Poster Session A
Rheumatoid arthritis (RA)
Session: (0423–0459) RA – Treatment Poster I
0452: Real Life Safety and Survival of Targeted Therapies in Arthritis Patients over Age of 65
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- EG
Abstract Poster Presenter(s)
Elena Grau Garcia1, Pablo Francisco Muñoz Martínez2, Laura Mas Sanchez3, Alba Maria Torrat Noves1, Daniel Ramos Castro1, Carmen Riesco Barcena1, Anderson Victor Huaylla Quispe1, Iago Alcantara Alvarez1, Belen Villanueva Mañez1, Samuel Leal Rodriguez1, Ines Canovas Olmos1, Hikmat Charia1, Marta De la Rubia Navarro1, Luis Gonzalez Puig1, Jose Ivorra Cortes1, Isabel Martinez Cordellat1, Carmen Najera Herranz1, Rosa Negueroles Albuixech1, Jose Eloy Oller Rodriguez1, Ernesto Tovar Sugrañes1, Elvira Vicens Bernabeu1 and Jose Andres Roman Ivorra4, 1Rheumatology Department. HUP La Fe, Valencia, Spain, 2Rheumatology Department. HUP La Fe, Sagunto, Spain, 3Rheumatology Department. HUP La Fe, Valéncia, Spain, 4Hospital Universitari i Politècnic la Fe, Valencia, Spain
Background/Purpose: Prognosis for chronic inflammatory arthritis is drastically improved over previous decades and older patients are treated with targeted therapies (TTs) (biological or synthetic targeted therapies). Clinical trials provide mainly information about TTs in patients below the age of 65, so real-life studies are needed to provide more information about TTs in patients over 65 years of age.
The aim of the present study was to compare clinical and therapeutic profile of arthritis patients undergoing TTs and to analyze safety and therapeutic survival according to different age groups.
Methods: We performed an observational cross-sectional study in rheumatoid arthritis (RA), psoriatic arthritis (PsA) and ankylosing spondylitis (AS) patients, older than 40 years old, who started biological or anti-JAK therapy between 2000 and 2022. A comparative analysis and a Kaplan-Meier survival analysis was performed.
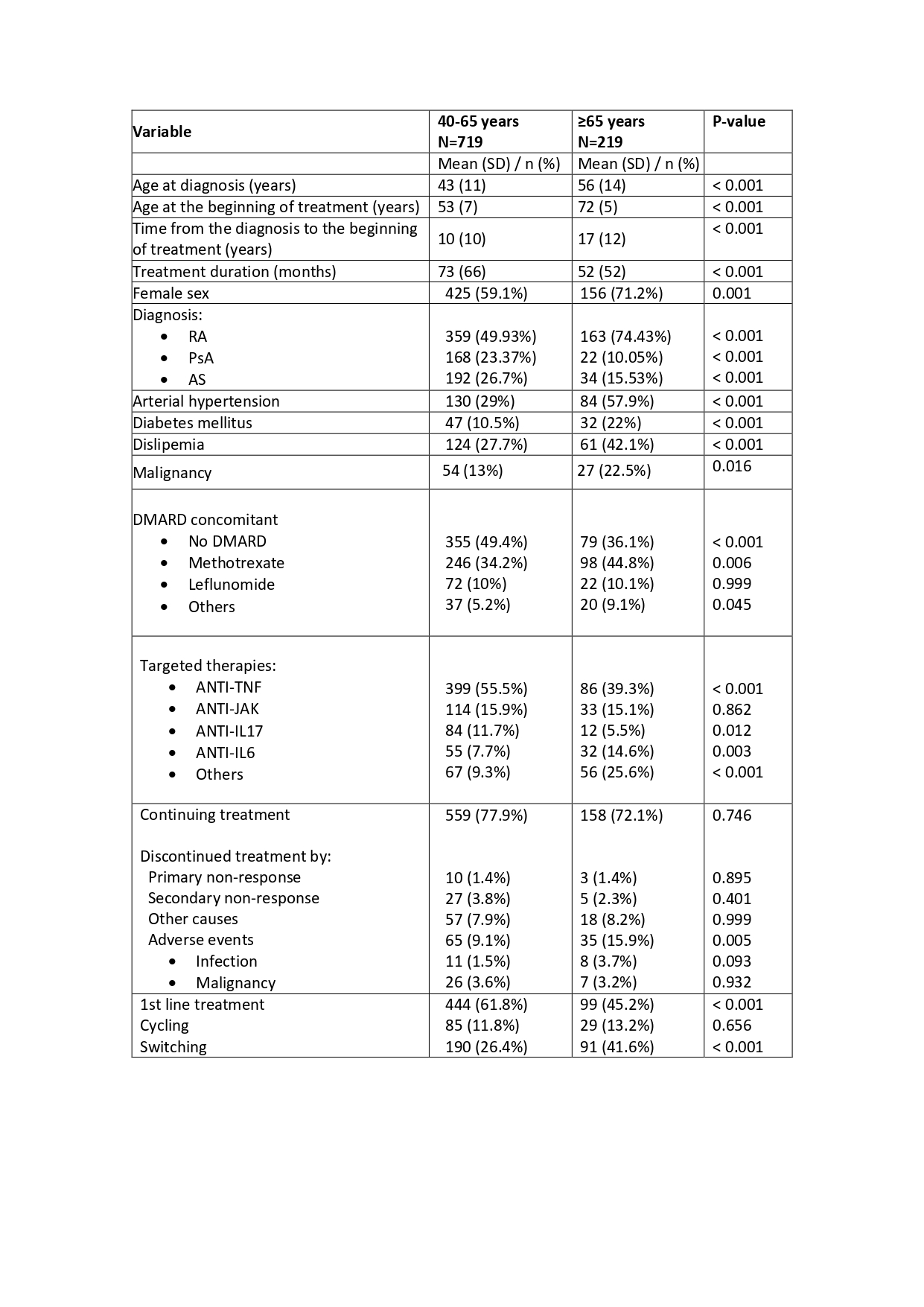
