Poster Session A
Reproductive health
Session: (0460–0479) Reproductive Issues in Rheumatic Disorders Poster I
0479: Exploring Reproductive Experiences with Women Enrolled in the Vasculitis Pregnancy Registry
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- CS
Catherine Sims, MD
Duke University
Durham, NC, United StatesDisclosure(s): UCB: Grant/Research Support (Ongoing)
Abstract Poster Presenter(s)
Catherine Sims1, Christine Yeung2, Heather Tam3, Joyce Kullman4, Amanda Eudy5, Renee Borchin6, Cristina Burroughs6, Megan Clowse7 and Peter Merkel2, 1Duke University School of Medicine, Durham, NC, 2University of Pennsylvania, Philadelphia, PA, 3Vasculitis Patient Powered Research Network, Stanford, CA, 4Vasculitis Foundation, Kansas City, MO, 5Duke University, Raleigh, NC, 6University of South Florida, Tampa, FL, 7Duke University, Chapel Hill, NC
Background/Purpose: There are limited data on the reproductive health and experiences of women with vasculitis. This study engaged women with vasculitis to understand their perspectives about pregnancy and breastfeeding.
Methods: The Vasculitis Pregnancy Registry (VPREG) is an international, online, prospective, patient-reported registry within the Vasculitis Patient-Powered Research Network (VPPRN). The VPREG team partnered with the Vasculitis Foundation and patient research partners to develop two qualitative interview guides to prompt discussions of reproductive experiences with i) women who had live births; and ii) women who had non-live births. The guides included closed-ended scale items and open-ended prompts to elicit participant experiences. The interviews, performed by a rheumatologist, explored topics including pregnancy, medication choices to treat vasculitis, disease activity levels, patient-physician relationships, experiences with delivery, and breastfeeding. Participant responses were evaluated using thematic analysis.
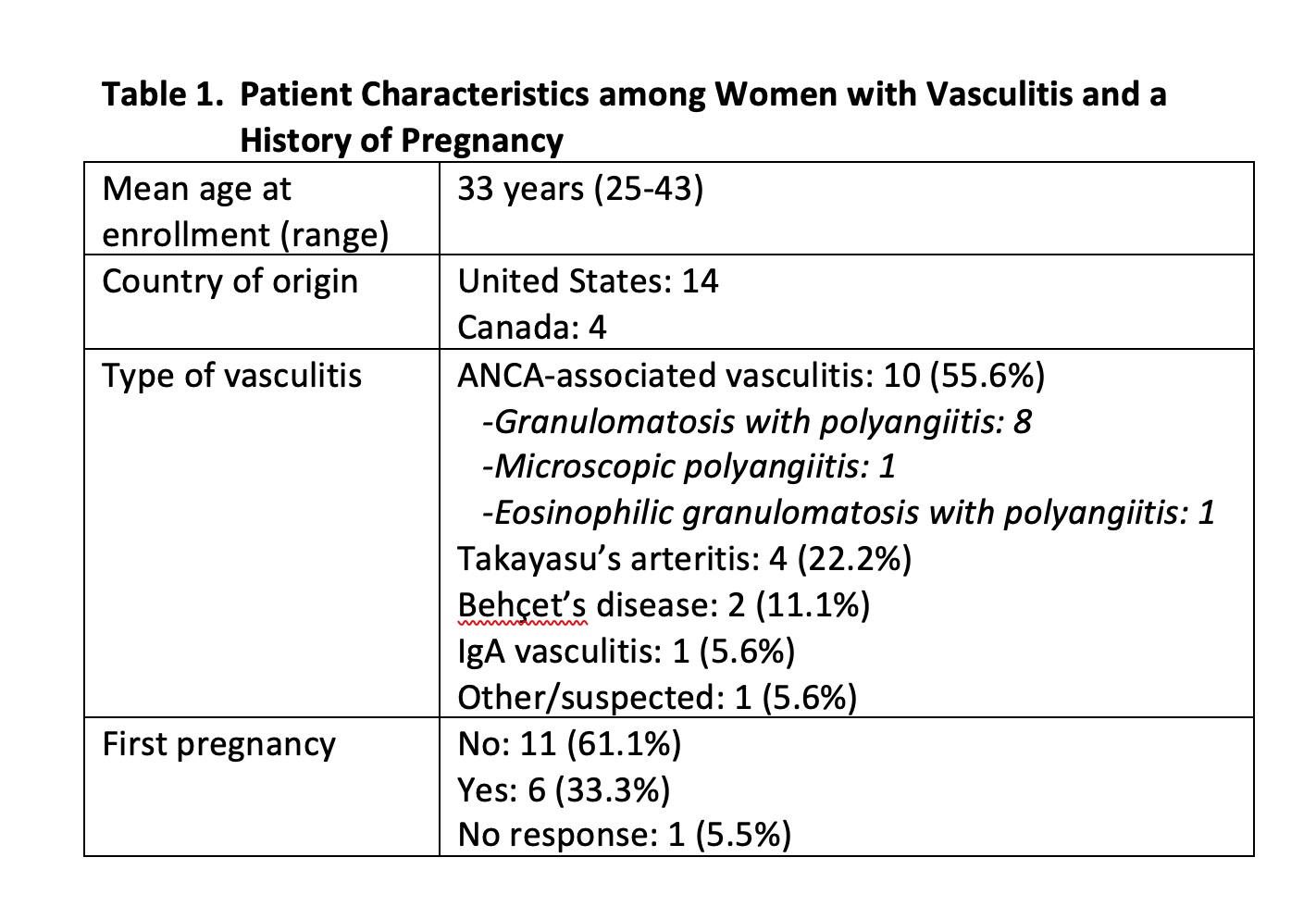
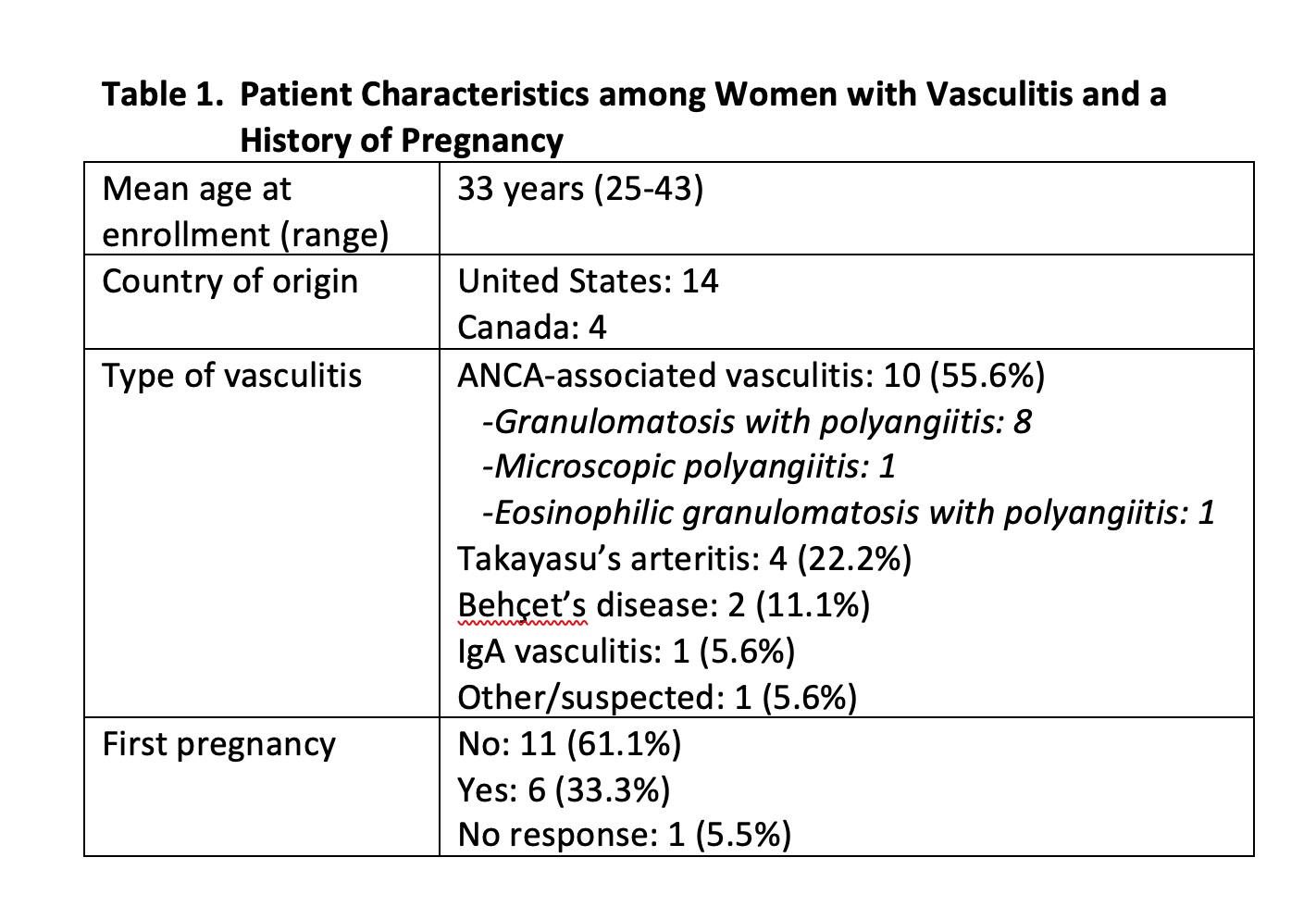
Results: The 18 participants were located in North America, ranged in age from 25-43 years, and most had more than one pregnancy (n=11) (Table 1). Anti-neutrophil cytoplasmic antibody-associated vasculitis was the most common diagnosis (n=10) followed by Takayasu's arteritis (n=4), Behçet's disease (n=2), IgA vasculitis (n=1), and relapsing polychondritis (n=1). Almost all pregnancies ended in a live birth (n=17).
