Poster Session A
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (0483–0509) Spondyloarthritis Including Psoriatic Arthritis – Diagnosis, Manifestations, & Outcomes Poster I: PsA
0506: Patient and Physician Global Assessment of Psoriatic Arthritis Disease Activity: High Concordance in an ArLAR Multinational Study
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- AM
Avin Maroof, MD, DO, MSc, MBChB
University of Kurdistan Hawler
Erbil, IraqDisclosure information not submitted.
Abstract Poster Presenter(s)
Nelly Ziade1, Noura Abbas2, Lina El Kibbi3, Avin Maroof4, Bassel Elzorkany5, Nizar Ani6, ASAL ADNAN7, NABAA IHSAN JAWAD AWADH7, Faiq Gorial8, Nada Alchama9, Chafika Haouichat10, Fatima Alnaimat11, Suad Hannawi12, Saed Atawnah13, HUSSEIN HALABI14, Manal Al-Mashaleh15, Laila Aljazwi16, Ahmed Abogamal17, laila Ayoub18, Elyes Bouajina19, Rachid Bahiri20, Sahar Saad21, Maha Sabkar21, Krystel Aouad22, Laure Gossec23 and Ihsane Hmamouchi24, 1Saint-Joseph University, Beirut, Lebanon, 2Saint Joseph University Beirut, Beirut, Lebanon, 3Specialized Medical Center, Riyadh, Saudi Arabia, 4Kurdistan University Hawler, Erbil, Iraq, 5Private (BZRC), Cairo, Egypt, 6Baghdad College of Medicine, Baghdad, Iraq, 7Baghdad Teaching Hospital, Baghdad, Iraq, 8University of Baghdad, Baghdad, Iraq, 9Ebn Al Nafiss Hospital, Damascus, Syria, 10Faculty of Medicine El Mahdi Si Ahmed, Blida, Algeria, 11University of Jordan, Amman, Jordan, 12Kuwait Hospital, Department of Rheumatology, Dubai, United Arab Emirates, 13Al ahli hospital, Hebron, Palestine, Hebron, Palestinian Territories, 14King Faisal Specialist Hospital & Research Centre, Jeddah, Saudi Arabia, 15Royal Medical Services, Amman, Jordan, 16Tripoli, Tripoli, Libya, 17Saudi German Hospital Dubai, Dubai, United Arab Emirates, 18University of Tripoli, Tripoli, Libya, 19Farhat Hached Hospital of Sousse, Sousse, Tunisia, 20Department of Rheumatology, El Ayachi Hospital Medical University, Sale, Morocco, 21King Hamad University Hospital, Bahrain, Bahrain, 22Saint George Hospital University Medical Center, Beirut, Lebanon, 23Sorbonne Université and Pitié Salpêtrière Hospital, Paris, France, 24Rheumatology Unit, Lalla Aicha Temara Hospital, Temara, Morocco
Background/Purpose: In patients with psoriatic arthritis (PsA), discordance between physicians and patients when assessing disease activity has been described as frequent, mainly in European and North American studies. This discordance may negatively impact treatment adherence and shared decision-making processes. Culture and beliefs influence patients' perceptions of health.
The purpose of this study was to evaluate the concordance between patient- (PGA) and physician-global assessment (PhGA) of PsA disease activity and its association with demographic and disease characteristics in a multinational group of patients from Arab countries.
Methods: This multicentric multinational cross-sectional study was conducted in thirteen Arab countries by the Arab League of Associations of Rheumatology (ArLAR) research group (ARCH). During a single routine visit, patients and physicians rated PsA disease activity on a numeric scale from 0 (no activity) to 10 (worse activity). In addition, demographic and disease data were collected, as well as PGA and PhGA for psoriasis (PsO) activity, Health Assessment Questionnaire (HAQ), Fibromyalgia Rapid Screening Tool (FiRST), Patient Health Questionnaire (PHQ4) and Disease Activity in Psoriatic Arthritis (DAPSA). First, the correlation between PGA and PhGA for PsA and PsO disease activity was assessed statistically using the Spearman correlation coefficient and graphically using the Bland and Altman method. Second, concordance between the PGA and PhGA PsA activity (defined as a difference between -2 and 2) was calculated and correlated with demographic and disease factors using multivariable binary logistic regression.
