Poster Session A
Rheumatoid arthritis (RA)
Session: (0380–0422) RA – Diagnosis, Manifestations, and Outcomes Poster I
0416: Association Between Sleep Disorders and Rheumatoid Arthritis: A Population-based Cohort Study
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- RK
Rakesh Kumar, MD, MBBS
Mayo Clinic
Rochester, MN, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Rakesh Kumar1, Edward Lovering1, Chanakya Kodishala2, Sara Achenbach3, Diego Carvalho1, Cynthia Crowson1, John Davis1 and Elena Myasoedova1, 1Mayo Clinic, Rochester, MN, 2Mayo Clinic Rochester Minnesota, Rochester, MN, 3Mayo Clinic, Rochester, MN, Rochester, MN
Background/Purpose: Some sleep disorders (SD) are more prevalent in patients with chronic inflammatory diseases, such as Rheumatoid Arthritis (RA). However, most of the research has focused on obstructive sleep apnea (OSA), and less is known about other SD (i.e., insomnia, restless legs syndrome [RLS]). The incidence of SD over time is also not well understood. Therefore, we aimed to examine the incidence of sleep disorders in patients with RA vs comparators without RA over time and by serologic status.
Methods: This retrospective population-based cohort study included residents of a geographically defined area, aged ≥50 years when they met 1987 ACR criteria for incident RA in 1980-2009. All these patients were followed until death/migration or 12/31/2021 and matched 1:1 on age, sex, and calendar year with non-RA comparators. SD were identified based on two ICD 9/10-CM codes and data were abstracted via manual record review. Demographics, medical comorbidities, laboratory data on RA characteristics were collected. We investigated the association between RA and sleep disorders by using Cox models, adjusting for age and sex. P-value < 0.05 was considered significant. All analyses were performed using SAS version 9.4.
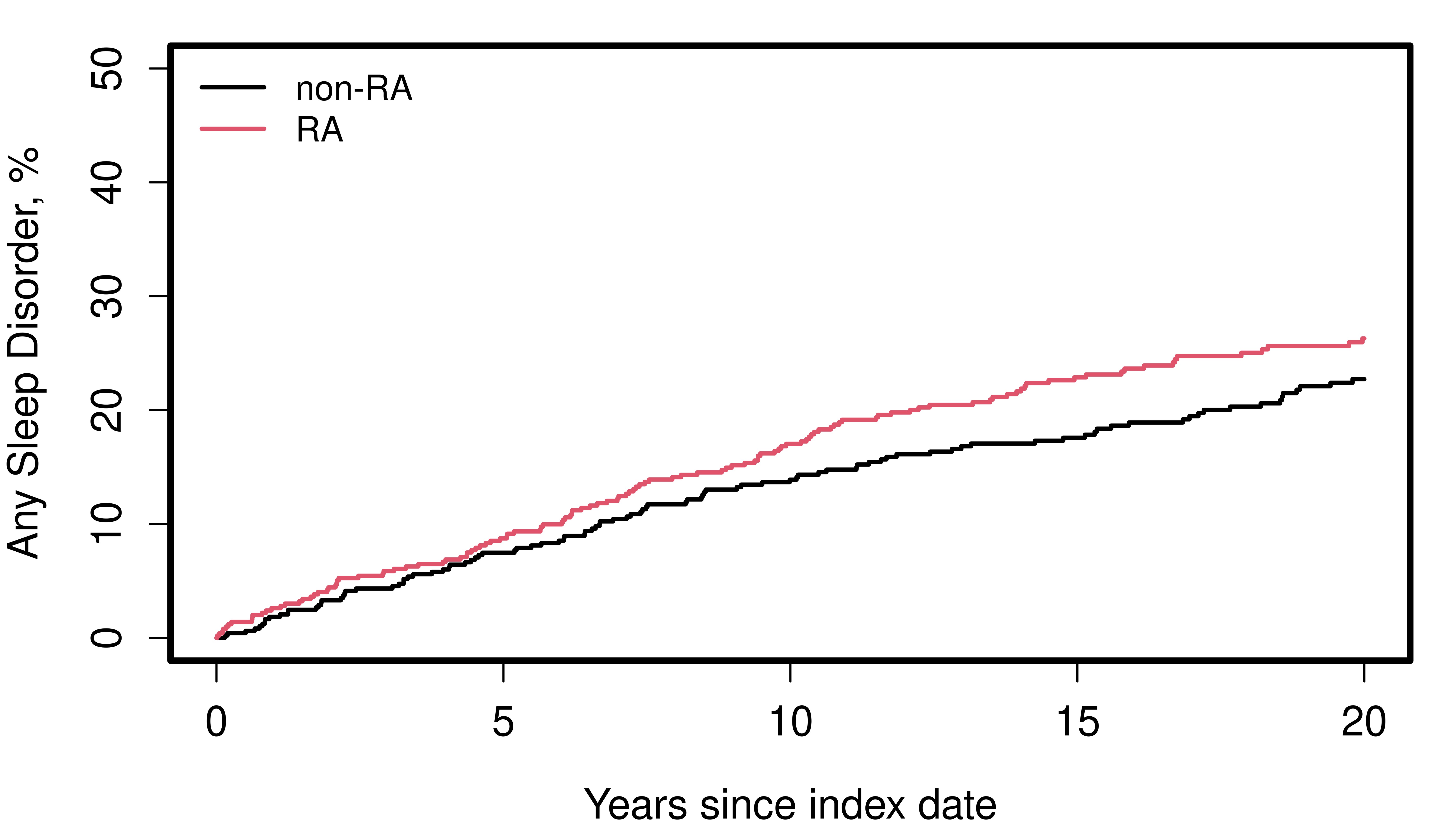
Results: A total of 573 patients with RA were studied (mean age 65.5 ±10.3 years, 66% female, 95% White, mean body mass index 28.1 ±6.1 kg/m2; 62% RF/Anti-CCP positive) along with 573 matched non-RA comparators. At RA incidence/index date, there were no differences in the prevalence of any SD in patients with RA vs non-RA controls (13% vs 14%, respectively) and by SD subtype: insomnia (6% vs 6%), OSA (7% vs 7%), RLS (2% vs 2%). During a median follow-up of 13.9 years in the RA cohort and 15.1 years in the non-RA cohort, SD developed in 129 patients with and 113 patients without RA. RA patients experienced a borderline increased risk for any SD (age- and sex-adjusted hazard ratio:1.29; 95% CI: 1.00-1.66, p=0.05) (Figure 1). The most common types of SD were OSA and insomnia.
