Plenary Session
Reproductive health
Session: Plenary I (0722–0726)
0722: Acute Cardiovascular Events in Autoimmune Rheumatic Disease Pregnancies
Sunday, November 12, 2023
11:15 AM - 11:25 AM PT
Location: Exhibit Hall A-B
- RD
Rashmi Dhital, MD
UC San Diego
San Diego, CA, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Plenary Presenter(s)
Rashmi Dhital1, Rebecca Baer2, Monica Guma2, Kenneth Kalunian2, Accelerating Medicines Partnership Program RA SLE Network3 and Christina Chambers2, 1UC San Diego, San Diego, CA, 2University of California San Diego, La Jolla, CA, 3Cedars-Sinai Medical Center, Los Angeles, CA
Background/Purpose: Cardiovascular diseases (CVDs) complicate 1-4% of pregnancies. Autoimmune rheumatic diseases (ARDs) are associated with a 1.5 to 3-fold higher CVD risk. Similarly, antiphospholipid syndrome (APS) is associated with increased risks of thromboembolism, pregnancy loss, and CVDs. However, research on the impact of ARDs and APS on maternal cardiovascular health is limited. In this study, we aim to compare the rates of acute CVEs in pregnant women with ARDs and primary APS as compared to a general population of pregnant women with neither condition, using a large population-based birth cohort in California.
Methods: We retrospectively analyzed pregnant individuals who delivered singleton liveborn infants in California between 2005-2020. Birth certificates were linked by the California Study of Outcomes in Mothers and Infants (SOMI) to maternal hospital discharge, emergency department and ambulatory surgery records. We identified ARDs, APS, and