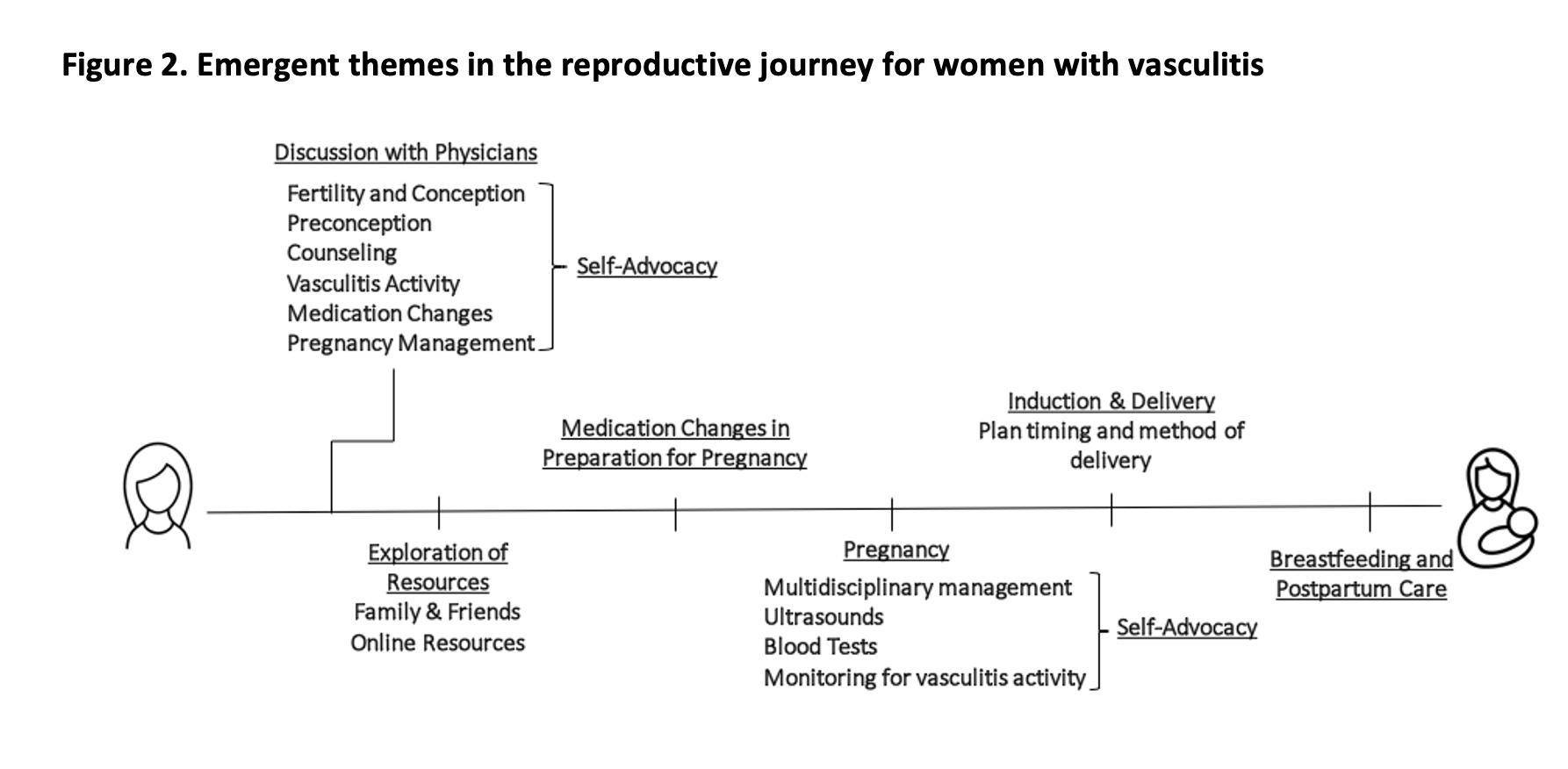
Four major themes emerged from interviews: 1) Women sought information about pregnancy from a range of sources, including their physicians, social media, and online forums (Figure 1); 2) Women cited discussions with family and physicians as important when deciding about treatment of vasculitis during pregnancy; 3) Women with vasculitis developed skills of self-advocacy during pregnancy to optimize communication between medical providers; and 4) Women with vasculitis had positive reproductive experiences with the majority reporting no flares of vasculitis, feeling "very well", and having "no pain" related to their vasculitis (Figure 2). Women who required changes to their medications to pursue their reproductive goals, identified physicians and family members as important participants in these conversations. Women described proactively gathering information about pregnancy and vasculitis from multiple sources, but ultimately decided their physician's perspective was the most influential. All women that used social media and online resources reported it did not impact or determine their reproductive decisions.