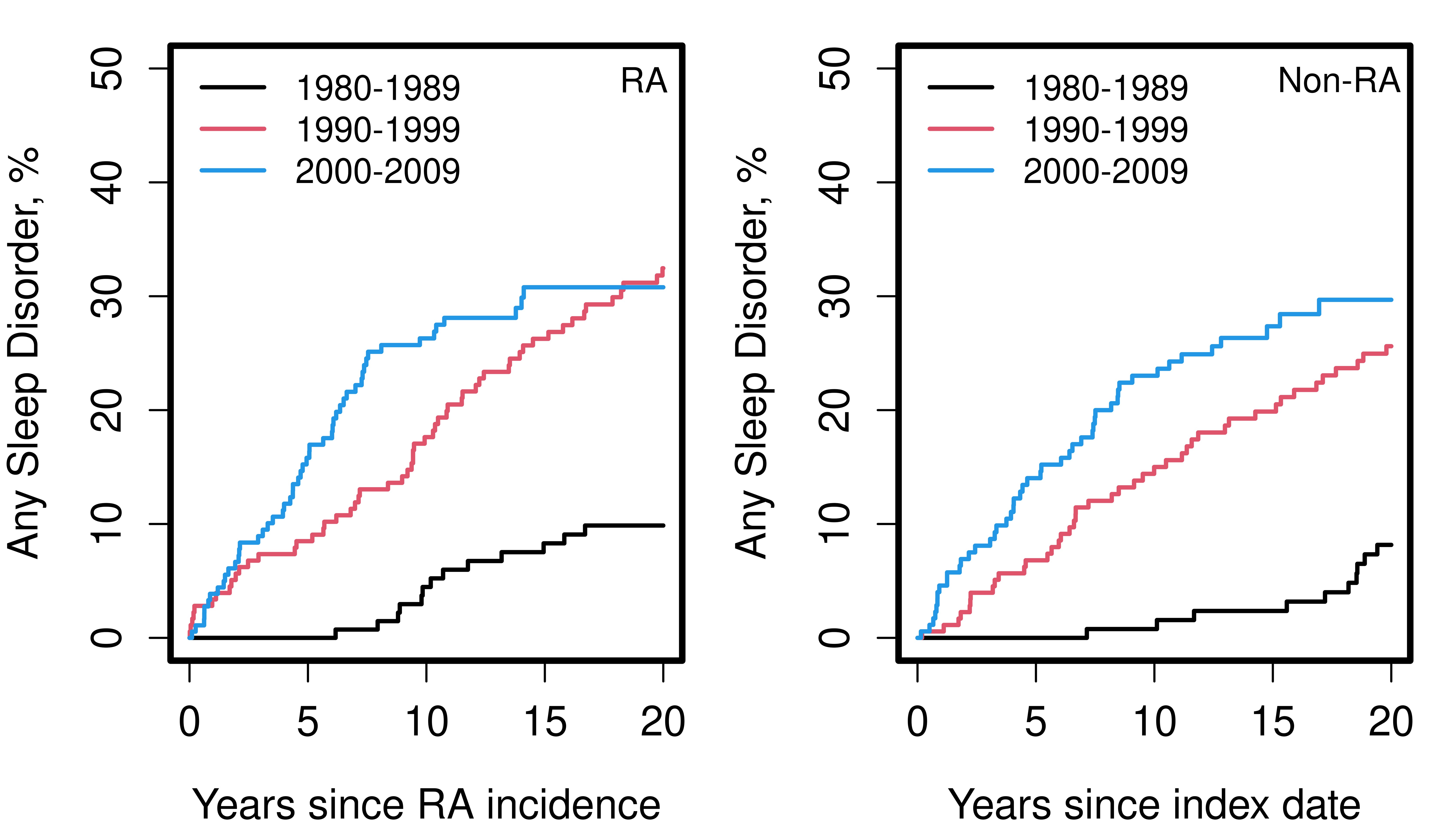
When comparing seropositive and seronegative patients with RA, there was no difference in the development of any SD (HR: 1.17; 0.82-1.67) or OSA (HR: 0.95; 95% CI: 0.59-1.54). However, seronegative patients were more likely to develop insomnia than seropositive patients (HR: 1.81; 95% CI: 1.09-3.03). This association persisted after adjusting for age, sex, smoking and obesity (HR 1.94, 95%CI 1.16-3.27). In addition, the incidence/diagnosis rate of SD increased over time by decade of RA incidence/index date (i.e., 1980-1989, 1990-1999, and 2000-2009) in both cohorts (Figure 2), and this association persisted even adjusting for age, sex, smoking status and obesity.
Conclusion: Our study findings indicate that RA patients tend to experience an increased risk for any SD after the index date. Patients with seronegative RA had significantly higher risk of insomnia compared to seropositive RA patients. The increased incidence rate of SD by decade of RA incidence/ index, likely reflects higher awareness and improved recognition of SD in more recent years. Further research is ongoing by our group to understand the underlying mechanisms for these associations, in order to inform preventive and management options for SD in patients with RA.
