Poster Session A
Systemic lupus erythematosus (SLE)
Session: (0543–0581) SLE – Diagnosis, Manifestations, & Outcomes Poster I
0564: Risk Factors for Immune Thrombocytopenia in Systemic Lupus Erythematosus and Generation of a Predictive Model to Assess Its Risk of Development
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- IC
Abstract Poster Presenter(s)
Irene Carrión-Barberà1, Jesús Cornudella Lema2, Sergio Vázquez Montes de Oca3, Francesc García Pallarols1, Jordi Monfort1, Blanca Sánchez-González1 and TAREK CARLOS SALMAN MONTE4, 1Hospital del Mar, Barcelona, Spain, 2Faculty of Medicine, Pompeu Fabra University, Barcelona, Spain and Faculty of Medicine, Autonomous University of Barcelona, Barcelona, Spain, 3Biomedical Informatics Research Group, IMIM, Barcelona, Spain, 4Hospital del Mar/Parc de Salut Mar-IMIM, Barcelona, Spain
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune disease with a wide variety of manifestations including immune thrombocytopenia (ITP), which has been described in 7-40% of SLE patients.
The aims of our study are to determine the prevalence of ITP in the cohort of patients with SLE from Hospital del Mar, to identify those risk factors associated with its development, and to build a predictive model capable of evaluating the risk of suffering ITP in these patients.
Methods: A case-control study was conducted in which 407 medical records of patients with SLE were reviewed. 34 had developed ITP (cases) and were matched by sex and age with 2 controls with SLE without ITP.