acute CVEs during pregnancy and up to 6 weeks postpartum using ICD codes. We used logistic regression to calculate adjusted relative risks (RRs) and 95% confidence intervals (CI) of association between acute CVEs and ARDs and APS, for each specific category of ARDs, and for CVEs by timing in relation to delivery. We performed mediation analysis to investigate if pregnancy complications such as gestational diabetes mellitus (GDM) and pre-eclampsia mediated the association between ARDs and CVEs.
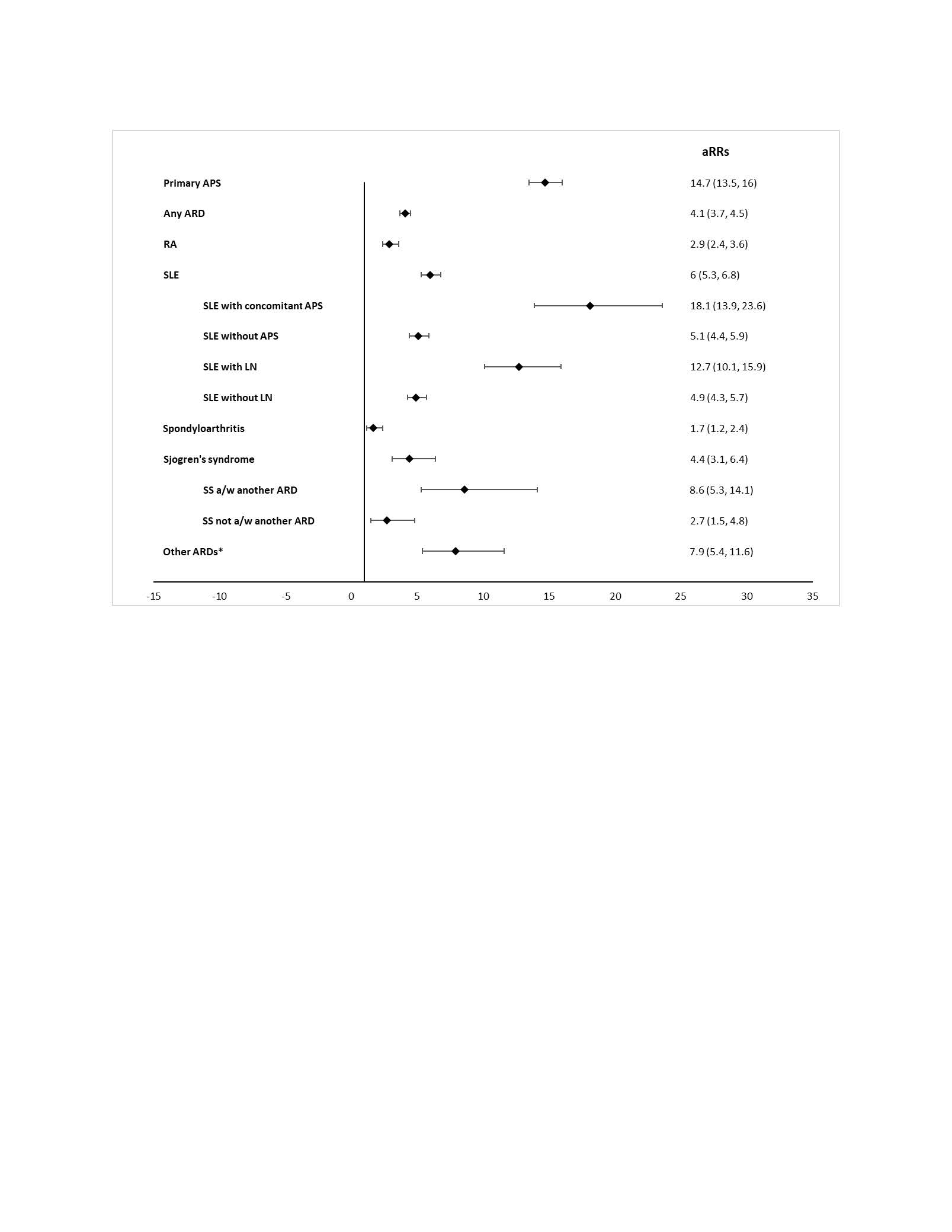
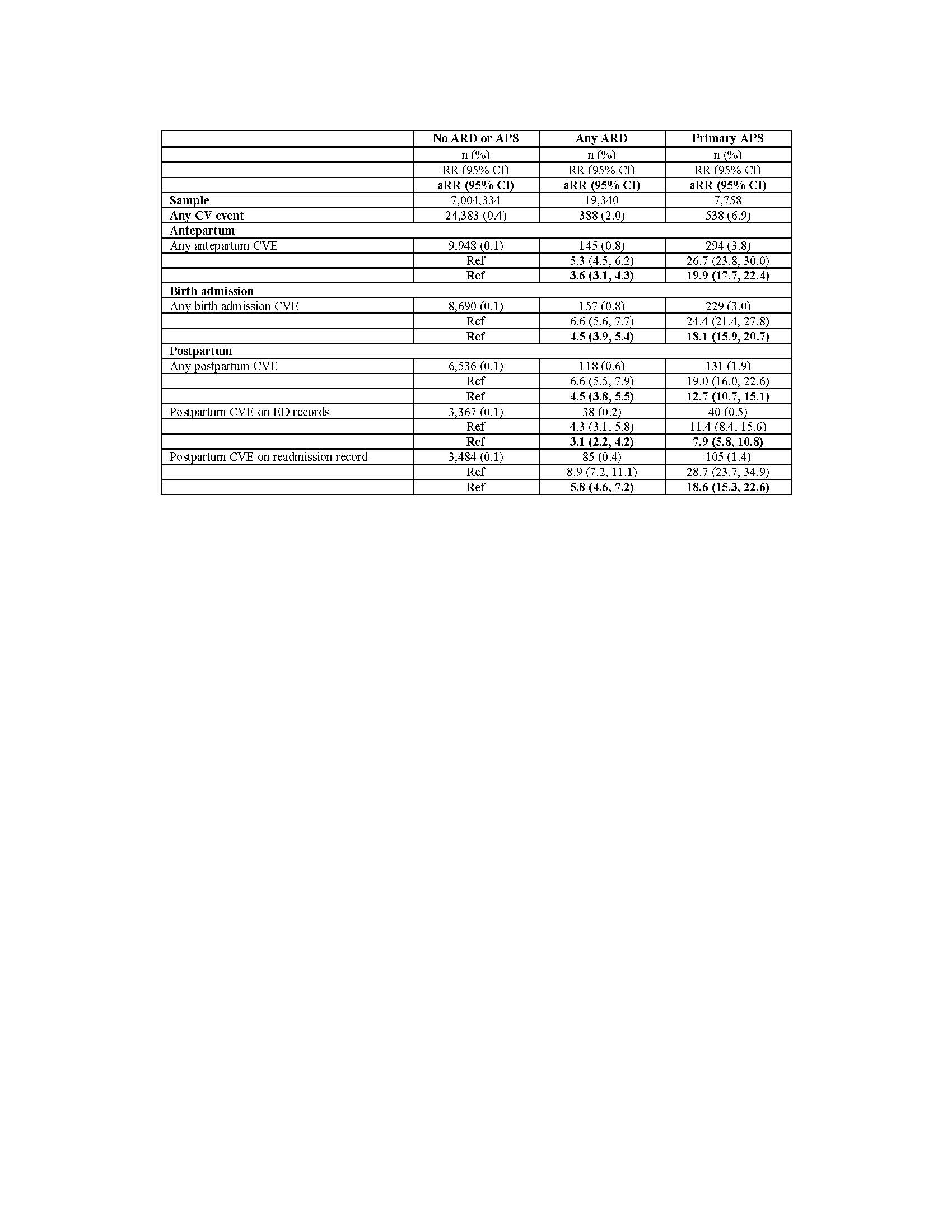
Results: CVEs occurred in 2.0% of 19,340 pregnant women with ARDs, 6.9% of 7,758 women with primary APS, and 0.4% of 7,004,334 women with neither. The risks of acute CVEs were significantly higher for pregnant women with ARDs (aRR 4.1, 95% CI 3.7, 4.5) and primary APS (aRR 14.7, 95% CI 13.5,16.0) than for the comparison group. Systemic lupus erythematosus (SLE) was associated with a 6-fold increased risk for CVE, which was further elevated with concomitant APS or nephritis (aRRs 18.1 and 12.7, respectively). (Figure 1). Only 12% of the excess association of acute CVEs with an ARD was mediated by preeclampsia and < 1% by GDM. About 25-30% of the CVEs occurred postpartum as documented in readmission records. This represented a 6-fold greater risk than in the comparison group (Table 2).