Results: 938 patients (62% female) were included in the study, of which 20.3% are PsA, 55.6% RA and 24.1% AS, with a mean age at the beginning of treatment of 57 (10) years and a mean duration of treatment of 68 (64) months. Patients were classified according to the age at the beginning of treatment: 40-65 years and ≥ 65 years of age. 219 patients (23.3%) were over 65 years of age. In table1 we show the comparative analysis between both groups.
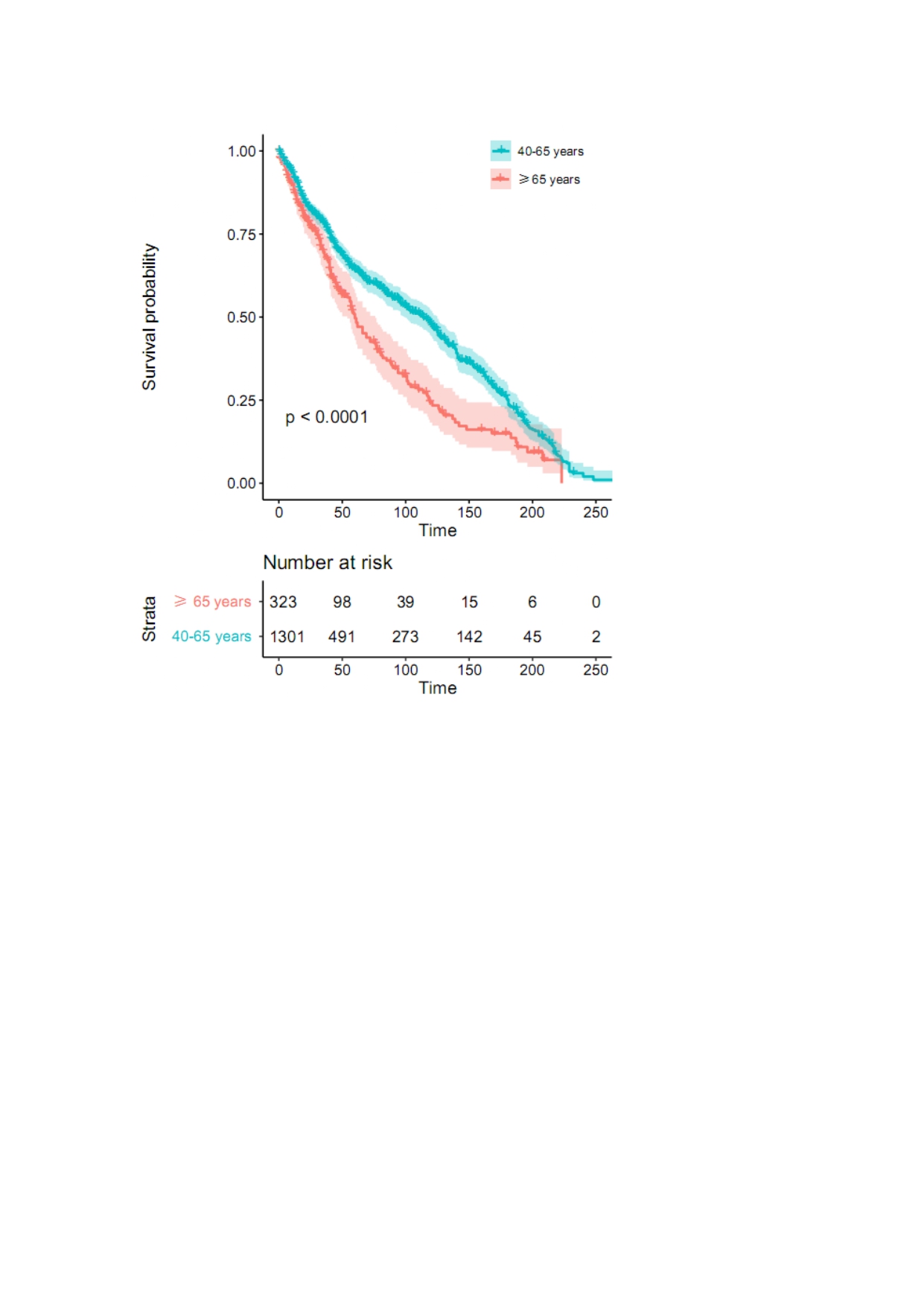
Higher proportion of arterial hypertension, diabetes mellitus and dislipemia in patients older than 65 years was observed. Using a logistic regression model, an association between conventional DMARD prescription and patients older than 65 years was found (P< 0.001), being the methotrexate the most used (44.8%). Anti-TNF therapy was the most extended treatment in both groups of patients, and an association between anti-IL6 therapy and older patients than 65 years was observed (P< 0.001). Previous TTs were more frequent in older patients (P=0.002) and treatment duration was lower in those patients (P< 0.001) (figure1). Adverse events were more commonly found in patients older than 65 years as the reason to TT discontinue (P=0.008), being infections the more frequent.
Conclusion: The use of conventional DMARDs and lower therapeutic survival are more frequent in patients older than 65 years of age.
Adverse events were the main reason of treatment suspension in these patients, with a higher proportion of infections among them in contrast to patients under 65 years old.
E. Grau Garcia: None; P. Muñoz Martínez: None; L. Mas Sanchez: None; A. Torrat Noves: None; D. Ramos Castro: None; C. Riesco Barcena: None; A. Huaylla Quispe: None; I. Alcantara Alvarez: None; B. Villanueva Mañez: None; S. Leal Rodriguez: None; I. Canovas Olmos: None; H. Charia: None; M. De la Rubia Navarro: None; L. Gonzalez Puig: None; J. Ivorra Cortes: None; I. Martinez Cordellat: None; C. Najera Herranz: None; R. Negueroles Albuixech: None; J. Oller Rodriguez: None; E. Tovar Sugrañes: None; E. Vicens Bernabeu: None; J. Roman Ivorra: None.