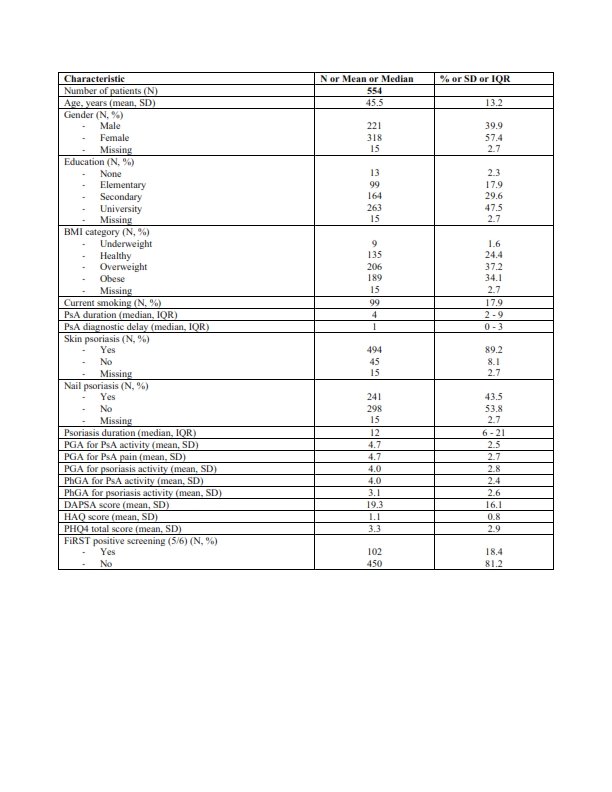
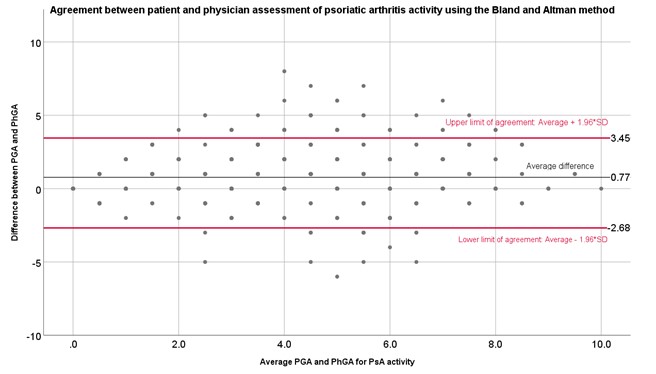
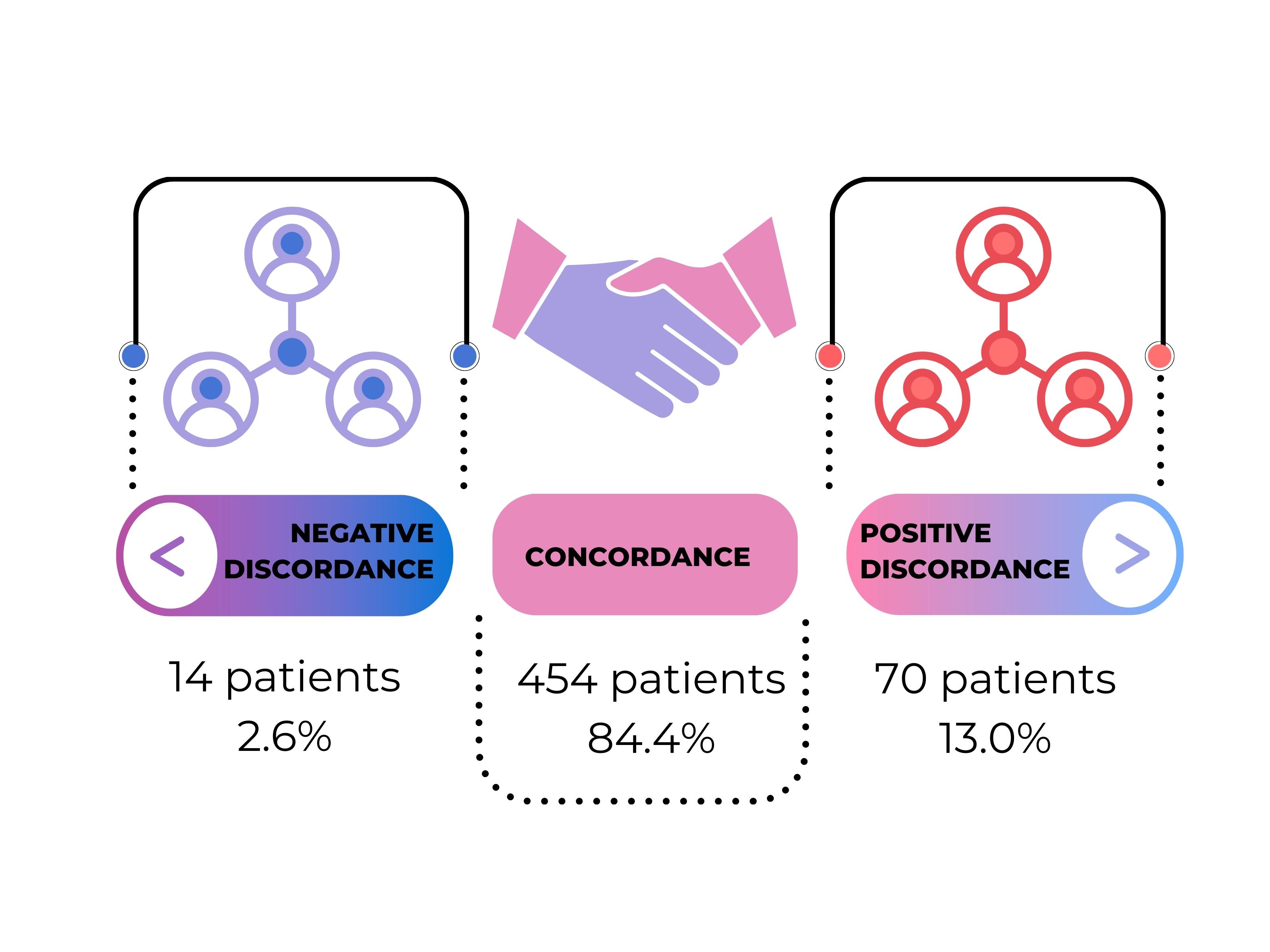
Results: The study included 554 patients from thirteen countries: mean age 45 years (SD 13), 57% females, median disease duration four years (IQR 2-9); 89.2% had skin PsO, and 43.5% had nail PsO. The disease was active overall: mean DAPSA was 19.3 (SD 16.1), HAQ 1.1 (SD 0.8), and PHQ4 3.3 (SD 2.9). The screening test for widespread pain was positive in 18.4% of patients (Table 1). The mean PGA for PsA activity was 4.7 (SD 2.5) versus a PhGA of 3.9 (SD 2.4). Similarly, PGA for psoriasis activity was 4.0 (SD 2.8), and PhGA was 3.1 (SD 2.6). The correlation between PGA and PhGA was strong for PsA activity (r= 0.738) (with good agreement on Bland and Altman (Figure 1)) and moderate for psoriasis activity (r=0.613). Among 554 patients' measurements, 358 (84.2%) were in concordance with the physician's global assessment (Figure 2). In the multivariable analysis, concordance was independently associated with a high CRP (OR 2.32 [95%CI 1.33; 4.02] and DAPSA category (better concordance in patients in remission (OR 1.02 (95%CI 1.01; 1.03]).
Conclusion: In this unselected sample of patients from Arab countries, there was a strong concordance between PGA and PhGA of PsA activity. This raises questions about patient expectations and pain perceptions in Arab countries. Concordance was stronger for PsA than PsO, indicating that rheumatologists may be more comfortable assessing joints than skin. The patient's evaluation of disease activity needs to be taken into account when considering the disease management plan, especially in patients who are not in remission.