To build the model, the cases whose ITP was posterior to SLE diagnosis and their controls were selected. The model consists of a Random Forest run on a cohort of 66 patients. The variables used were those that showed the greatest disparity in frequency of appearance between both groups. The model was trained with 70% of the cohort and tested with the remaining 30%. The scores obtained were calculated by means of the average of the results obtained after 1000 executions.
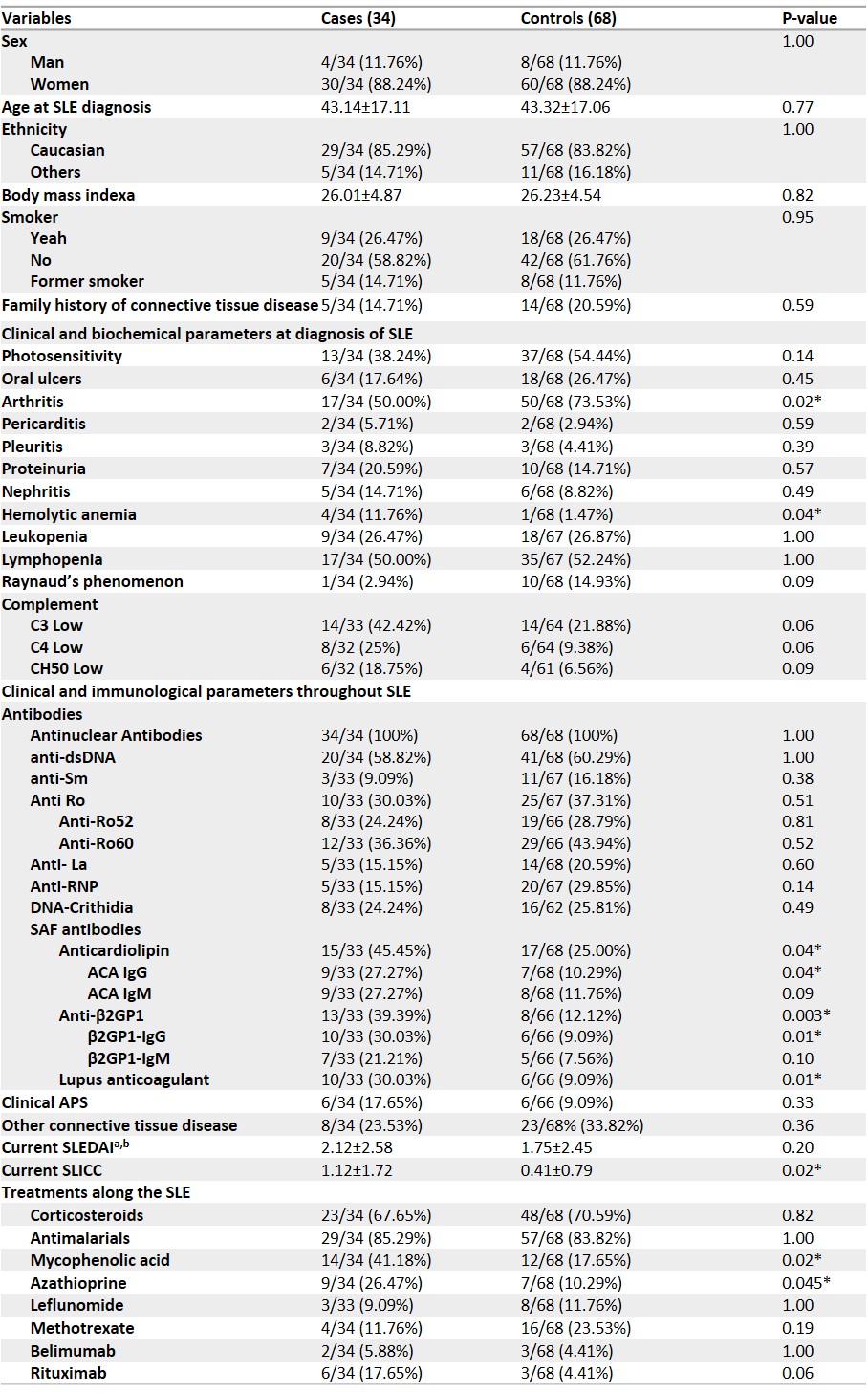
Results: Table 1 describes the characteristics and differences between cases and controls and Figure 1 the characteristics used to build the model. The prevalence of ITP in our cohort was 8.35% and it was diagnosed at an age of 43.14 ± 17.11 years. No significant differences were found in demographic variables between groups. At the diagnosis of SLE, controls presented a higher prevalence of arthritis (p-val = 0.02), while cases presented a higher proportion of hemolytic anemia (p-val = 0.04). Throughout the disease, cases presented a greater presence of lupus anticoagulant (p-val = 0.01), anticardiolipin (p-val = 0.044) and anti-β2-glycoprotein 1 antibodies (anti-β2GP1) (p-val = 0.003). In turn, cases had a significantly higher SLICC than controls (p-val = 0.02). Regarding treatment, cases received mycophenolic acid (MPA) (p-val = 0.02) and azathioprine (AZA) (p-val = 0.045) more frequently.
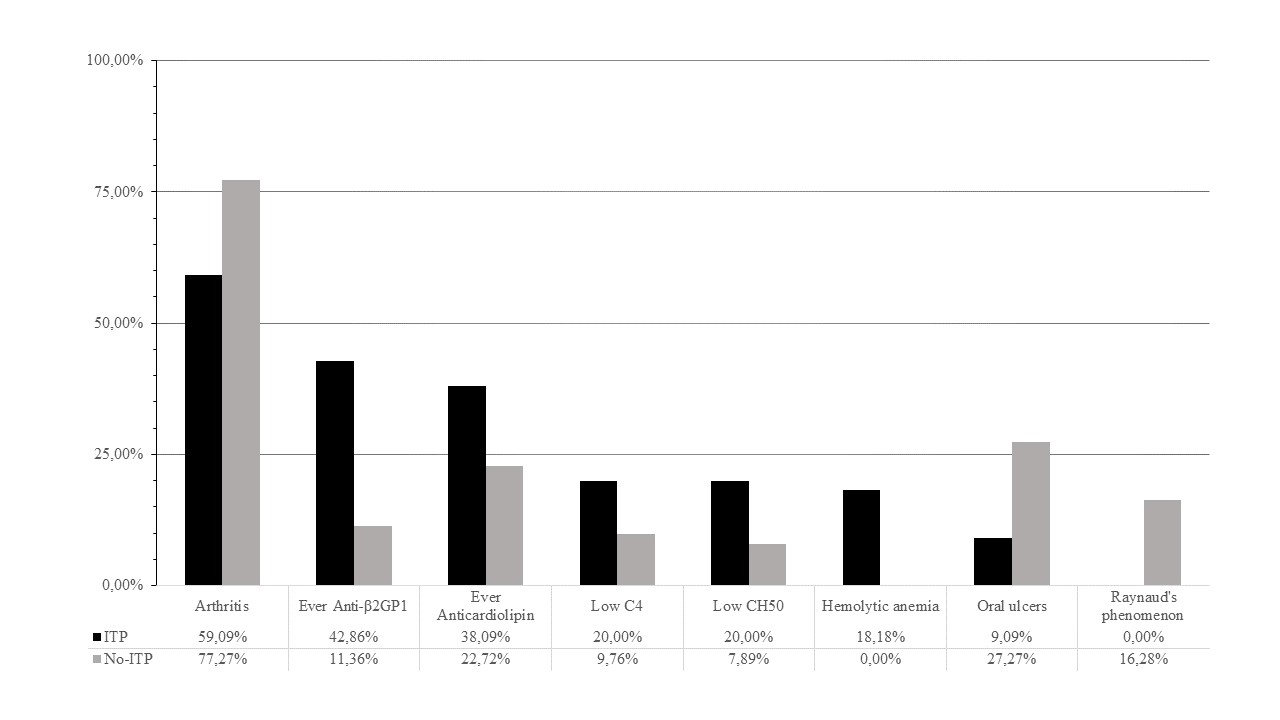
The variables that showed the most disparity and importance for the model were hemolytic anemia, low C4, low C50, anticardiolipin and anti-β2GP1, which were more frequent in cases, and oral ulcers, arthritis and Raynaud's phenomenon (RP) in controls.