Background/Purpose: Prognosis for chronic inflammatory arthritis is drastically improved over previous decades and older patients are treated with targeted therapies (TTs) (biological or synthetic targeted therapies). Clinical trials provide mainly information about TTs in patients below the age of 65, so real-life studies are needed to provide more information about TTs in patients over 65 years of age.
The aim of the present study was to compare clinical and therapeutic profile of arthritis patients undergoing TTs and to analyze safety and therapeutic survival according to different age groups.
Methods: We performed an observational cross-sectional study in rheumatoid arthritis (RA), psoriatic arthritis (PsA) and ankylosing spondylitis (AS) patients, older than 40 years old, who started biological or anti-JAK therapy between 2000 and 2022. A comparative analysis and a Kaplan-Meier survival analysis was performed.
Results: 938 patients (62% female) were included in the study, of which 20.3% are PsA, 55.6% RA and 24.1% AS, with a mean age at the beginning of treatment of 57 (10) years and a mean duration of treatment of 68 (64) months. Patients were classified according to the age at the beginning of treatment: 40-65 years and ≥ 65 years of age. 219 patients (23.3%) were over 65 years of age. In table1 we show the comparative analysis between both groups.
Higher proportion of arterial hypertension, diabetes mellitus and dislipemia in patients older than 65 years was observed. Using a logistic regression model, an association between conventional DMARD prescription and patients older than 65 years was found (P< 0.001), being the methotrexate the most used (44.8%). Anti-TNF therapy was the most extended treatment in both groups of patients, and an association between anti-IL6 therapy and older patients than 65 years was observed (P< 0.001). Previous TTs were more frequent in older patients (P=0.002) and treatment duration was lower in those patients (P< 0.001) (figure1). Adverse events were more commonly found in patients older than 65 years as the reason to TT discontinue (P=0.008), being infections the more frequent.