Conclusion: Pregnant women with ARDs and primary APS have significantly higher risks for acute CVEs compared to pregnant women without these conditions, with the highest risks among those with SLE with concomitant APS, followed by primary APS and SLE with nephritis. Furthermore, about 25-30% of CVEs occurred during the postpartum period, highlighting the importance of close monitoring of cardiovascular risks and events in women with ARDs or APS both during pregnancy and postpartum.
R. Dhital: None; R. Baer: None; M. Guma: None; K. Kalunian: AbbVie/Abbott, 2, Amgen, 5, AstraZeneca, 2, Aurinia, 2, Bristol-Myers Squibb(BMS), 2, Eli Lilly, 2, EquilliumBio, 2, Genentech, 2, Gilead, 2, Janssen, 2, KezarBio, 1, Merck/MSD, 2, Novartis, 2, Pfizer, 2, Remegene, 2, Roche, 2, UCB, 5; A. RA SLE Network: None; C. Chambers: Amgen, 5, AstraZeneca, 5, Bristol-Myers Squibb(BMS), 5, Genzyme Sanofi-Aventis, 5, Gerber Foundation, 5, Gilead, 5, GlaxoSmithKline, 5, Hoffman La-Roche-Genentech, 5, Janssen Pharmaceuticals, 5, Leo Pharma, 5, Novartis, 5, Pfizer, Inc., 5, Regeneron, 5, Sanofi, 5, Sun Pharma Global FZE, 5, Takeda Pharmaceutical Company Limited, 5, UCB Pharma, USA, 5.
Background/Purpose: Cardiovascular diseases (CVDs) complicate 1-4% of pregnancies. Autoimmune rheumatic diseases (ARDs) are associated with a 1.5 to 3-fold higher CVD risk. Similarly, antiphospholipid syndrome (APS) is associated with increased risks of thromboembolism, pregnancy loss, and CVDs. However, research on the impact of ARDs and APS on maternal cardiovascular health is limited. In this study, we aim to compare the rates of acute CVEs in pregnant women with ARDs and primary APS as compared to a general population of pregnant women with neither condition, using a large population-based birth cohort in California.