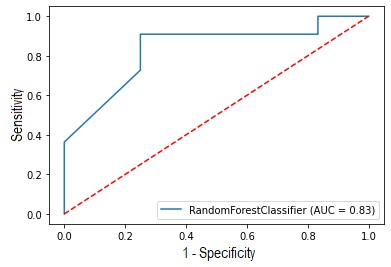
The model presented a sensitivity of 87.53%, a positive predictive value of 81.92%, a specificity of 80.50%, an area under the curve (AUC) of 83.92% (Figure 2), and an accuracy of 83.68%.
Conclusion: Patients with SLE who develop ITP seem to have a different phenotype than those who do not, presenting with less arthritis and more hemolytic anemia at diagnosis, as well as higher positivity for antiphospholipid syndrome antibodies throughout the disease. Having developed ITP was associated with higher SLICC and receiving treatment more frequently with MPA and AZA, probably indicating a more severe disease.
We have created a predictive model capable of evaluating the risk of developing ITP in patients with SLE. By combining 8 variables (hemolytic anemia, low C4, low C50, anticardiolipin, anti-β2GP1, oral ulcers, arthritis, and RP), the model correctly predicts 87.53% of patients with SLE who will develop ITP with an accuracy of 83.68%.
I. Carrión-Barberà: None; J. Cornudella Lema: None; S. Vázquez Montes de Oca: None; F. García Pallarols: None; J. Monfort: None; B. Sánchez-González: None; T. SALMAN MONTE: None.
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune disease with a wide variety of manifestations including immune thrombocytopenia (ITP), which has been described in 7-40% of SLE patients.
The aims of our study are to determine the prevalence of ITP in the cohort of patients with SLE from Hospital del Mar, to identify those risk factors associated with its development, and to build a predictive model capable of evaluating the risk of suffering ITP in these patients.
Methods: A case-control study was conducted in which 407 medical records of patients with SLE were reviewed. 34 had developed ITP (cases) and were matched by sex and age with 2 controls with SLE without ITP.
To build the model, the cases whose ITP was posterior to SLE diagnosis and their controls were selected. The model consists of a Random Forest run on a cohort of 66 patients. The variables used were those that showed the greatest disparity in frequency of appearance between both groups. The model was trained with 70% of the cohort and tested with the remaining 30%. The scores obtained were calculated by means of the average of the results obtained after 1000 executions.
Results: Table 1 describes the characteristics and differences between cases and controls and Figure 1 the characteristics used to build the model. The prevalence of ITP in our cohort was 8.35% and it was diagnosed at an age of 43.14 ± 17.11 years. No significant differences were found in demographic variables between groups. At the diagnosis of SLE, controls presented a higher prevalence of arthritis (p-val = 0.02), while cases presented a higher proportion of hemolytic anemia (p-val = 0.04). Throughout the disease, cases presented a greater presence of lupus anticoagulant (p-val = 0.01), anticardiolipin (p-val = 0.044) and anti-β2-glycoprotein 1 antibodies (anti-β2GP1) (p-val = 0.003). In turn, cases had a significantly higher SLICC than controls (p-val = 0.02). Regarding treatment, cases received mycophenolic acid (MPA) (p-val = 0.02) and azathioprine (AZA) (p-val = 0.045) more frequently.
The variables that showed the most disparity and importance for the model were hemolytic anemia, low C4, low C50, anticardiolipin and anti-β2GP1, which were more frequent in cases, and oral ulcers, arthritis and Raynaud's phenomenon (RP) in controls.
The model presented a sensitivity of 87.53%, a positive predictive value of 81.92%, a specificity of 80.50%, an area under the curve (AUC) of 83.92% (Figure 2), and an accuracy of 83.68%.
