Poster Session A
Systemic lupus erythematosus (SLE)
Session: (0543–0581) SLE – Diagnosis, Manifestations, & Outcomes Poster I
0567: N-Terminal Pro-Brain Natriuretic Peptide Correlates Strongly with Cardiovascular Damage in Systemic Lupus Erythematous (SLE): A Cross-sectional Study
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- AM
Arielle Mendel, MD, FRCPC, MSc
McGill University Health Centre
Montréal, QC, CanadaDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Karim Sacre1, Evelyne Vinet2, Christian Pineau2, Arielle Mendel3, Fares Kalache3, Louis Pierre Grenier3, Thao Huynh3 and Sasha Bernatsky4, 1Université Paris Cité, Paris, France, 2McGill University Health Centre, Montréal, QC, Canada, 3McGill University Health Centre, Montreal, QC, Canada, 4Research Institute of the McGill University Health Centre, Montreal, QC, Canada
Background/Purpose: Cardiovascular (CV) disease represents the leading cause of death in SLE. Traditional risk factors are less accurate at identifying cardiovascular risk in SLE than in the general population. N-Terminal pro-Brain Natriuretic Peptide (NT-proBNP) is a key biomarker to detect heart disease and predict cardiac outcomes, in non-lupus populations. We assessed NT-proBNP in a large cross-sectional sample of unselected SLE patients and investigated associations with CV damage.
Methods: Adults meeting ACR SLE classification have been consecutively enrolled in our Lupus Clinic cohort. Patients were followed yearly with evaluations of drugs, SLICC Damage Index (SDI), SLEDAI-2K, and other measures including cardiovascular risk factors. NT-proBNP (pg/mL) levels were measured in serum collected at annual research visits between March 2022 and April 2023. The main outcome was CV damage defined as any CV SDI events. Cross-sectional associations between NT-proBNP and this outcome were evaluated using multivariable logistic regression model.
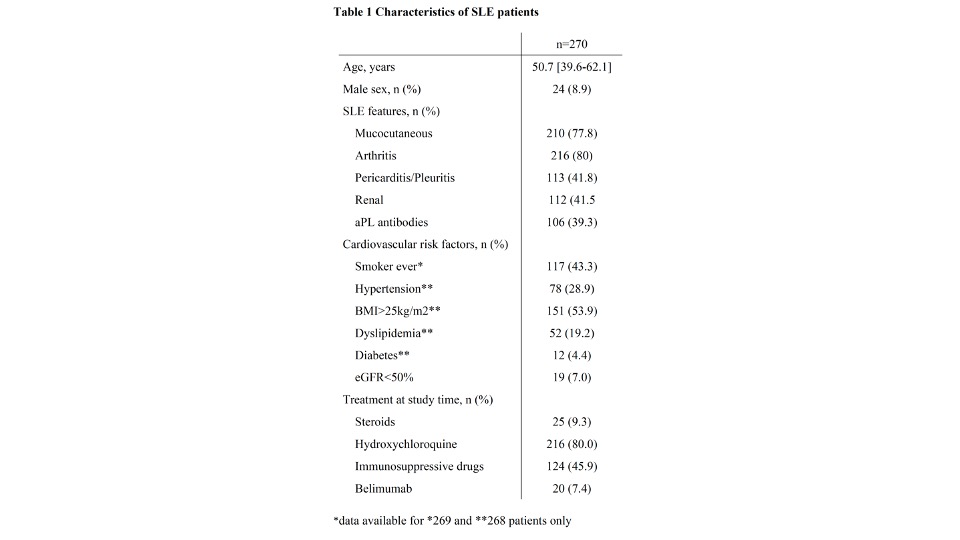
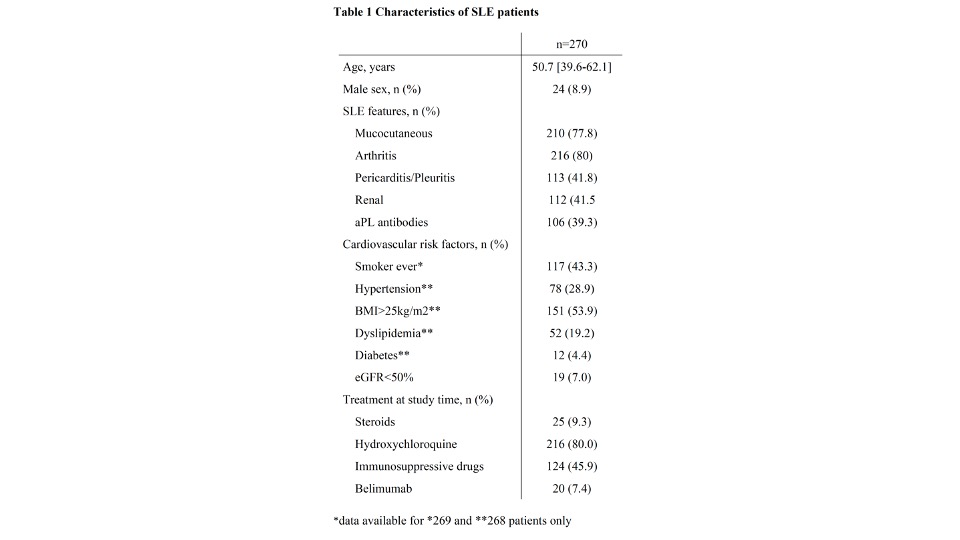
