk factors in this low-risk group (Table 2B).
Conclusion: Renal arteriosclerosis found in kidney biopsy at LN diagnosis was a strong, early, and independent risk factor for future CVD events, outperforming traditional CVD risk factors. This observation held consistent even in LN patients with preserved kidney function. This suggests systematic grading of renal ASCL in LN biopsies may help to identify patients who could benefit from aggressive CVD prevention.
S. Garg: None; B. Astor: None; S. Lim: None; A. Raval: None; W. Zhong: None; S. Panzer: None; B. Rovin: AstraZeneca, 2, 5, Aurinia, 2, 5, Biogen, 2, F. Hoffmann-La Roche Ltd, 2, Genentech, 2, GlaxoSmithKlein(GSK), 2, Novartis, 2; C. Bartels: Pfizer, 5.
Background/Purpose: Patients < 40 years old with lupus nephritis (LN) face 42-fold higher risk of cardiovascular disease (CVD) compared to peers. Traditional CVD risk calculators fail to accurately predict future CVD risk in young LN patients, making decisions to prescribe empiric CVD prevention wrought with uncertainty. While a kidney biopsy is routinely performed to diagnose LN, renal arteriosclerosis (ASCL) is not routinely reported. Renal arteriosclerosis (ASCL) in kidney biopsies at LN diagnosis might represent changes in systemic arteries and could guide CVD risk stratification when most probably don't take this into account. Thus, in this study we systematically graded renal arteriosclerosis in kidney biopsies at LN diagnosis and examined its role as an early predictor of future incident CVD events.
Methods: Data were abstracted from adult LN patients who underwent diagnostic kidney biopsy between 1994-2021, including socio-demographics, traditional CVD risk factors, and pathology reports. Incident CVD-related deaths and non-fatal CVD events (ischemic heart disease, cerebrovascular accident, transient ischemic attack, and peripheral vascular disease) were adjudicated using published guidelines. Index standard of care kidney biopsies performed to diagnose LN were re-read by a pathologist to grade renal arteriosclerosis (ASCL) by calculating percent luminal narrowing of renal arteries using the Banff criteria. We examined the role of renal ASCL in diagnostic LN biopsies as an early predictor of future CVD using a Cox proportional hazards model in: a) all LN patients; b) those with preserved kidney function defined as chronic kidney disease stages 1-2.
Results: Among 173 adult patients with incident LN, 75% were female and 35% were of Black race or Hispanic ethnicity, and mean age at diagnosis was 38±17 years. Mean eGFR was 79±38 ml/min/1.73m2; 65% of patients had preserved kidney function. We noted 47% and 32% of patients had renal ASCL ≥15% and 25%.
A total of 45 CVD-related deaths and events were observed during up to 18 years of follow-up after LN diagnosis. Mild renal ASCL changes (15% and 25% luminal narrowing) were associated with 2-3-fold higher risk of future CVD (Adjusted HR 2.2 & HR 2.8; Table 1A). The Cox proportional hazard model highlighted accelerated CVD events in patients with renal ASCL ≥15% compared to those without renal ASCL (Fig. 1A). Renal ASCL had higher specificity compared to traditional CV risk factors (Table 2A).
In those with persevered kidney function (n=112), mild renal ASCL predicted 2-fold higher risk of CVD (Adjusted HR 2.2 & HR 2.4; Table 1B). Again, patients with renal ASCL had accelerated CVD events even in this low-risk group (Fig. 1B). Renal ASCL was an early independent risk factor of future CVD with higher specificity than traditional CV risk factors in this low-risk group (Table 2B).
Conclusion: Renal arteriosclerosis found in kidney biopsy at LN diagnosis was a strong, early, and independent risk factor for future CVD events, outperforming traditional CVD risk factors. This observation held consistent even in LN patients with preserved kidney function. This suggests systematic grading of renal ASCL in LN biopsies may help to identify patients who could benefit from aggressive CVD prevention.