Conclusion: Patients with SLE who develop ITP seem to have a different phenotype than those who do not, presenting with less arthritis and more hemolytic anemia at diagnosis, as well as higher positivity for antiphospholipid syndrome antibodies throughout the disease. Having developed ITP was associated with higher SLICC and receiving treatment more frequently with MPA and AZA, probably indicating a more severe disease.
We have created a predictive model capable of evaluating the risk of developing ITP in patients with SLE. By combining 8 variables (hemolytic anemia, low C4, low C50, anticardiolipin, anti-β2GP1, oral ulcers, arthritis, and RP), the model correctly predicts 87.53% of patients with SLE who will develop ITP with an accuracy of 83.68%.
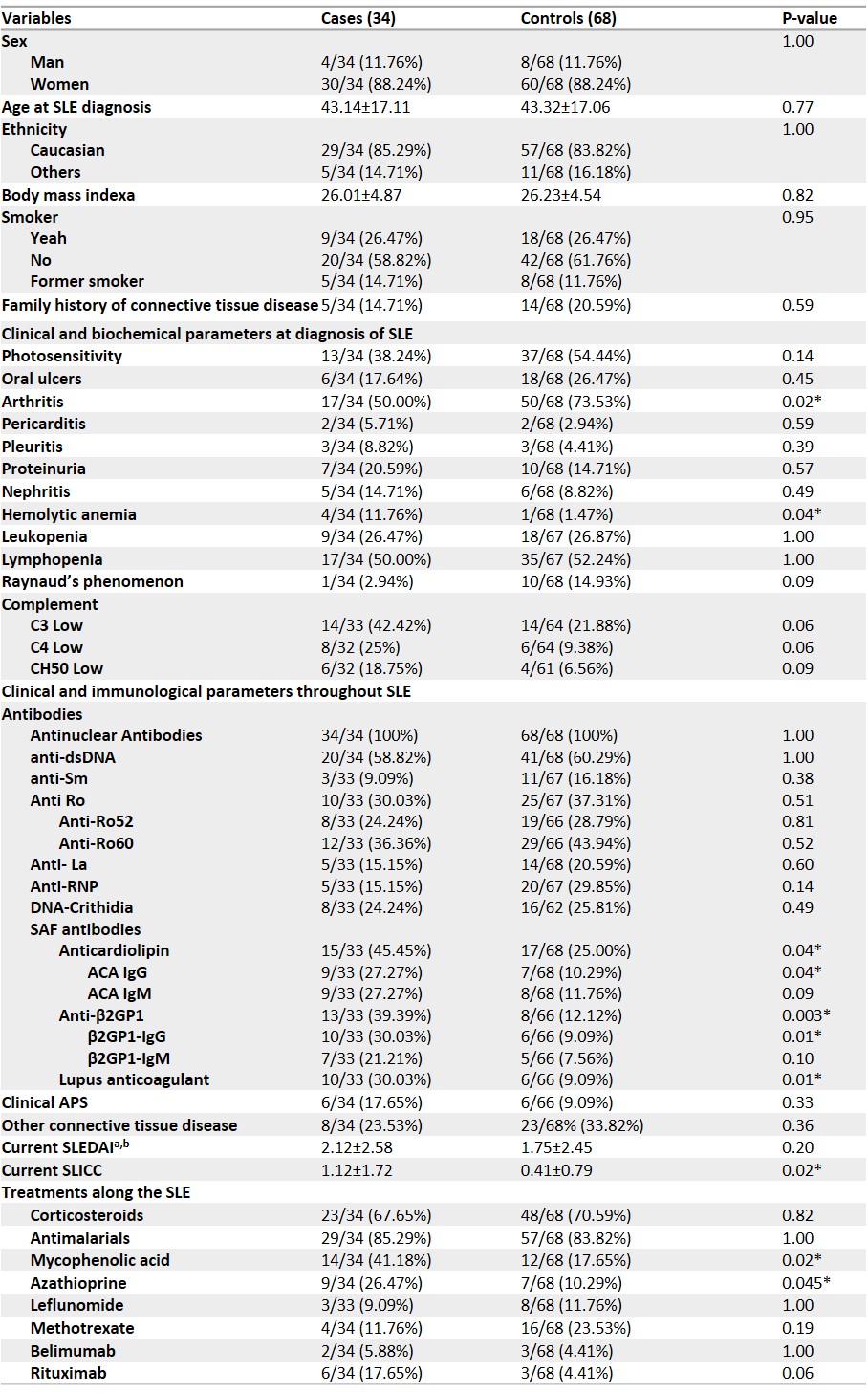
Table 1: Characteristics of cases and controls. * Indicates statistically significant differences between cases and controls (95% confidence level). a Indicates mean ± standard deviation. b SLEDAI-1 point. ITP: immune thrombocytopenia. APS: antiphospholipid syndrome. Anti-β2GP1: anti-β2-Glycoprotein 1 antibodies. ACA: anticardiolipin antibodies. SLEDAI: systemic lupus erythematosus disease activity index. SLICC: systemic lupus international collaborating clinics damage index.
