Plenary Session
Session: Plenary I (0722–0726)
0726: Expert Consensus Recommendations for Musculoskeletal Ultrasound Education in Canadian Rheumatology Residency Training Programs
Sunday, November 12, 2023
12:15 PM - 12:25 PM PT
Location: Exhibit Hall A-B
- MP
Maria Powell, MD
University of Calgary
Calgary, AB, CanadaDisclosure(s): No financial relationships with ineligible companies to disclose
Plenary Presenter(s)
Maria Powell1, Steven Thomson1, Sibel Aydin2, Mohammad Bardi3, Susan Barr1, Lihi Eder4, Gurjit S Kaeley5, Sahil Koppikar6, Shirley Lake7, Christopher Lyddell8, Chris Penney1, Michael Stein9, Pooneh Akhavan10, Minna Kohler11, Maggie Larche12, Samar Aboulenain13, Dana Jerome6, Adam Kovacs-Litman13, Ashley Yip14, Janeve Desy1, Kevin McLaughlin1 and Irene W Y Ma1, 1University of Calgary, Calgary, AB, Canada, 2Department of Medicine, Ottawa Hospital Riverside Campus, Ottawa, ON, Canada, 3Dr. M Bardi Inc, Vancouver, BC, Canada, 4Women’s College Research Institute, Division of Rheumatology, University of Toronto, Toronto, ON, Canada, 5University of Florida College of Medicine – Jacksonville, Ponte Vedra Beach, FL, 6Women's College Hospital & University of Toronto, Toronto, ON, Canada, 7Sunny Brook Hospital & University of Toronto, North York, ON, Canada, 8Self, Edmonton, AB, Canada, 9McGill University, Montréal, QC, Canada, 10self-employed, Toronto, ON, Canada, 11Massachusetts General Hospital, Harvard Medical School, Boston, MA, 12McMaster University, Hamilton, ON, Canada, 13University of Toronto, Toronto, ON, Canada, 14University of Alberta, Edmonton, AB, Canada
Background/Purpose: The Royal College of Physicians and Surgeons of Canada has recently incorporated musculoskeletal ultrasound (MSUS) education into Canadian rheumatology residency programs as an optional training experience. Many Canadian rheumatology programs offer MSUS training for residents, but there is currently no national ultrasound curriculum in Canada outside of externally available courses. The objective of this study was to establish expert consensus on the MSUS competencies that can be incorporated into Canadian rheumatology residency training programs.
Methods: We used a 3-stage consensus design to identify MSUS competencies for Canadian rheumatology residents. We defined consensus a priori as agreement of 70% or higher. We identified all study participants using non-probability sampling and snowball technique. In stage 1, we invited 13 MSUS experts to participate in an online meeting using a modified nominal group technique (NGT) to identify a prioritized list of MSUS competencies. In stage 2, we invited 18 individuals including MSUS experts, rheumatology residents with MSUS experience, and rheumatology program directors with exposure to MSUS in their residency program to participate in a MSUS working group. We invited members of the MSUS working group to complete 3 rounds of online surveys using a modified Delphi technique to establish consensus on the items that should be included for each of the prioritized MSUS competencies identified during the modified NGT. Items not reaching consensus were re-addressed in a maximum of two subsequent rounds. In stage 3, we invited MSUS experts to attend a structured online focus group to review the final list of competencies.