R. Kumar: None; E. Lovering: None; C. Kodishala: None; S. Achenbach: None; D. Carvalho: None; C. Crowson: None; J. Davis: Girihlet, 9, Pfizer, 5, Remission Medical, 9; E. Myasoedova: None.
Background/Purpose: Some sleep disorders (SD) are more prevalent in patients with chronic inflammatory diseases, such as Rheumatoid Arthritis (RA). However, most of the research has focused on obstructive sleep apnea (OSA), and less is known about other SD (i.e., insomnia, restless legs syndrome [RLS]). The incidence of SD over time is also not well understood. Therefore, we aimed to examine the incidence of sleep disorders in patients with RA vs comparators without RA over time and by serologic status.
Methods: This retrospective population-based cohort study included residents of a geographically defined area, aged ≥50 years when they met 1987 ACR criteria for incident RA in 1980-2009. All these patients were followed until death/migration or 12/31/2021 and matched 1:1 on age, sex, and calendar year with non-RA comparators. SD were identified based on two ICD 9/10-CM codes and data were abstracted via manual record review. Demographics, medical comorbidities, laboratory data on RA characteristics were collected. We investigated the association between RA and sleep disorders by using Cox models, adjusting for age and sex. P-value < 0.05 was considered significant. All analyses were performed using SAS version 9.4.
Results: A total of 573 patients with RA were studied (mean age 65.5 ±10.3 years, 66% female, 95% White, mean body mass index 28.1 ±6.1 kg/m2; 62% RF/Anti-CCP positive) along with 573 matched non-RA comparators. At RA incidence/index date, there were no differences in the prevalence of any SD in patients with RA vs non-RA controls (13% vs 14%, respectively) and by SD subtype: insomnia (6% vs 6%), OSA (7% vs 7%), RLS (2% vs 2%). During a median follow-up of 13.9 years in the RA cohort and 15.1 years in the non-RA cohort, SD developed in 129 patients with and 113 patients without RA. RA patients experienced a borderline increased risk for any SD (age- and sex-adjusted hazard ratio:1.29; 95% CI: 1.00-1.66, p=0.05) (Figure 1). The most common types of SD were OSA and insomnia.
When comparing seropositive and seronegative patients with RA, there was no difference in the development of any SD (HR: 1.17; 0.82-1.67) or OSA (HR: 0.95; 95% CI: 0.59-1.54). However, seronegative patients were more likely to develop insomnia than seropositive patients (HR: 1.81; 95% CI: 1.09-3.03). This association persisted after adjusting for age, sex, smoking and obesity (HR 1.94, 95%CI 1.16-3.27). In addition, the incidence/diagnosis rate of SD increased over time by decade of RA incidence/index date (i.e., 1980-1989, 1990-1999, and 2000-2009) in both cohorts (Figure 2), and this association persisted even adjusting for age, sex, smoking status and obesity.
Conclusion: Our study findings indicate that RA patients tend to experience an increased risk for any SD after the index date. Patients with seronegative RA had significantly higher risk of insomnia compared to seropositive RA patients. The increased incidence rate of SD by decade of RA incidence/ index, likely reflects higher awareness and improved recognition of SD in more recent years. Further research is ongoing by our group to understand the underlying mechanisms for these associations, in order to inform preventive and management options for SD in patients with RA.