Results: Overall, 270 SLE patients (91% female 91%, median age of 50.7 [1st quartile- 3rd quartile: 39.6-62.1] years) from the MUHC cohort were included. At NT-proBNP assessment, median disease duration was 17.7 years [11.6-27.2] and median SLEDAI-2K and SDI scores were 2 [0-4] and 1 [0-3] respectively. Characteristics of patients are given in Table 1. Thirty-three (12%) patients had CV damage including coronary artery disease (n=14), cerebral vascular accident (n=12), chronic pericarditis (n=6), valvular diseases (n=5), cardiomyopathy (n=3) and peripheral artery disease (n=1). The median [1stquartile- 3rd quartile] NT-proBNP serum level was 95 [54-185] pg/mL. NT-proBNP levels were higher in patients with CV damage (281 [140-856] versus 84 [50-147] pg/mL in those without CV damage, P< 0.001) and were especially high in patients with more than one CV damage item (989 pg/mL [734–1725] versus 194 [122-327] pg/mL in those with one CV damage item only, P< 0.0001). The ROC curve for NT-proBNP demonstrated strong associations with CV damage (AUC 0.78, 95% CI 0.69-0.87). The threshold providing the best discrimination for those with/without CVD was 133 pg/mL, with a sensitivity of 79% (95% CI 64-91) and a specificity of 70% (95% CI 64-76). In multivariate analyses, hypertension (OR 3.3, 95% C 1.2-9.0), dyslipidemia (OR 3.6, 95% CI 1.3-9.6) and NT-proBNP >133 pg/mL (OR 7.0, 95% CI, 2.6-19.1) were strongly associated with CV damage. CV damage was less frequent in SLE patients on hydroxychloroquine (OR 0.3, 95% CI 0.1-0.8). Increased NT-proBNP levels were themselves associated with age (OR 4.2, 95% CI 2.2-8.3), smoking (OR 1.9, 95% CI 1.0-3.5), reduced eGFR (4.1, 95% CI 1.3-13.1), prior pericarditis/pleuritis (OR 2.5, 95% CI 1.4-4.5) and aPL antibodies (OR 2.6, 95% CI 1.4-4.9)
Conclusion: Serum NT-proBNP levels correlate with CV damage in SLE. Future evaluations are needed to identify the usefulness of NT-proBNP in tailoring treatments to prevent CV burden in SLE. The novel associations of NT-proBNP levels with pericarditis/pleuritis and aPL antibodies suggest new avenues for research to better understand what drives CV risk in SLE.