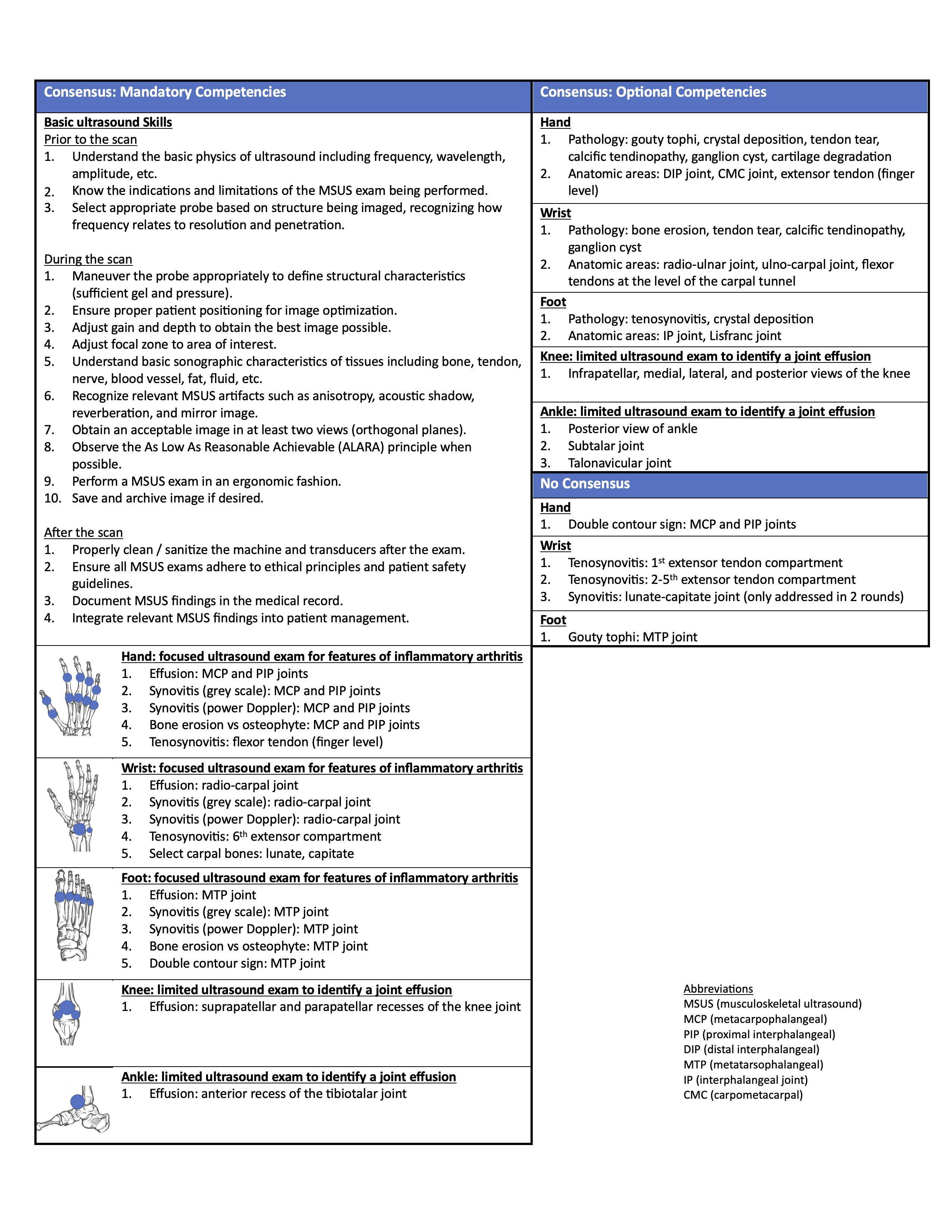
Results: Ten of the 13 invited MSUS experts attended the online meeting using a modified NGT, in which experts reached consensus on a prioritized list of 45 competencies (Figure 1). In stage 2, members of the MSUS working group included individuals from 7/12 (58%) Canadian rheumatology programs (English stream) and two MSUS experts from the United States. There was a 100% response rate for all 3 rounds of surveys in the modified Delphi technique. The first round of surveys addressed 86 items derived from the prioritized competencies identified during the modified NGT. The second round of surveys addressed 51 items, and the third round addressed 10 items. After 3 rounds of surveys, the MSUS working group reached consensus on all but 5 items, recommending 42 items be mandatory and 39 be optional. Members of the MSUS working group recommended that it is mandatory for all Canadian rheumatology residents to learn basic ultrasound skills; how to perform a focused MSUS exam of the hands, wrists, and feet for features of inflammatory arthritis including effusion, synovitis (grey scale and power Doppler), bone erosion versus osteophyte, and tenosynovitis; and a limited MSUS exam of the knee and ankle to identify a joint effusion (Table 1).
Conclusion: This study reports the expert consensus recommendations for MSUS in Canadian rheumatology residency training programs. These recommendations can be used to help guide programs as they develop MSUS curricula.