Conclusion: Women with vasculitis value the recommendations of their rheumatologists during reproductive healthcare discussions. Self-advocacy was frequently described during pregnancy because women felt they needed to act as liaisons among multiple specialists to ensure proper medical treatment. This study found that patients prioritize their relationships and conversations with physicians when planning for pregnancy.
.jpg)
C. Sims: UCB, 5; C. Yeung: None; H. Tam: None; J. Kullman: None; A. Eudy: Amgen, 2, Exagen, 5, GlaxoSmithKlein(GSK), 5, Immunovant, 5, Pfizer, 5; R. Borchin: None; C. Burroughs: None; M. Clowse: Exagen, 5, GlaxoSmithKlein(GSK), 2, 5, Immunovant, 5, UCB, 2, 5; P. Merkel: AbbVie/Abbott, 5, Amgen, 2, 5, ArGenx, 2, AstraZeneca, 2, 5, Boehringer-Ingelheim, 2, 5, Bristol-Myers Squibb(BMS), 2, 5, Cabaletta, 2, CSL Behring, 2, Eicos, 5, Electra, 5, Genentech, 5, GlaxoSmithKlein(GSK), 2, 5, HiBio, 2, InflaRx, 2, 5, Janssen, 2, Jubilant, 2, Kyverna, 2, 11, MiroBio, 2, Neutrolis, 5, Novartis, 2, NS Pharma, 2, Q32, 2, Regeneron, 2, Sanofi, 2, Sparrow, 2, Takeda, 2, 5, UpToDate, 9, Visterra, 2.