Conclusion: The use of conventional DMARDs and lower therapeutic survival are more frequent in patients older than 65 years of age.
Adverse events were the main reason of treatment suspension in these patients, with a higher proportion of infections among them in contrast to patients under 65 years old.
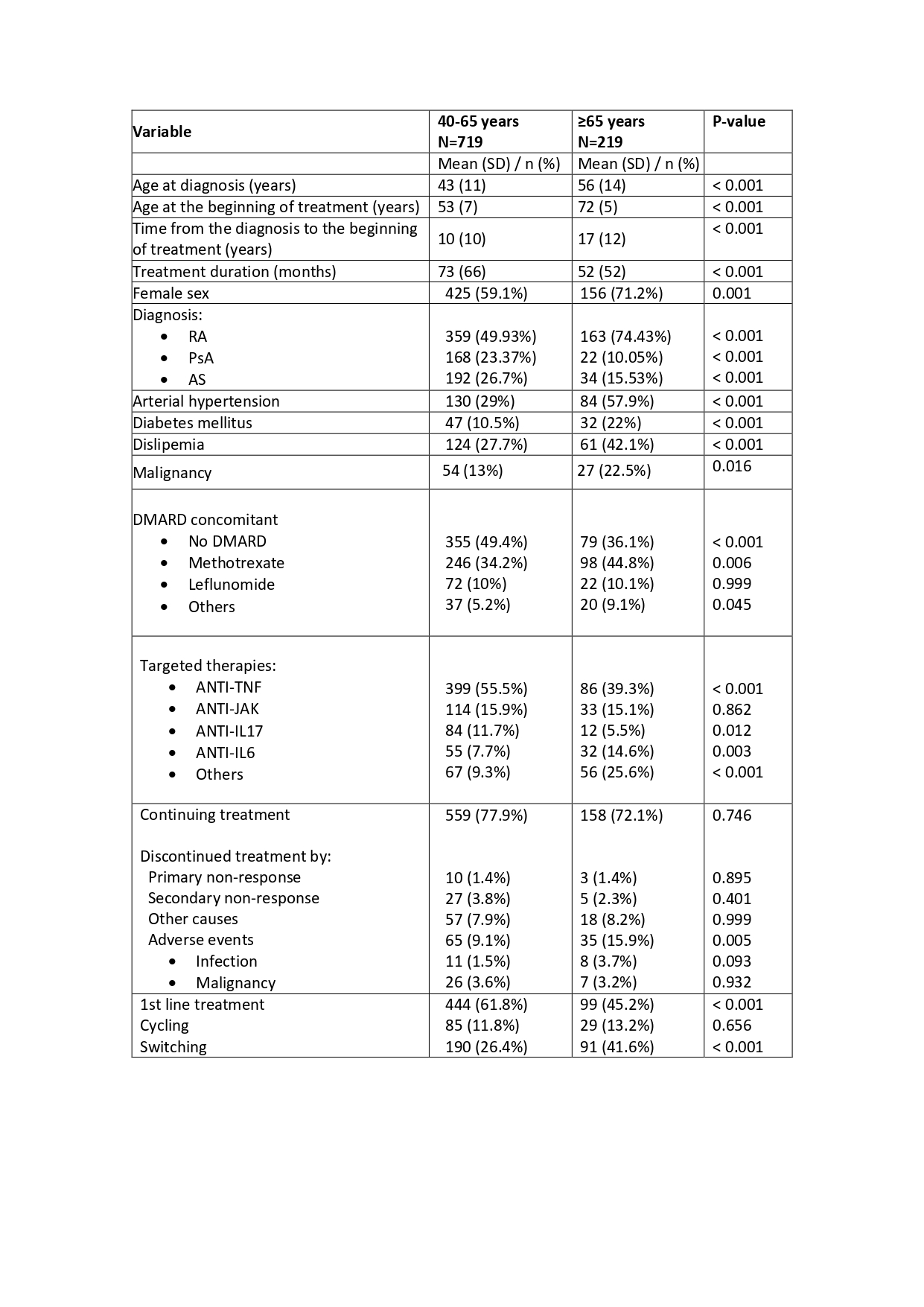
Table1. Comparative analysis of clinical profile of different age groups at the beginning of TTs.