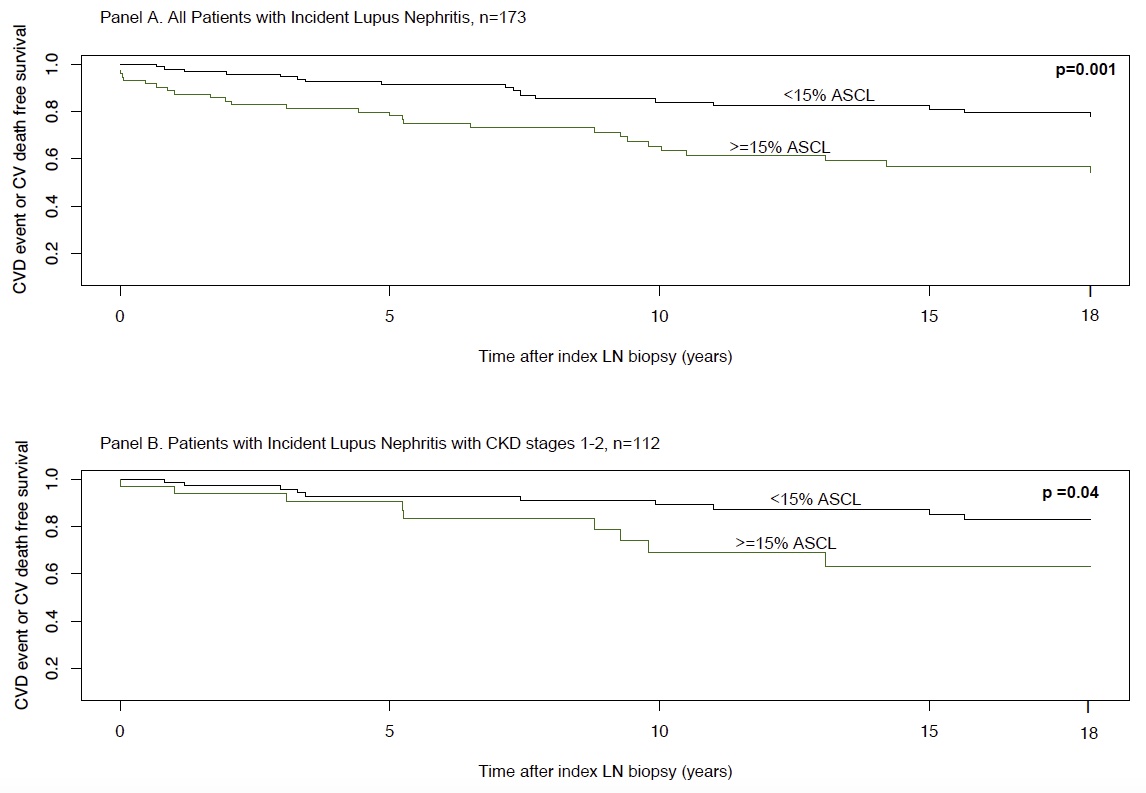
Figure 1. Survival curves showing CVD event or CVD related death free survival over 18-year follow-up period by 15% or more luminal narrowing of renal arteries (ASCL) in diagnostic LN biopsies in all patients with LN (Panel A.) and in patients with LN with preserved kidney function defined as CKD stages 1-2 (Panel B)
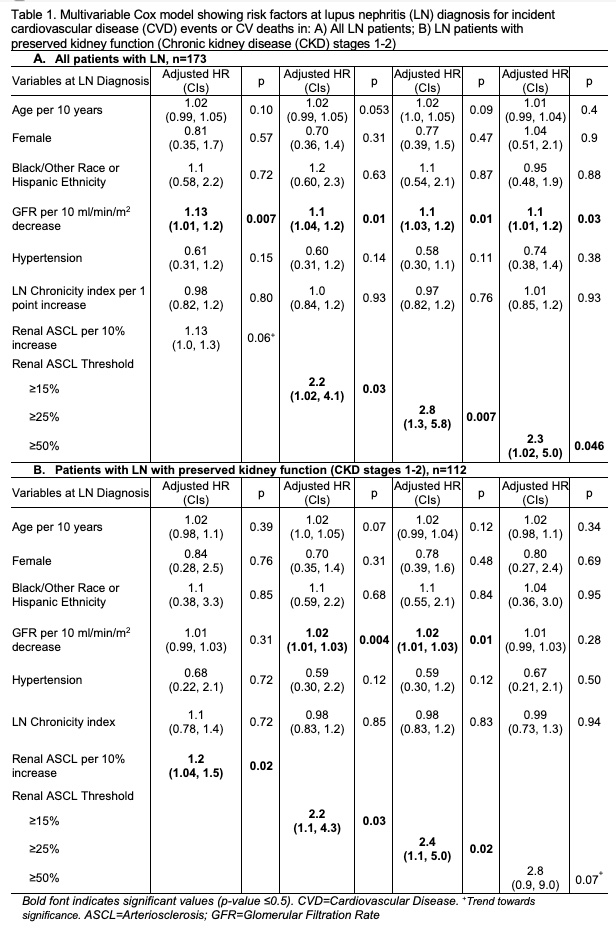
Table 1. Multivariable Cox model showing risk factors at lupus nephritis (LN) diagnosis for incident cardiovascular disease (CVD) events or CVD related deaths in: A) All LN patients; B) LN patients with preserved kidney function (CKD stages 1-2)