Background/Purpose: There are limited data on the reproductive health and experiences of women with vasculitis. This study engaged women with vasculitis to understand their perspectives about pregnancy and breastfeeding.
Methods: The Vasculitis Pregnancy Registry (VPREG) is an international, online, prospective, patient-reported registry within the Vasculitis Patient-Powered Research Network (VPPRN). The VPREG team partnered with the Vasculitis Foundation and patient research partners to develop two qualitative interview guides to prompt discussions of reproductive experiences with i) women who had live births; and ii) women who had non-live births. The guides included closed-ended scale items and open-ended prompts to elicit participant experiences. The interviews, performed by a rheumatologist, explored topics including pregnancy, medication choices to treat vasculitis, disease activity levels, patient-physician relationships, experiences with delivery, and breastfeeding. Participant responses were evaluated using thematic analysis.
Results: The 18 participants were located in North America, ranged in age from 25-43 years, and most had more than one pregnancy (n=11) (Table 1). Anti-neutrophil cytoplasmic antibody-associated vasculitis was the most common diagnosis (n=10) followed by Takayasu's arteritis (n=4), Behçet's disease (n=2), IgA vasculitis (n=1), and relapsing polychondritis (n=1). Almost all pregnancies ended in a live birth (n=17).
Four major themes emerged from interviews: 1) Women sought information about pregnancy from a range of sources, including their physicians, social media, and online forums (Figure 1); 2) Women cited discussions with family and physicians as important when deciding about treatment of vasculitis during pregnancy; 3) Women with vasculitis developed skills of self-advocacy during pregnancy to optimize communication between medical providers; and 4) Women with vasculitis had positive reproductive experiences with the majority