Methods: We retrospectively analyzed pregnant individuals who delivered singleton liveborn infants in California between 2005-2020. Birth certificates were linked by the California Study of Outcomes in Mothers and Infants (SOMI) to maternal hospital discharge, emergency department and ambulatory surgery records. We identified ARDs, APS, and acute CVEs during pregnancy and up to 6 weeks postpartum using ICD codes. We used logistic regression to calculate adjusted relative risks (RRs) and 95% confidence intervals (CI) of association between acute CVEs and ARDs and APS, for each specific category of ARDs, and for CVEs by timing in relation to delivery. We performed mediation analysis to investigate if pregnancy complications such as gestational diabetes mellitus (GDM) and pre-eclampsia mediated the association between ARDs and CVEs.
Results: CVEs occurred in 2.0% of 19,340 pregnant women with ARDs, 6.9% of 7,758 women with primary APS, and 0.4% of 7,004,334 women with neither. The risks of acute CVEs were significantly higher for pregnant women with ARDs (aRR 4.1, 95% CI 3.7, 4.5) and primary APS (aRR 14.7, 95% CI 13.5,16.0) than for the comparison group. Systemic lupus erythematosus (SLE) was associated with a 6-fold increased risk for CVE, which was further elevated with concomitant APS or nephritis (aRRs 18.1 and 12.7, respectively). (Figure 1). Only 12% of the excess association of acute CVEs with an ARD was mediated by preeclampsia and < 1% by GDM. About 25-30% of the CVEs occurred postpartum as documented in readmission records. This represented a 6-fold greater risk than in the comparison group (Table 2).