N. Ziade: Abbvie, 6, Boehringer-Ingelheim, 6, Eli Lilly, 6, Janssen, 6, Newbridge, 6, Novartis, 6, Pfizer, 6, Pierre Fabre, 6, Roche, 6, sanofi, 6; N. Abbas: None; L. El Kibbi: None; A. Maroof: None; B. Elzorkany: None; N. Ani: None; A. ADNAN: None; N. AWADH: None; F. Gorial: None; N. Alchama: None; C. Haouichat: None; F. Alnaimat: None; S. Hannawi: GSK, 2, 6; S. Atawnah: None; H. HALABI: None; M. Al-Mashaleh: None; L. Aljazwi: None; A. Abogamal: None; l. Ayoub: None; E. Bouajina: None; R. Bahiri: None; S. Saad: None; M. Sabkar: None; K. Aouad: None; L. Gossec: AbbVie, 2, 12, Personal fees, Amgen, 2, Biogen, 5, BMS, 12, Personal fees, Celltrion, 12, Personal fees, Eli Lilly, 5, 12, Personal fees, Galapagos, 12, Personal fees, Janssen, 12, Personal fees, MSD, 12, Personal fees, Novartis, 5, 12, Personal fees, Pfizer, 12, Personal fees, Sandoz, 5, 12, Personal fees, UCB Pharma, 5, 12, Personal fees; I. Hmamouchi: None.
Background/Purpose: In patients with psoriatic arthritis (PsA), discordance between physicians and patients when assessing disease activity has been described as frequent, mainly in European and North American studies. This discordance may negatively impact treatment adherence and shared decision-making processes. Culture and beliefs influence patients' perceptions of health.
The purpose of this study was to evaluate the concordance between patient- (PGA) and physician-global assessment (PhGA) of PsA disease activity and its association with demographic and disease characteristics in a multinational group of patients from Arab countries.
Methods: This multicentric multinational cross-sectional study was conducted in thirteen Arab countries by the Arab League of Associations of Rheumatology (ArLAR) research group (ARCH). During a single routine visit, patients and physicians rated PsA disease activity on a numeric scale from 0 (no activity) to 10 (worse activity). In addition, demographic and disease data were collected, as well as PGA and PhGA for psoriasis (PsO) activity, Health Assessment Questionnaire (HAQ), Fibromyalgia Rapid Screening Tool (FiRST), Patient Health Questionnaire (PHQ4) and Disease Activity in Psoriatic Arthritis (DAPSA). First, the correlation between PGA and PhGA for PsA and PsO disease activity was assessed statistically using the Spearman correlation coefficient and graphically using the Bland and Altman method. Second, concordance between the PGA and PhGA PsA activity (defined as a difference between -2 and 2) was calculated and correlated with demographic and disease factors using multivariable binary logistic regression.
Results: The study included 554 patients from thirteen countries: mean age 45 years (SD 13), 57% females, median disease duration four years (IQR 2-9); 89.2% had skin PsO, and 43.5% had nail PsO. The disease was active overall: mean DAPSA was 19.3 (SD 16.1), HAQ 1.1 (SD 0.8), and PHQ4 3.3 (SD 2.9). The screening test for widespread pain was positive in 18.4% of patients (Table 1). The mean PGA for PsA activity was 4.7 (SD 2.5) versus a PhGA of 3.9 (SD 2.4). Similarly, PGA for psoriasis activity was 4.0 (SD 2.8), and PhGA was 3.1 (SD 2.6). The correlation between PGA and PhGA was strong for PsA activity (r= 0.738) (with good agreement on Bland and Altman (Figure 1)) and moderate for psoriasis activity (r=0.613). Among 554 patients' measurements, 358 (84.2%) were in concordance with the physician's global assessment (Figure 2). In the multivariable analysis, concordance was independently associated with a high CRP (OR 2.32 [95%CI 1.33; 4.02] and DAPSA category (better concordance in patients in remission (OR 1.02 (95%CI 1.01; 1.03]).
Conclusion: In this unselected sample of patients from Arab countries, there was a strong concordance between PGA and PhGA of PsA activity. This raises questions about patient expectations and pain perceptions in Arab countries. Concordance was stronger for PsA than PsO, indicating that rheumatologists may be more comfortable assessing joints than skin. The patient's evaluation of disease activity needs to be taken into account when considering the disease management plan, especially in patients who are not in remission.
