Poster Session A
Diversity, inclusion and racial disparities
Session: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
0194: Reproductive Health Conversations with a Primarily Hispanic Systemic Lupus Erythematosus Population: Influences and Barriers
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- ZZ
Abstract Poster Presenter(s)
Zarmeen Zaheer1, Martha Delgado2, Jack Rodman3, Julia Simard4, Sandy Lee5 and Leanna Wise6, 1Huntington Health, Tampa, FL, 2LAC+USC/Keck School of Medicine, Los Angeles, CA, 3University of Southern California, Los Angeles, CA, 4Department of Epidemiology & Population Health, Stanford University School of Medicine, Stanford, CA, 5University of Southern California, Walnut, CA, 6LAC+USC/Keck Medicine of USC, Pasadena, CA
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune disease most commonly seen in women of childbearing age, with a greater burden in non-Caucasian populations. The American College of Rheumatology (ACR) published guidelines in 2020 to inform a shared decision-making process on reproductive health management between patients and their physicians. However, there is little data as to how these guidelines are experienced by patients in the "real world" setting, and specifically by Hispanic patients, who have high rates of poor SLE outcomes. Our patient survey assesses influences on and barriers to reproductive health conversations and explores how a predominantly Hispanic SLE population obtains reproductive health information.
Methods: A 28-question survey was distributed in either English or Spanish to female patients with SLE ages 18 - 50 in our outpatient urban Los Angeles rheumatology clinic. Questions focused on four areas – contraception, preconception counseling, pregnancy management, and medication safety – and were informed by the ACR guidelines. The majority of the questions were multiple choice. Patients were not required to answer all questions and branching logic was used depending on patients' unique reproductive history. Data were presented using frequency (%) or median (IQR) and evaluated using Fisher's exact or Wilcoxon rank sum test, as appropriate.
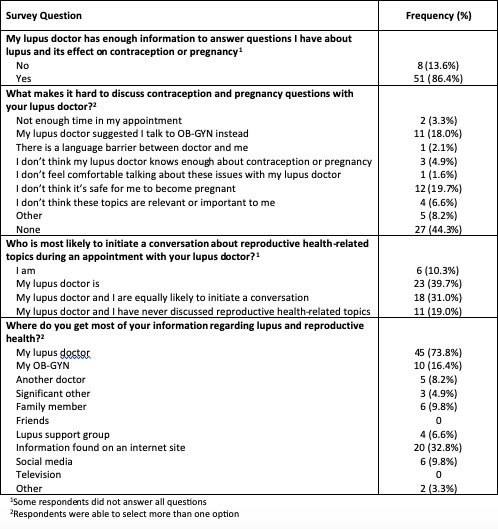
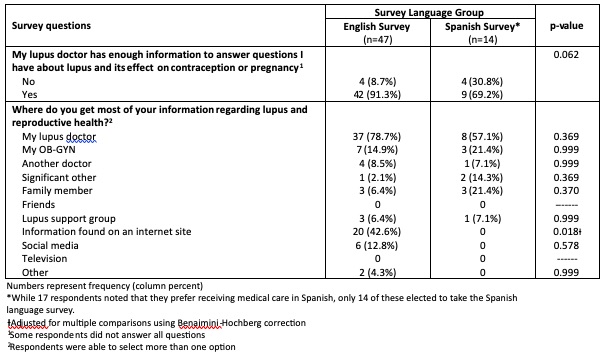
Results: From March 15, 2023 to May 16, 2023, 61 surveys were collected (Table 1). Response rate was 92%. 40% of patients noted that the rheumatologist was most likely to initiate a conversation about reproductive health-related topics; 31% reported that patient and rheumatologist were equally likely to initiate such a conversation, and 19% noted never having any such conversation (Table 2).86% of respondents believed that their rheumatologist had sufficient expertise to answer questions about the effect of SLE on contraception use and pregnancy planning, however, this was observed more frequently in the English survey (91%) compared to the Spanish survey (69%) (p = 0.062) (Table 3). 56% of patients identified that there were difficulties with reproductive health care discussions, most commonly noting: "I don't think it's safe for me to become pregnant" (19.7%), and "my lupus doctor has suggested that I talk with an OBGYN instead" (18%). Respondents noted their top three sources for reproductive health information as their rheumatologists (73.8%), the internet (32.8%), and their OBGYN (16.4%) (Table 2).
Conclusion: Our data show that most respondents of our primarily Hispanic SLE population in a safety-net clinic rely on the rheumatologist as a crucial source of reproductive health information. However, more than half reported that there were difficulties with reproductive health conversations, including patients' perception about the safety of pregnancy, and rheumatologists deferring to OBGYNs. Furthermore, nearly 20% noted never having a reproductive health conversation with a rheumatologist. Given the above, effective interventions to improve evidence-based reproductive health conversations between Hispanic patients with SLE and rheumatologists should be investigated.
