Poster Session A
Infection-related rheumatic syndromes
Session: (0196–0228) Infection-related Rheumatic Disease Poster
0208: Pneumocystis Jirovecii Pneumonia (PJP) Prophylaxis (PPX), Investigating the Practice Patterns of Providers for Patients on Chronic, High-Dose Immunosuppression in a Rural Integrated Health System
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- AB
Angela Bobak, DO (she/her/hers)
Geisinger Medical Center Internal Medicine Residency
Danville, PA, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Angela Bobak1, Emely Pimentel1, Jordan Jackson2, Celia Gray3, Hema Srinivasan3, Andrea Berger3 and David Bulbin3, 1Geisinger Medical Center Internal Medicine Residency, Danville, PA, 2Geisinger Medical Center Medicine-Pediatrics Residency, Danville, PA, 3Geisinger Health System, Danville, PA
Background/Purpose: PJP is an opportunistic fungus causing significant morbidity and mortality in immunocompromised patients. Guidelines describe PJP PPX indications among non-HIV infected individuals with cancer and solid organ transplant; however, this is lacking for individuals with rheumatic diseases requiring immunosuppression. General consensus reveals PJP PPX should be considered in patients receiving medication associated with lymphodepletion, likely to cause defects in cell-mediated immunity. Examples include prednisone 20mg or greater, monoclonal antibodies (anti-CD52 alemtuzumab and anti-CD20 rituximab), alkylating agents (cyclophosphamide), and checkpoint inhibitors (pembrolizumab, nivolumab, durvalumab). We conducted a restrospective analysis investigating the percentage of patients, within our rural system, who received appropriate PJP PPX when on immunosuppression and if discrepancies exist among specialties. We aim to determine the incidence of PJP and if PPX causes a reduction in infection risk.
Methods: A retrospective chart review of the electronic medical record was performed for adult patients from 2016-2021 prescribed immunosuppression in the form of prednisone ≥ 20mg for at least 4 weeks or any duration of alemtuzumab, cyclophosphamide, durvalumab, nivolumab, pembrolizumab, and rituximab. Prescribers within rheumatology, hematology/oncology, neurology, pulmonology, dermatology, nephrology, and gastroenterology were included. Exclusion criteria included HIV, solid organ transplant, and active cancer. Forms of PJP PPX included TMP/SMX, atovaquone, dapsone, or inhaled pentamidine. PJP diagnosis was included if occurred within one year of immunosuppression. A chi-square test and logistic regression model were used to compare PPX prescriptions by department. Odds ratio and 95% confidence intervals are reported.
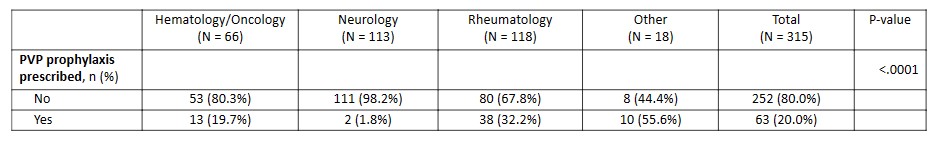
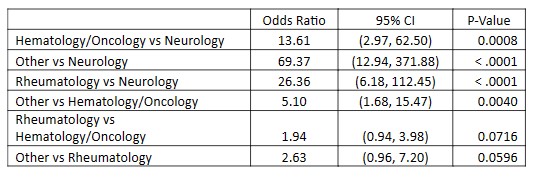
Results: We identified a cohort of 16,500 individual patients with 52,409 prescription encounters. Two PJP cases occurred in individuals not on PPX but prescribed the following: (rituximab and prednisone 40mg) and (rituximab and prednisone 80mg). Initial review of alemtuzumab, cyclophosphamide, durvalumab, nivolumab, pembrolizumab, and rituximab produced 315 patients and 2,508 prescription encounters with 20% of patients receiving PPX. The proportion of patients prescribed PPX differed by department (p < .0001) with the following: rheumatology 32.2%, hematology/oncology 19.7%, and neurology 1.8%. Pairwise odds ratio estimates and 95% confidence intervals from a logistic regression model demonstrated that rheumatology prescribed PPX significantly more than neurology (odds ratio, 26.36 [95% CI, 6.18-112.45], p < .0001). Review of prednisone prescription encounters is still ongoing, with percentage of appropriate PPX and risk reduction analysis to be included at final presentation.
Conclusion: PJP carries significant morbidity and mortality for patients on immunosuppression; however, PPX is highly underutilized in our rural health care system. Further investigation is needed to identify factors leading to low PPX rates and determining the incidence and severity of adverse effects from PPX, as these often influence prescriber practices.
A. Bobak: None; E. Pimentel: None; J. Jackson: None; C. Gray: None; H. Srinivasan: None; A. Berger: None; D. Bulbin: AbbVie/Abbott, 2, 6, Alexion, 2, 6, Amgen, 2, 6, Novartis, 2, Sanofi Genzyme, 6.