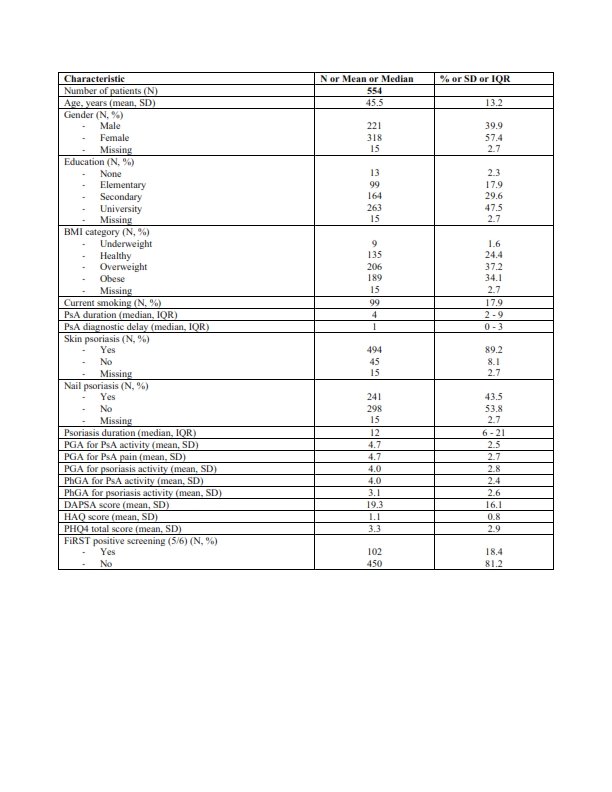
Table 1. Patients’ and disease’s characteristics.
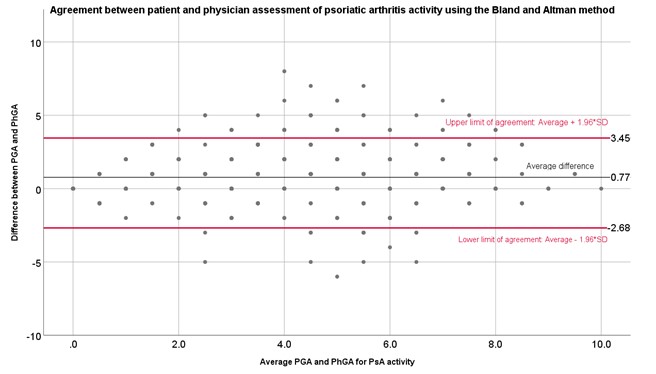
Figure 1. Agreement between PGA (Patient) and PhGA (Physician Global Assessment) of PsA activity using the Bland and Altman plot. Each dot is the difference between PGA and PhGA for a specific patient.
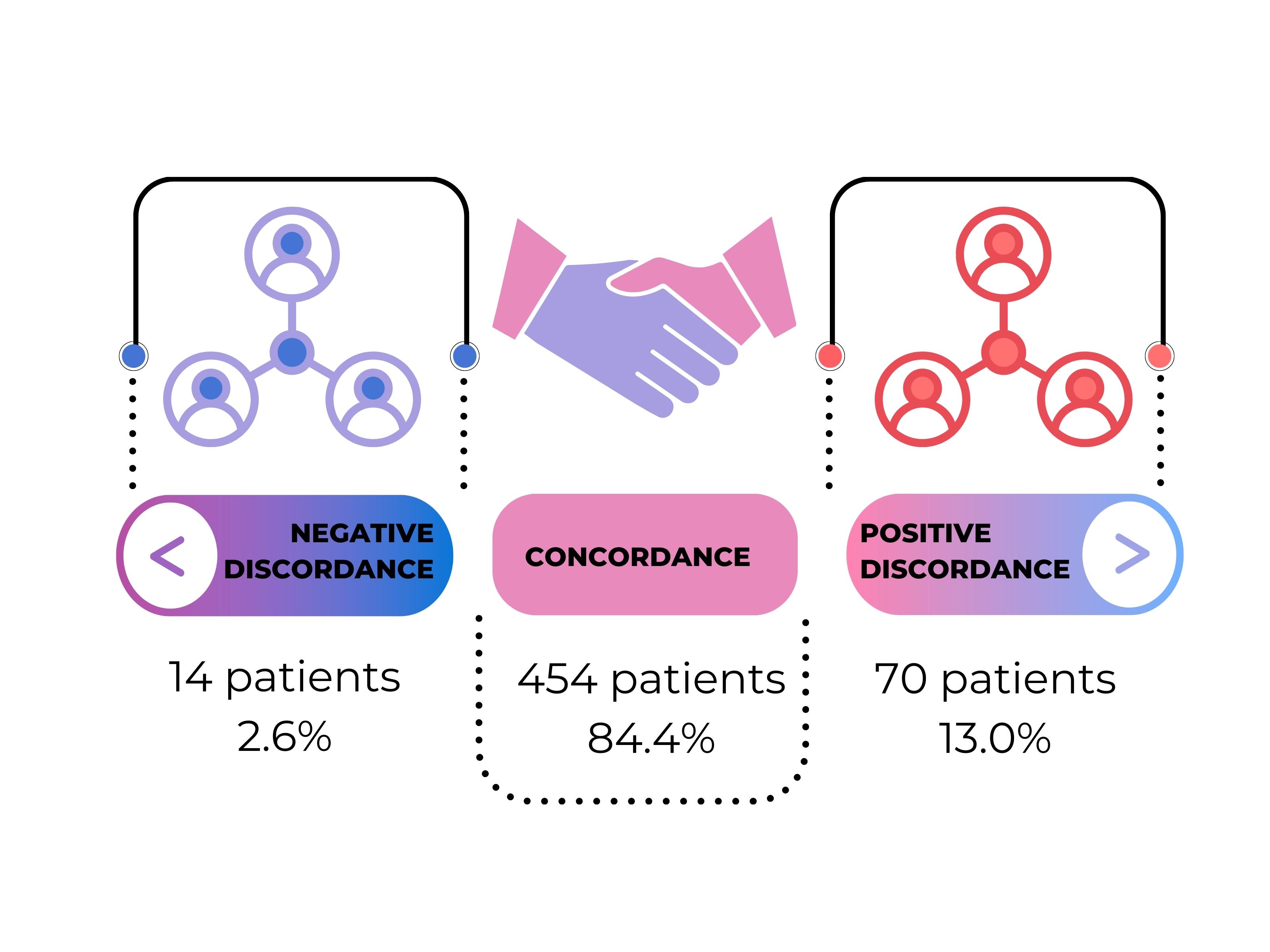
Figure 2. Concordance between PGA and PhGA of PsA activity, defined by a difference (PGA – PhGA) comprised between -2 and +2 (total available = 538 pairs)
N. Ziade: Abbvie, 6, Boehringer-Ingelheim, 6, Eli Lilly, 6, Janssen, 6, Newbridge, 6, Novartis, 6, Pfizer, 6, Pierre Fabre, 6, Roche, 6, sanofi, 6; N. Abbas: None; L. El Kibbi: None; A. Maroof: None; B. Elzorkany: None; N. Ani: None; A. ADNAN: None; N. AWADH: None; F. Gorial: None; N. Alchama: None; C. Haouichat: None; F. Alnaimat: None; S. Hannawi: GSK, 2, 6; S. Atawnah: None; H. HALABI: None; M. Al-Mashaleh: None; L. Aljazwi: None; A. Abogamal: None; l. Ayoub: None; E. Bouajina: None; R. Bahiri: None; S. Saad: None; M. Sabkar: None; K. Aouad: None; L. Gossec: AbbVie, 2, 12, Personal fees, Amgen, 2, Biogen, 5, BMS, 12, Personal fees, Celltrion, 12, Personal fees, Eli Lilly, 5, 12, Personal fees, Galapagos, 12, Personal fees, Janssen, 12, Personal fees, MSD, 12, Personal fees, Novartis, 5, 12, Personal fees, Pfizer, 12, Personal fees, Sandoz, 5, 12, Personal fees, UCB Pharma, 5, 12, Personal fees; I. Hmamouchi: None.