Conclusion: Pregnant women with ARDs and primary APS have significantly higher risks for acute CVEs compared to pregnant women without these conditions, with the highest risks among those with SLE with concomitant APS, followed by primary APS and SLE with nephritis. Furthermore, about 25-30% of CVEs occurred during the postpartum period, highlighting the importance of close monitoring of cardiovascular risks and events in women with ARDs or APS both during pregnancy and postpartum.
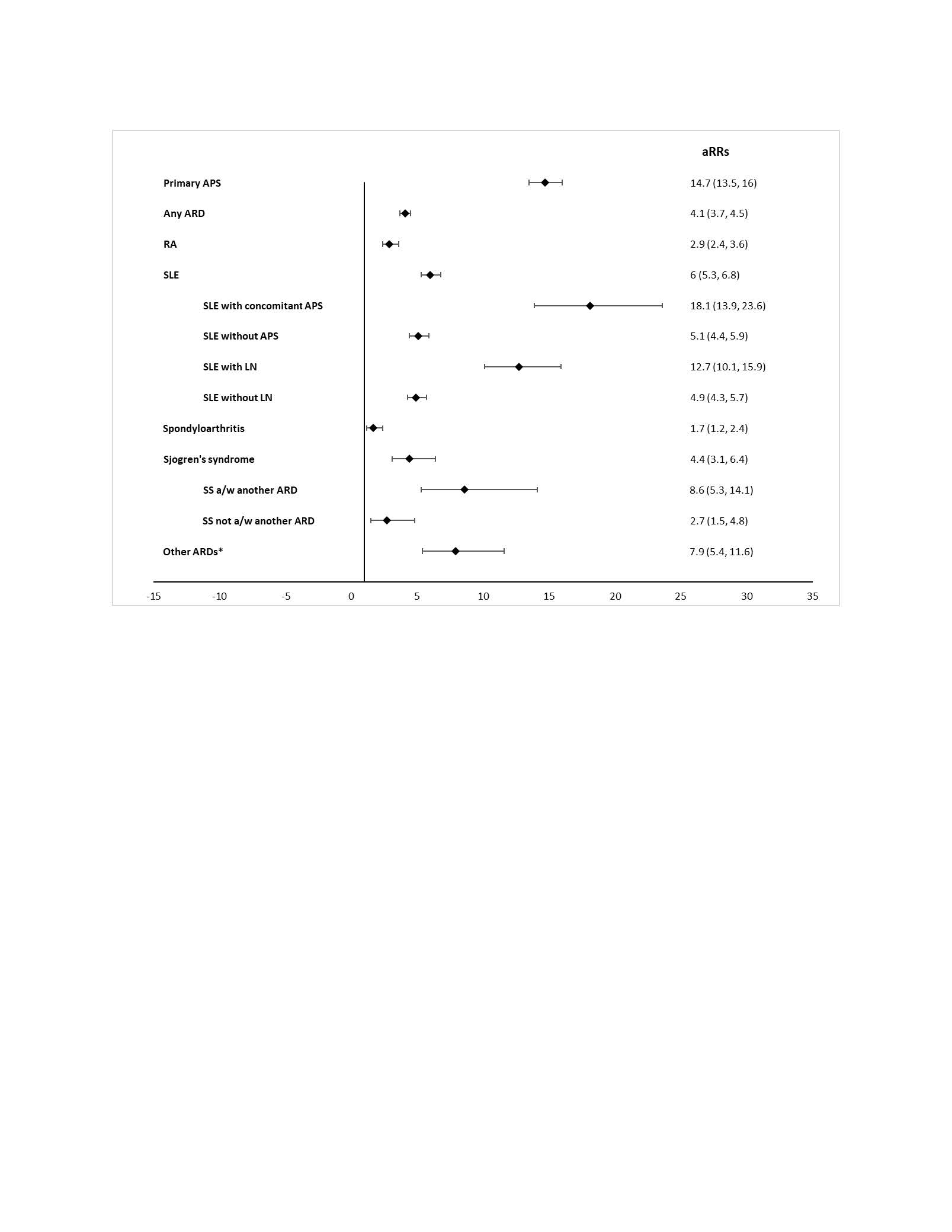
Figure 1. Comparison of risks of acute cardiovascular events during pregnancy or within 6 weeks post-partum for autoimmune rheumatic diseases (ARDs) and primary antiphospholipid syndrome (APS) as compared to the comparison group with neither condition, 2005 – 2020
#Adjusted relative risks (aRRs) adjusted for baseline covariates that occurred before pregnancy (maternal age at delivery, race/ethnicity, payer for delivery, maternal education, maternal pre-pregnancy body mass index, preexisting hypertension, preexisting diabetes, hyperlipidemia, smoking, alcohol use, drug use, and depression).
* APS: antiphospholipid syndrome, ARD: autoimmune rheumatic disease, RA: rheumatoid arthritis, SLE: systemic lupus erythematosus, LN: lupus nephritis, SS: Sjogren’s syndrome, * Other ARDs (Systemic sclerosis, myositis, vasculitis)
#Adjusted relative risks (aRRs) adjusted for baseline covariates that occurred before pregnancy (maternal age at delivery, race/ethnicity, payer for delivery, maternal education, maternal pre-pregnancy body mass index, preexisting hypertension, preexisting diabetes, hyperlipidemia, smoking, alcohol use, drug use, and depression).