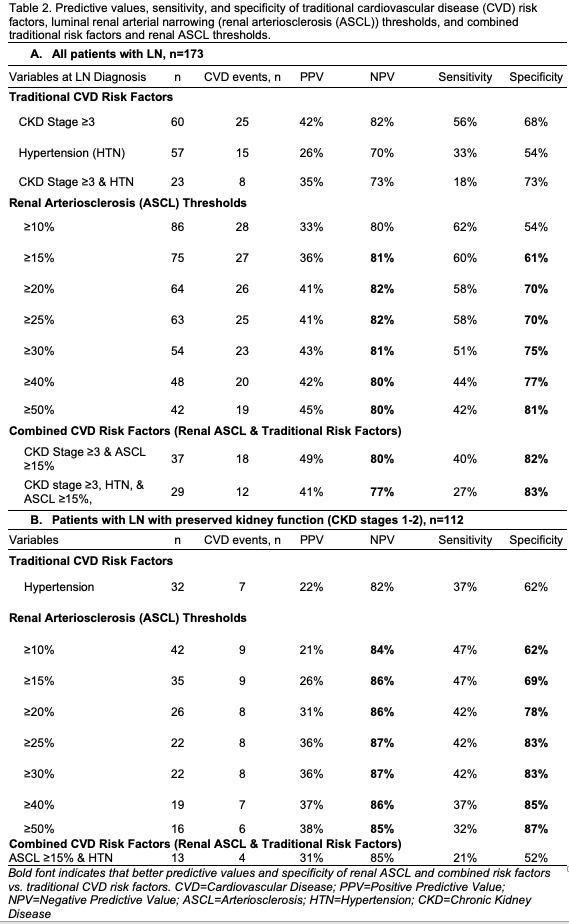
Table 2. Predictive values, sensitivity, and specificity of traditional cardiovascular disease (CVD) risk factors, luminal renal arterial narrowing (renal arteriosclerosis (ASCL)) thresholds, and combined traditional risk factors and renal ASCL thresholds.
S. Garg: None; B. Astor: None; S. Lim: None; A. Raval: None; W. Zhong: None; S. Panzer: None; B. Rovin: AstraZeneca, 2, 5, Aurinia, 2, 5, Biogen, 2, F. Hoffmann-La Roche Ltd, 2, Genentech, 2, GlaxoSmithKlein(GSK), 2, Novartis, 2; C. Bartels: Pfizer, 5.