reporting no flares of vasculitis, feeling "very well", and having "no pain" related to their vasculitis (Figure 2). Women who required changes to their medications to pursue their reproductive goals, identified physicians and family members as important participants in these conversations. Women described proactively gathering information about pregnancy and vasculitis from multiple sources, but ultimately decided their physician's perspective was the most influential. All women that used social media and online resources reported it did not impact or determine their reproductive decisions.
Conclusion: Women with vasculitis value the recommendations of their rheumatologists during reproductive healthcare discussions. Self-advocacy was frequently described during pregnancy because women felt they needed to act as liaisons among multiple specialists to ensure proper medical treatment. This study found that patients prioritize their relationships and conversations with physicians when planning for pregnancy.
.jpg)
Figure 1 displays the variety of resources patients with vasculitis accessed to gather information about their reproductive health
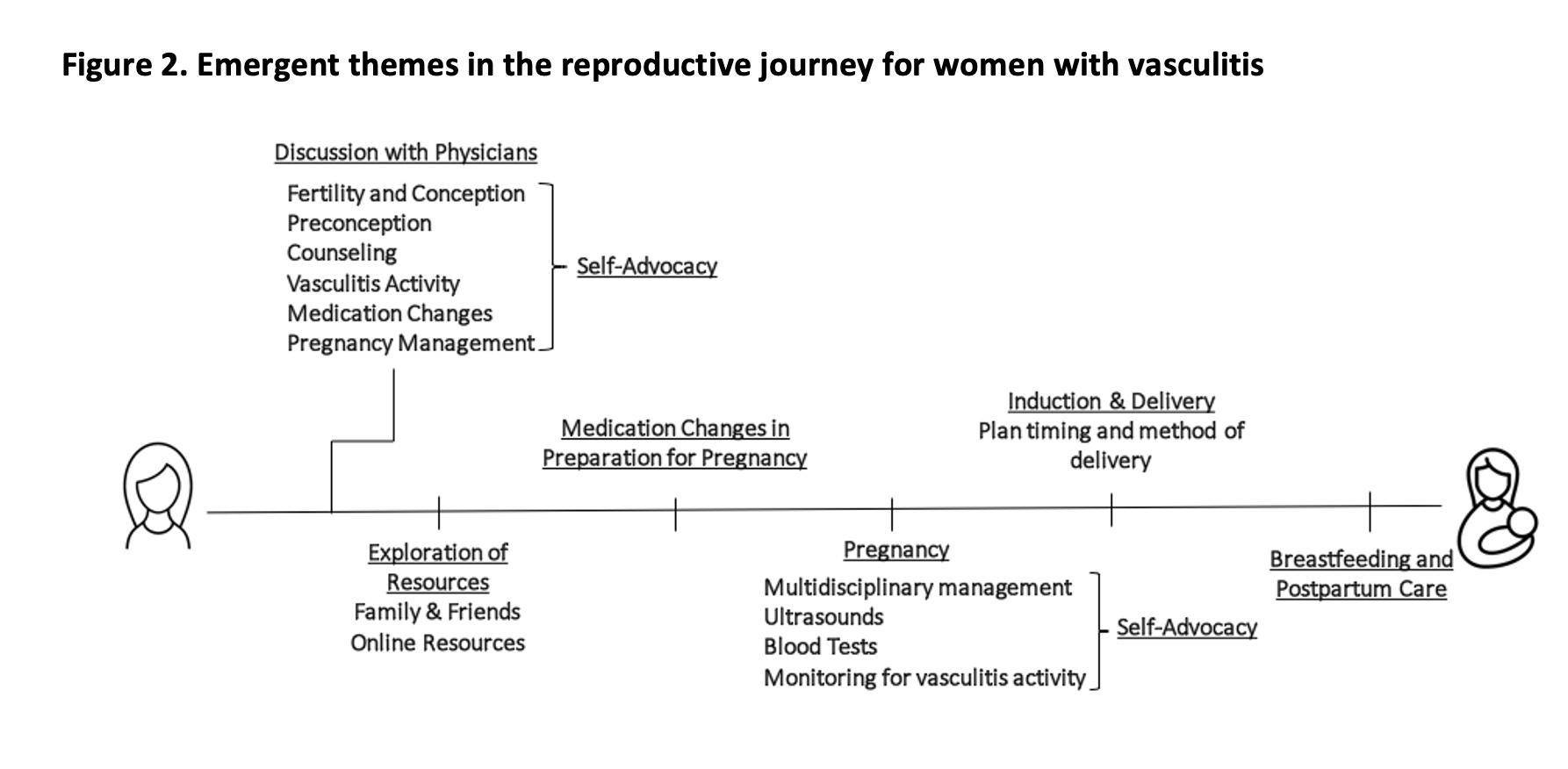
Figure 2 summarizes the emergent themes along the reproductive timeline of patients with vasculitis
C. Sims: UCB, 5; C. Yeung: None; H. Tam: None; J. Kullman: None; A. Eudy: Amgen, 2, Exagen, 5, GlaxoSmithKlein(GSK), 5, Immunovant, 5, Pfizer, 5; R. Borchin: None; C. Burroughs: None; M. Clowse: Exagen, 5, GlaxoSmithKlein(GSK), 2, 5, Immunovant, 5, UCB, 2, 5; P. Merkel: AbbVie/Abbott, 5, Amgen, 2, 5, ArGenx, 2, AstraZeneca, 2, 5, Boehringer-Ingelheim, 2, 5, Bristol-Myers Squibb(BMS), 2, 5, Cabaletta, 2, CSL Behring, 2, Eicos, 5, Electra, 5, Genentech, 5, GlaxoSmithKlein(GSK), 2, 5, HiBio, 2, InflaRx, 2, 5, Janssen, 2, Jubilant, 2, Kyverna, 2, 11, MiroBio, 2, Neutrolis, 5, Novartis, 2, NS Pharma, 2, Q32, 2, Regeneron, 2, Sanofi, 2, Sparrow, 2, Takeda, 2, 5, UpToDate, 9, Visterra, 2.