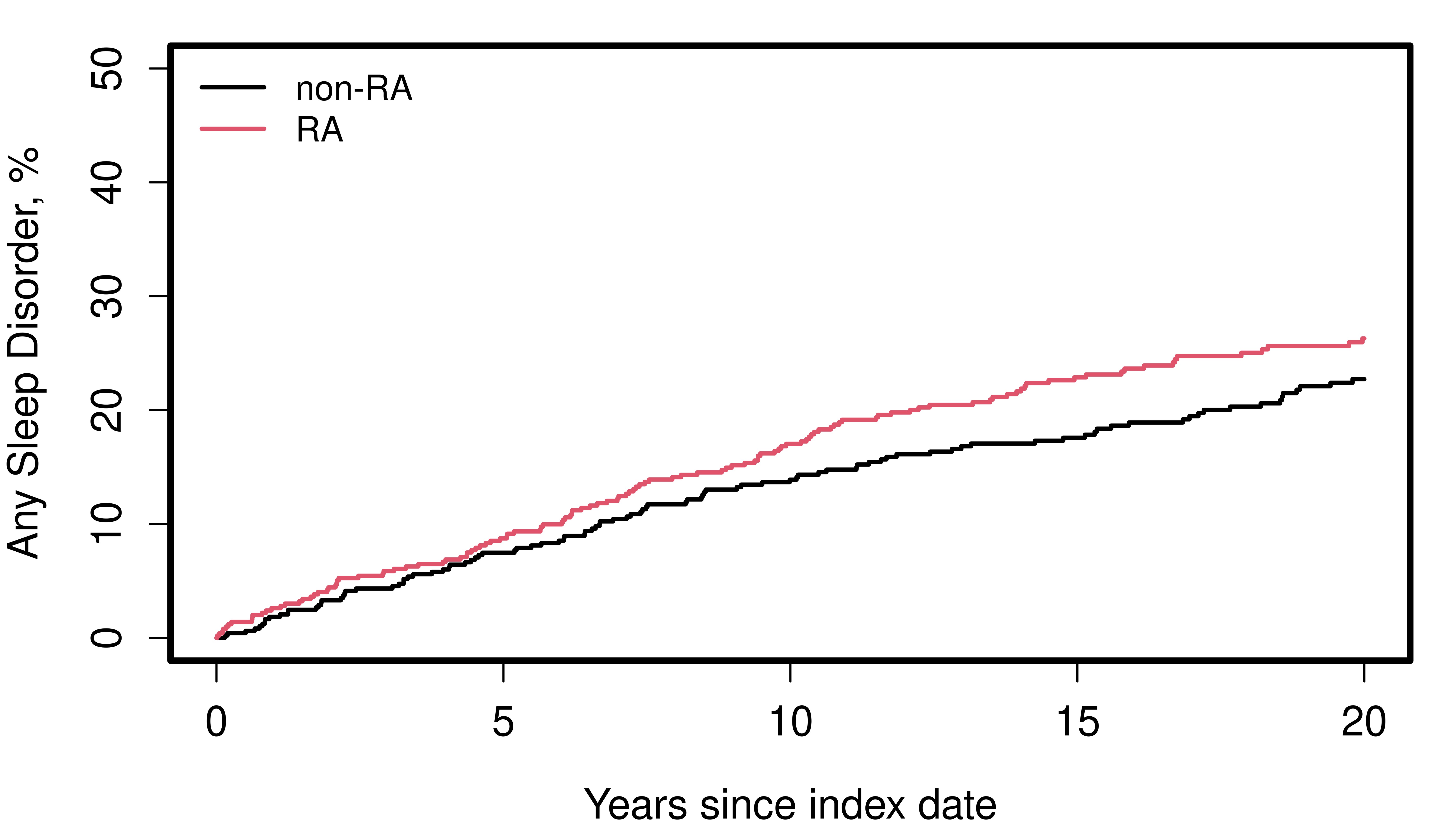
Figure 1. Cumulative incidence of sleep disorders in patients with incident RA in 1980-2009 vs non-RA comparators
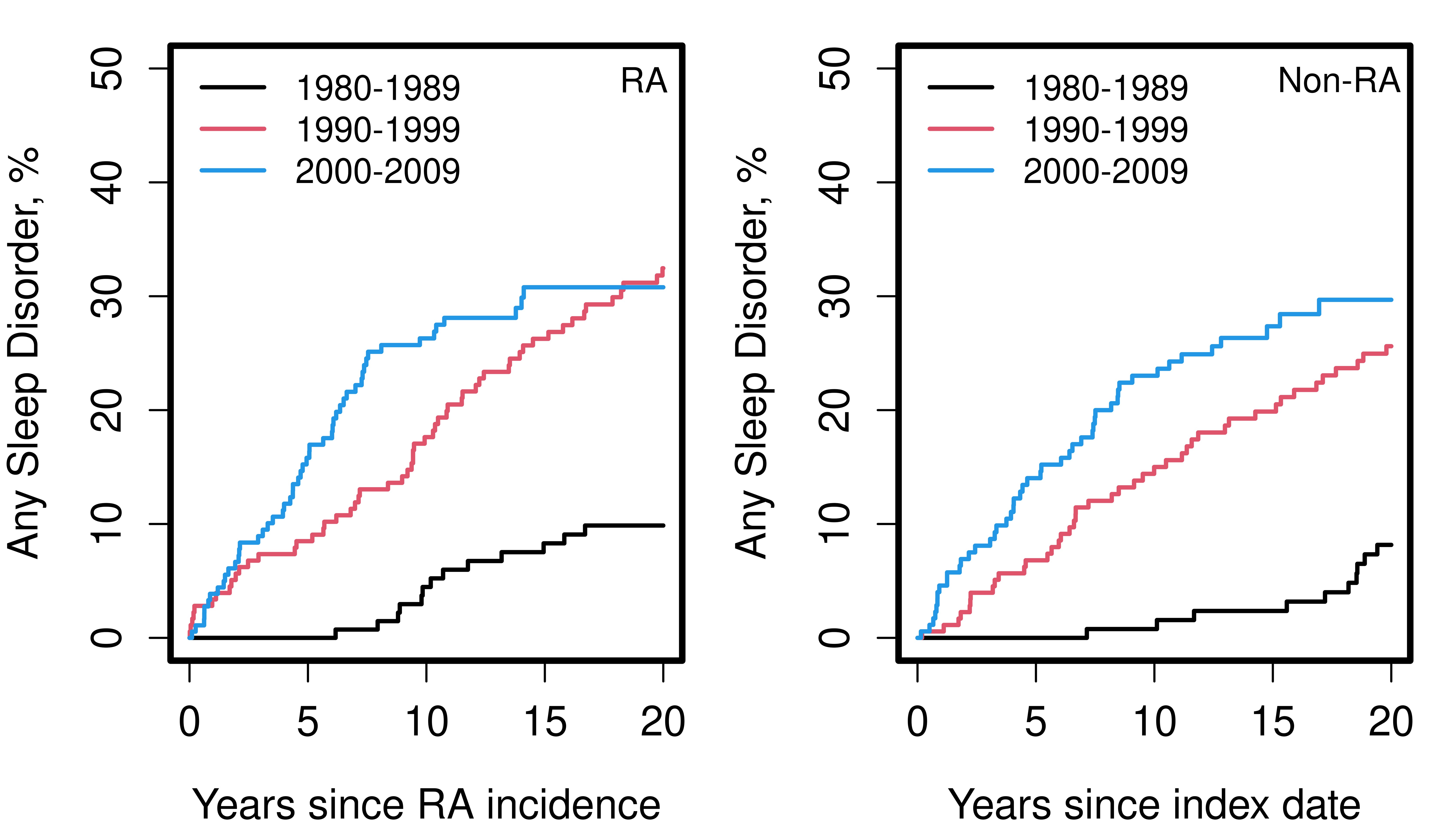
Figure 2. Cumulative incidence of sleep disorders in patients with incident RA in 1980-2009 vs non-RA comparators by decade
R. Kumar: None; E. Lovering: None; C. Kodishala: None; S. Achenbach: None; D. Carvalho: None; C. Crowson: None; J. Davis: Girihlet, 9, Pfizer, 5, Remission Medical, 9; E. Myasoedova: None.