.jpg)
Z. Zaheer: None; M. Delgado: None; J. Rodman: None; J. Simard: None; S. Lee: None; L. Wise: AstraZeneca, 6, Aurinia Pharma, 2, 6, GlaxoSmithKlein(GSK), 6.
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune disease most commonly seen in women of childbearing age, with a greater burden in non-Caucasian populations. The American College of Rheumatology (ACR) published guidelines in 2020 to inform a shared decision-making process on reproductive health management between patients and their physicians. However, there is little data as to how these guidelines are experienced by patients in the "real world" setting, and specifically by Hispanic patients, who have high rates of poor SLE outcomes. Our patient survey assesses influences on and barriers to reproductive health conversations and explores how a predominantly Hispanic SLE population obtains reproductive health information.
Methods: A 28-question survey was distributed in either English or Spanish to female patients with SLE ages 18 - 50 in our outpatient urban Los Angeles rheumatology clinic. Questions focused on four areas – contraception, preconception counseling, pregnancy management, and medication safety – and were informed by the ACR guidelines. The majority of the questions were multiple choice. Patients were not required to answer all questions and branching logic was used depending on patients' unique reproductive history. Data were presented using frequency (%) or median (IQR) and evaluated using Fisher's exact or Wilcoxon rank sum test, as appropriate.
Results: From March 15, 2023 to May 16, 2023, 61 surveys were collected (Table 1). Response rate was 92%. 40% of patients noted that the rheumatologist was most likely to initiate a conversation about reproductive health-related topics; 31% reported that patient and rheumatologist were equally likely to initiate such a conversation, and 19% noted never having any such conversation (Table 2).86% of respondents believed that their rheumatologist had sufficient expertise to answer questions about the effect of SLE on contraception use and pregnancy planning, however, this was observed more frequently in the English survey (91%) compared to the Spanish survey (69%) (p = 0.062) (Table 3). 56% of patients identified that there were difficulties with reproductive health care discussions, most commonly noting: "I don't think it's safe for me to become pregnant" (19.7%), and "my lupus doctor has suggested that I talk with an OBGYN instead" (18%). Respondents noted their top three sources for reproductive health information as their rheumatologists (73.8%), the internet (32.8%), and their OBGYN (16.4%) (Table 2).
Conclusion: Our data show that most respondents of our primarily Hispanic SLE population in a safety-net clinic rely on the rheumatologist as a crucial source of reproductive health information. However, more than half reported that there were difficulties with reproductive health conversations, including patients' perception about the safety of pregnancy, and rheumatologists deferring to OBGYNs. Furthermore, nearly 20% noted never having a reproductive health conversation with a rheumatologist. Given the above, effective interventions to improve evidence-based reproductive health conversations between Hispanic patients with SLE and rheumatologists should be investigated.
.jpg)
Table 1. Demographic and clinical characteristics for all 61 patient respondents
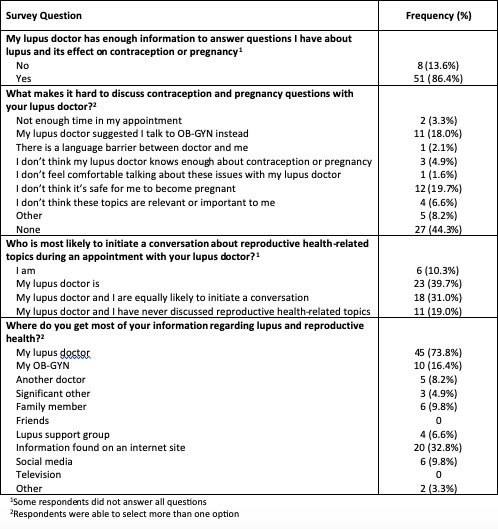
Table 2. Influences on reproductive health conversations (given the total N for this table)
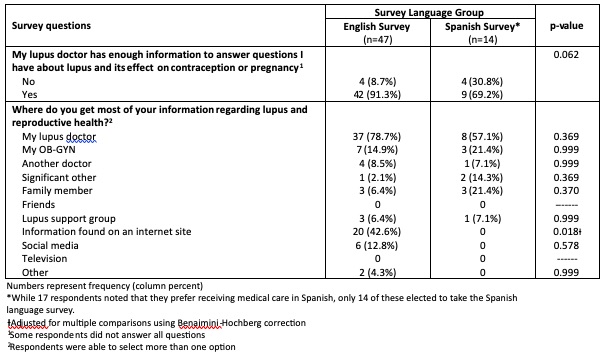
Table 3. Barriers and contraception discussion by survey language group
Z. Zaheer: None; M. Delgado: None; J. Rodman: None; J. Simard: None; S. Lee: None; L. Wise: AstraZeneca, 6, Aurinia Pharma, 2, 6, GlaxoSmithKlein(GSK), 6.