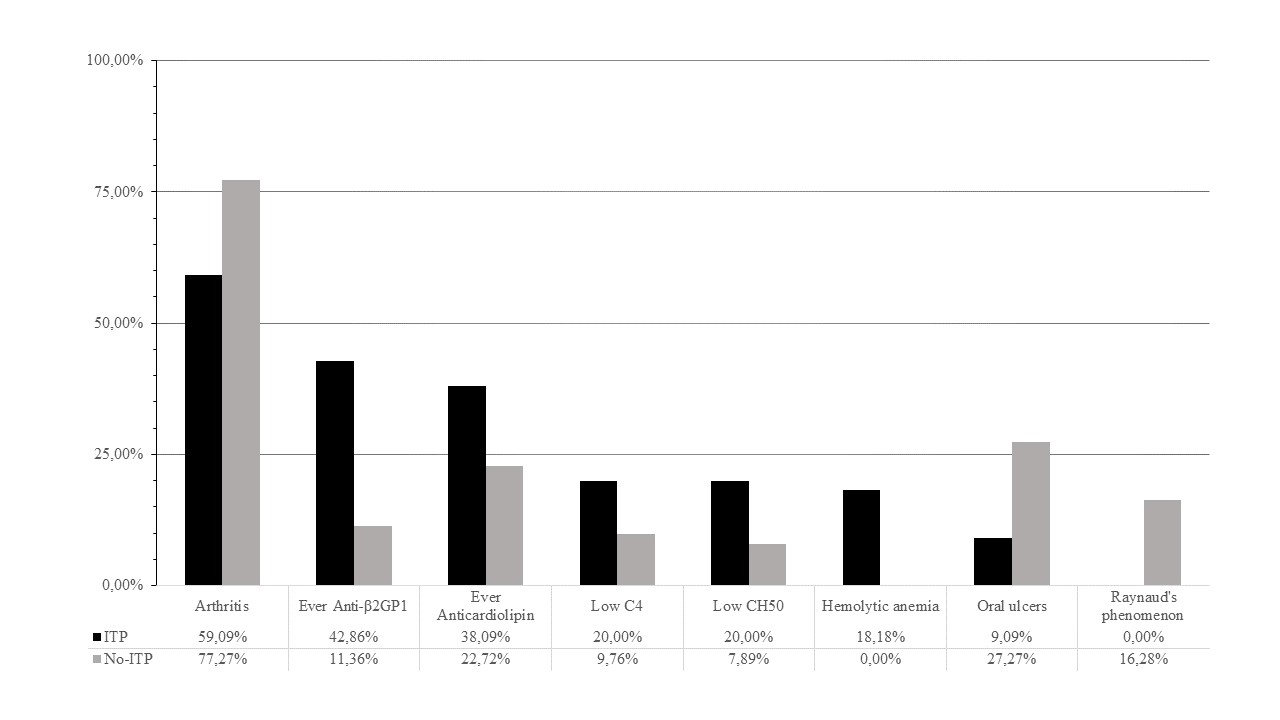
Figure 1: Variables used in the predictive model and their different prevalences in cases in controls. Ever anti-β2GP1: positivity for anti-β2-Glycoprotein 1 antibodies at any point during SLE progression. Ever anticardiolipin: positivity for anticardiolipin antibodies at any point during SLE progression.
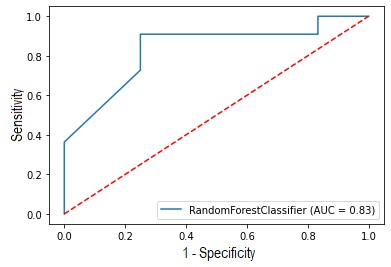
Figure 2: Area under the curve. Relationship between sensitivity and 1-specificity.
I. Carrión-Barberà: None; J. Cornudella Lema: None; S. Vázquez Montes de Oca: None; F. García Pallarols: None; J. Monfort: None; B. Sánchez-González: None; T. SALMAN MONTE: None.