M. Powell: None; S. Thomson: None; S. Aydin: AbbVie, 5, 6, Celgene, 5, 6, Eli Lilly, 5, 6, Janssen, 5, 6, Novartis, 5, 6, Pfizer, 5, 6, UCB, 5, 6; M. Bardi: None; S. Barr: None; L. Eder: AbbVie, 2, 5, Eli Lilly, 2, 5, Fresenius Kabi, 5, Janssen, 2, 5, Novartis, 2, 5, Pfizer Inc, 2, 5, Sandoz, 5, UCB, 2, 5; G. S Kaeley: Abbvie, 5, Gilead, 5, Janssen, 5; S. Koppikar: None; S. Lake: None; C. Lyddell: None; C. Penney: None; M. Stein: None; P. Akhavan: None; M. Kohler: Mymee, 2, Springer Publications, 9; M. Larche: None; S. Aboulenain: None; D. Jerome: None; A. Kovacs-Litman: None; A. Yip: None; J. Desy: None; K. McLaughlin: None; I. Ma: None.
Background/Purpose: The Royal College of Physicians and Surgeons of Canada has recently incorporated musculoskeletal ultrasound (MSUS) education into Canadian rheumatology residency programs as an optional training experience. Many Canadian rheumatology programs offer MSUS training for residents, but there is currently no national ultrasound curriculum in Canada outside of externally available courses. The objective of this study was to establish expert consensus on the MSUS competencies that can be incorporated into Canadian rheumatology residency training programs.
Methods: We used a 3-stage consensus design to identify MSUS competencies for Canadian rheumatology residents. We defined consensus a priori as agreement of 70% or higher. We identified all study participants using non-probability sampling and snowball technique. In stage 1, we invited 13 MSUS experts to participate in an online meeting using a modified nominal group technique (NGT) to identify a prioritized list of MSUS competencies. In stage 2, we invited 18 individuals including MSUS experts, rheumatology residents with MSUS experience, and rheumatology program directors with exposure to MSUS in their residency program to participate in a MSUS working group. We invited members of the MSUS working group to complete 3 rounds of online surveys using a modified Delphi technique to establish consensus on the items that should be included for each of the prioritized MSUS competencies identified during the modified NGT. Items not reaching consensus were re-addressed in a maximum of two subsequent rounds. In stage 3, we invited MSUS experts to attend a structured online focus group to review the final list of competencies.
Results: Ten of the 13 invited MSUS experts attended the online meeting using a modified NGT, in which experts reached consensus on a prioritized list of 45 competencies (Figure 1). In stage 2, members of the MSUS working group included individuals from 7/12 (58%) Canadian rheumatology programs (English stream) and two MSUS experts from the United States. There was a 100% response rate for all 3 rounds of surveys in the modified Delphi technique. The first round of surveys addressed 86 items derived from the prioritized competencies identified during the modified NGT. The second round of surveys addressed 51 items, and the third round addressed 10 items. After 3 rounds of surveys, the MSUS working group reached consensus on all but 5 items, recommending 42 items be mandatory and 39 be optional. Members of the MSUS working group recommended that it is mandatory for all Canadian rheumatology residents to learn basic ultrasound skills; how to perform a focused MSUS exam of the hands, wrists, and feet for features of inflammatory arthritis including effusion, synovitis (grey scale and power Doppler), bone erosion versus osteophyte, and tenosynovitis; and a limited MSUS exam of the knee and ankle to identify a joint effusion (Table 1).
Conclusion: This study reports the expert consensus recommendations for MSUS in Canadian rheumatology residency training programs. These recommendations can be used to help guide programs as they develop MSUS curricula.

Figure 1: Summary of the modified nominal group technique (NGT) process used to identify prioritized musculoskeletal ultrasound (MSUS) competencies for Canadian rheumatology residents.