K. Sacre: None; E. Vinet: None; C. Pineau: None; A. Mendel: None; F. Kalache: None; L. Grenier: None; T. Huynh: None; S. Bernatsky: None.
Background/Purpose: Cardiovascular (CV) disease represents the leading cause of death in SLE. Traditional risk factors are less accurate at identifying cardiovascular risk in SLE than in the general population. N-Terminal pro-Brain Natriuretic Peptide (NT-proBNP) is a key biomarker to detect heart disease and predict cardiac outcomes, in non-lupus populations. We assessed NT-proBNP in a large cross-sectional sample of unselected SLE patients and investigated associations with CV damage.
Methods: Adults meeting ACR SLE classification have been consecutively enrolled in our Lupus Clinic cohort. Patients were followed yearly with evaluations of drugs, SLICC Damage Index (SDI), SLEDAI-2K, and other measures including cardiovascular risk factors. NT-proBNP (pg/mL) levels were measured in serum collected at annual research visits between March 2022 and April 2023. The main outcome was CV damage defined as any CV SDI events. Cross-sectional associations between NT-proBNP and this outcome were evaluated using multivariable logistic regression model.
Results: Overall, 270 SLE patients (91% female 91%, median age of 50.7 [1st quartile- 3rd quartile: 39.6-62.1] years) from the MUHC cohort were included. At NT-proBNP assessment, median disease duration was 17.7 years [11.6-27.2] and median SLEDAI-2K and SDI scores were 2 [0-4] and 1 [0-3] respectively. Characteristics of patients are given in Table 1. Thirty-three (12%) patients had CV damage including coronary artery disease (n=14), cerebral vascular accident (n=12), chronic pericarditis (n=6), valvular diseases (n=5), cardiomyopathy (n=3) and peripheral artery disease (n=1). The median [1stquartile- 3rd quartile] NT-proBNP serum level was 95 [54-185] pg/mL. NT-proBNP levels were higher in patients with CV damage (281 [140-856] versus 84 [50-147] pg/mL in those without CV damage, P< 0.001) and were especially high in patients with more than one CV damage item (989 pg/mL [734–1725] versus 194 [122-327] pg/mL in those with one CV damage item only, P< 0.0001). The ROC curve for NT-proBNP demonstrated strong associations with CV damage (AUC 0.78, 95% CI 0.69-0.87). The threshold providing the best discrimination for those with/without CVD was 133 pg/mL, with a sensitivity of 79% (95% CI 64-91) and a specificity of 70% (95% CI 64-76). In multivariate analyses, hypertension (OR 3.3, 95% C 1.2-9.0), dyslipidemia (OR 3.6, 95% CI 1.3-9.6) and NT-proBNP >133 pg/mL (OR 7.0, 95% CI, 2.6-19.1) were strongly associated with CV damage. CV damage was less frequent in SLE patients on hydroxychloroquine (OR 0.3, 95% CI 0.1-0.8). Increased NT-proBNP levels were themselves associated with age (OR 4.2, 95% CI 2.2-8.3), smoking (OR 1.9, 95% CI 1.0-3.5), reduced eGFR (4.1, 95% CI 1.3-13.1), prior pericarditis/pleuritis (OR 2.5, 95% CI 1.4-4.5) and aPL antibodies (OR 2.6, 95% CI 1.4-4.9)
Conclusion: Serum NT-proBNP levels correlate with CV damage in SLE. Future evaluations are needed to identify the usefulness of NT-proBNP in tailoring treatments to prevent CV burden in SLE. The novel associations of NT-proBNP levels with pericarditis/pleuritis and aPL antibodies suggest new avenues for research to better understand what drives CV risk in SLE.
K. Sacre: None; E. Vinet: None; C. Pineau: None; A. Mendel: None; F. Kalache: None; L. Grenier: None; T. Huynh: None; S. Bernatsky: None.