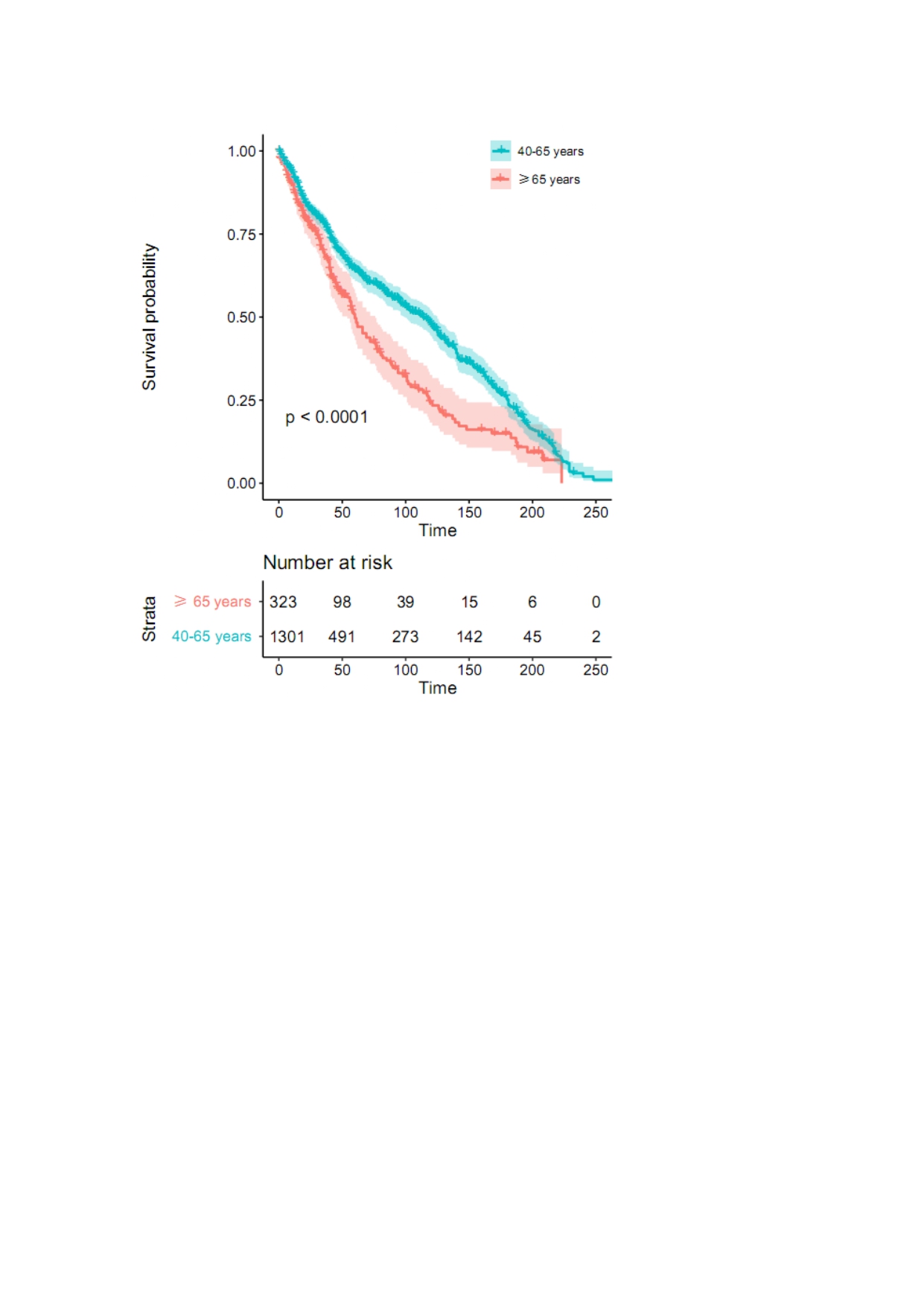
Figure 1
E. Grau Garcia: None; P. Muñoz Martínez: None; L. Mas Sanchez: None; A. Torrat Noves: None; D. Ramos Castro: None; C. Riesco Barcena: None; A. Huaylla Quispe: None; I. Alcantara Alvarez: None; B. Villanueva Mañez: None; S. Leal Rodriguez: None; I. Canovas Olmos: None; H. Charia: None; M. De la Rubia Navarro: None; L. Gonzalez Puig: None; J. Ivorra Cortes: None; I. Martinez Cordellat: None; C. Najera Herranz: None; R. Negueroles Albuixech: None; J. Oller Rodriguez: None; E. Tovar Sugrañes: None; E. Vicens Bernabeu: None; J. Roman Ivorra: None.