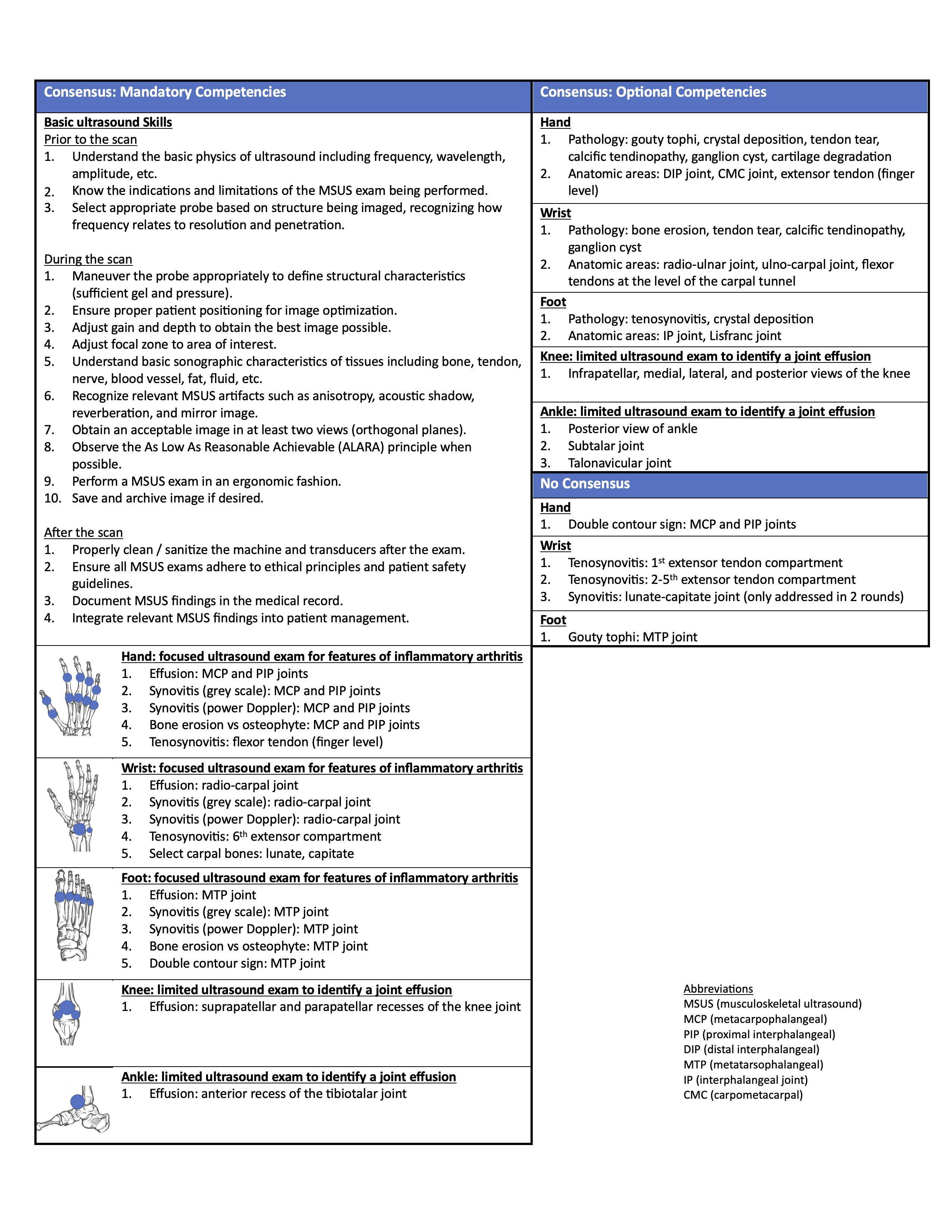
Table 1: Summary of final recommended musculoskeletal ultrasound (MSUS) competencies for Canadian rheumatology residents after 3 rounds of surveys using a modified Delphi technique.
M. Powell: None; S. Thomson: None; S. Aydin: AbbVie, 5, 6, Celgene, 5, 6, Eli Lilly, 5, 6, Janssen, 5, 6, Novartis, 5, 6, Pfizer, 5, 6, UCB, 5, 6; M. Bardi: None; S. Barr: None; L. Eder: AbbVie, 2, 5, Eli Lilly, 2, 5, Fresenius Kabi, 5, Janssen, 2, 5, Novartis, 2, 5, Pfizer Inc, 2, 5, Sandoz, 5, UCB, 2, 5; G. S Kaeley: Abbvie, 5, Gilead, 5, Janssen, 5; S. Koppikar: None; S. Lake: None; C. Lyddell: None; C. Penney: None; M. Stein: None; P. Akhavan: None; M. Kohler: Mymee, 2, Springer Publications, 9; M. Larche: None; S. Aboulenain: None; D. Jerome: None; A. Kovacs-Litman: None; A. Yip: None; J. Desy: None; K. McLaughlin: None; I. Ma: None.