Background/Purpose: PJP is an opportunistic fungus causing significant morbidity and mortality in immunocompromised patients. Guidelines describe PJP PPX indications among non-HIV infected individuals with cancer and solid organ transplant; however, this is lacking for individuals with rheumatic diseases requiring immunosuppression. General consensus reveals PJP PPX should be considered in patients receiving medication associated with lymphodepletion, likely to cause defects in cell-mediated immunity. Examples include prednisone 20mg or greater, monoclonal antibodies (anti-CD52 alemtuzumab and anti-CD20 rituximab), alkylating agents (cyclophosphamide), and checkpoint inhibitors (pembrolizumab, nivolumab, durvalumab). We conducted a restrospective analysis investigating the percentage of patients, within our rural system, who received appropriate PJP PPX when on immunosuppression and if discrepancies exist among specialties. We aim to determine the incidence of PJP and if PPX causes a reduction in infection risk.
Methods: A retrospective chart review of the electronic medical record was performed for adult patients from 2016-2021 prescribed immunosuppression in the form of prednisone ≥ 20mg for at least 4 weeks or any duration of alemtuzumab, cyclophosphamide, durvalumab, nivolumab, pembrolizumab, and rituximab. Prescribers within rheumatology, hematology/oncology, neurology, pulmonology, dermatology, nephrology, and gastroenterology were included. Exclusion criteria included HIV, solid organ transplant, and active cancer. Forms of PJP PPX included TMP/SMX, atovaquone, dapsone, or inhaled pentamidine. PJP diagnosis was included if occurred within one year of immunosuppression. A chi-square test and logistic regression model were used to compare PPX prescriptions by department. Odds ratio and 95% confidence intervals are reported.
Results: We identified a cohort of 16,500 individual patients with 52,409 prescription encounters. Two PJP cases occurred in individuals not on PPX but prescribed the following: (rituximab and prednisone 40mg) and (rituximab and prednisone 80mg). Initial review of alemtuzumab, cyclophosphamide, durvalumab, nivolumab, pembrolizumab, and rituximab produced 315 patients and 2,508 prescription encounters with 20% of patients receiving PPX. The proportion of patients prescribed PPX differed by department (p < .0001) with the following: rheumatology 32.2%, hematology/oncology 19.7%, and neurology 1.8%. Pairwise odds ratio estimates and 95% confidence intervals from a logistic regression model demonstrated that rheumatology prescribed PPX significantly more than neurology (odds ratio, 26.36 [95% CI, 6.18-112.45], p < .0001). Review of prednisone prescription encounters is still ongoing, with percentage of appropriate PPX and risk reduction analysis to be included at final presentation.
Conclusion: PJP carries significant morbidity and mortality for patients on immunosuppression; however, PPX is highly underutilized in our rural health care system. Further investigation is needed to identify factors leading to low PPX rates and determining the incidence and severity of adverse effects from PPX, as these often influence prescriber practices.
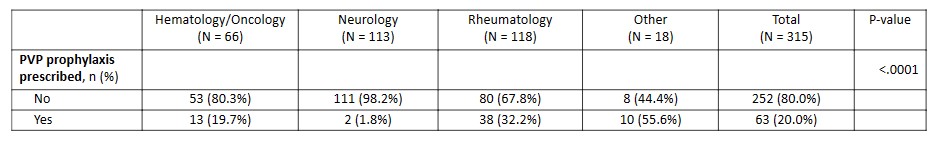
Table 1. The proportion of patients with PPX prescriptions did differ by department (chi-square test: p < .0001). Rheumatology had the highest proportion (32.2%), followed by hematology/oncology (19.7%) and neurology (1.8%). The grouping designated "other" consisted of small sample size specialties including nephrology (n = 11), dermatology (n = 3), and unspecified.
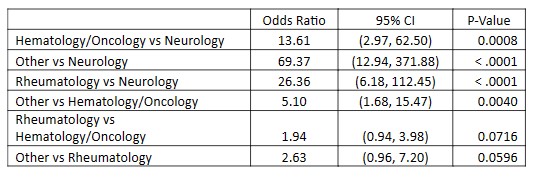
Table 2. This table consists of the pairwise odds ratio estimates and their 95% confidence intervals from a logistic regression model with PPX prescription as the outcome and department as the predictor. Rheumatology prescribed PPX significantly more than neurology, but rheumatology did not have significantly increased PPX rates compared with hematology/oncology or the "other" category. All departments prescribed PPX more frequenly than neurology.
A. Bobak: None; E. Pimentel: None; J. Jackson: None; C. Gray: None; H. Srinivasan: None; A. Berger: None; D. Bulbin: AbbVie/Abbott, 2, 6, Alexion, 2, 6, Amgen, 2, 6, Novartis, 2, Sanofi Genzyme, 6.