* APS: antiphospholipid syndrome, ARD: autoimmune rheumatic disease, RA: rheumatoid arthritis, SLE: systemic lupus erythematosus, LN: lupus nephritis, SS: Sjogren’s syndrome, * Other ARDs (Systemic sclerosis, myositis, vasculitis)
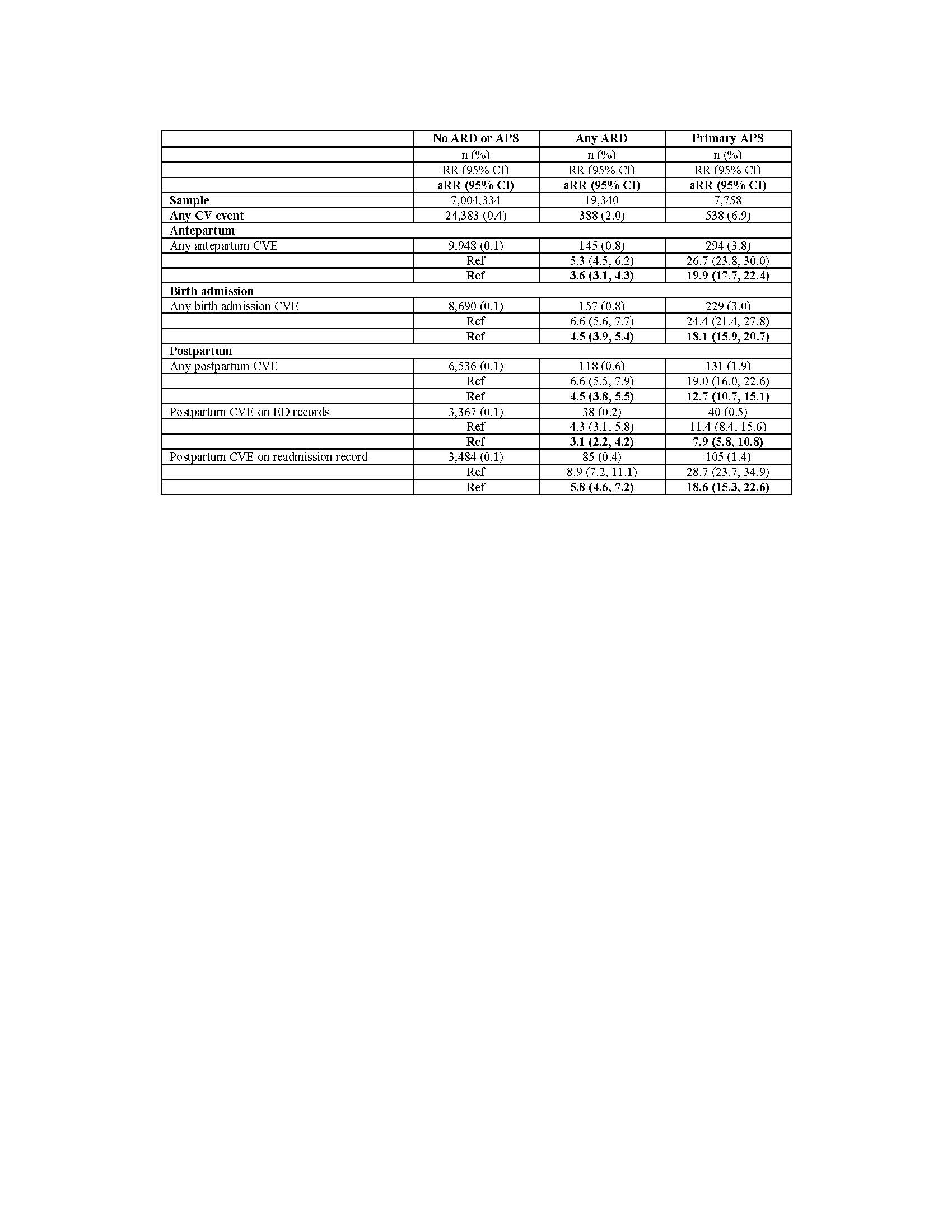
Table 2. Rates of acute cardiovascular events by timing in relation to delivery for autoimmune rheumatic diseases (ARDs) and primary antiphospholipid syndrome (APS) as compared to the comparison group with neither condition, 2005 – 2020
*ARD: autoimmune rheumatic disease, APS: antiphospholipid syndrome, CVE: cardiovascular event, ED: emergency department
*ARD: autoimmune rheumatic disease, APS: antiphospholipid syndrome, CVE: cardiovascular event, ED: emergency department
R. Dhital: None; R. Baer: None; M. Guma: None; K. Kalunian: AbbVie/Abbott, 2, Amgen, 5, AstraZeneca, 2, Aurinia, 2, Bristol-Myers Squibb(BMS), 2, Eli Lilly, 2, EquilliumBio, 2, Genentech, 2, Gilead, 2, Janssen, 2, KezarBio, 1, Merck/MSD, 2, Novartis, 2, Pfizer, 2, Remegene, 2, Roche, 2, UCB, 5; A. RA SLE Network: None; C. Chambers: Amgen, 5, AstraZeneca, 5, Bristol-Myers Squibb(BMS), 5, Genzyme Sanofi-Aventis, 5, Gerber Foundation, 5, Gilead, 5, GlaxoSmithKline, 5, Hoffman La-Roche-Genentech, 5, Janssen Pharmaceuticals, 5, Leo Pharma, 5, Novartis, 5, Pfizer, Inc., 5, Regeneron, 5, Sanofi, 5, Sun Pharma Global FZE, 5, Takeda Pharmaceutical Company Limited, 5, UCB Pharma, USA, 5.



