Poster Session A
Vasculitis
Session: (0691–0721) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
0698: Differentiating Large Vessel Vasculitis from Vasculitis Mimickers in a Real World Setting: Clinical Presentation, Laboratory Tests and Radiographic Findings
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- JH
James Haigney, MD
Beth Israel Deaconess Medical Center
Medford, MA, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
James haigney1, Laura Fandino1 and Vasileios Kyttaris2, 1Beth Israel Deaconess Medical Center, Boston, MA, 2BIDMC, Boston, MA
Background/Purpose: As the resolution of Computed Tomography Angiography (CTA) has improved, rheumatologists have faced an increased volume of consults to evaluate patients for the presence of radiographic abdominal vasculitis (RAV). Biopsy is often not possible due to the nature of the lesion. In our experience, a large portion of these patients are ultimately not found to have vasculitis after a thorough evaluation. In this study we sought to identify the most predictive symptoms, laboratory, and imaging findings of having RAV at the first point of contact with the rheumatology consult service.
Methods: Patients with billing codes for vasculitis or non-inflammatory arteriopathies (NIA) evaluated by the rheumatology service between January 1, 2016 and December 31, 2021 were considered for inclusion in this study. Of these, only patients with question of vasculitis by imaging of the renal arteries, abdominal aorta, or mesenteric arteries and their branches (celiac, inferior and superior mesenteric arteries) with >1 year of follow up were included in the final analysis. Biographic data, presenting symptoms, laboratory data, and imaging reports were extracted. Patients were classified by their final diagnosis at the 1-year time point as either having vasculitis or NIA as determined by the treating physician based on their clinical course and response to treatment. Statistical analysis was conducted using STATA software.
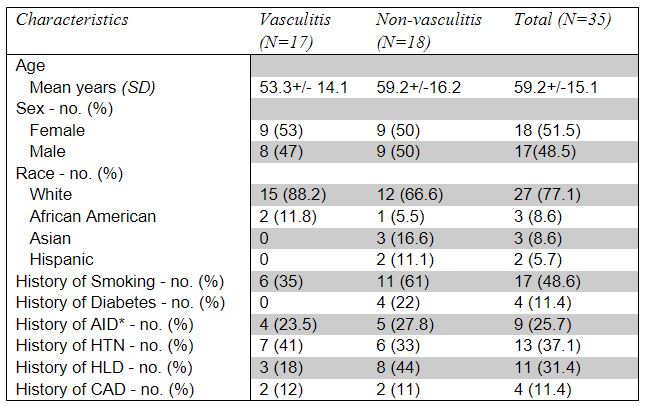
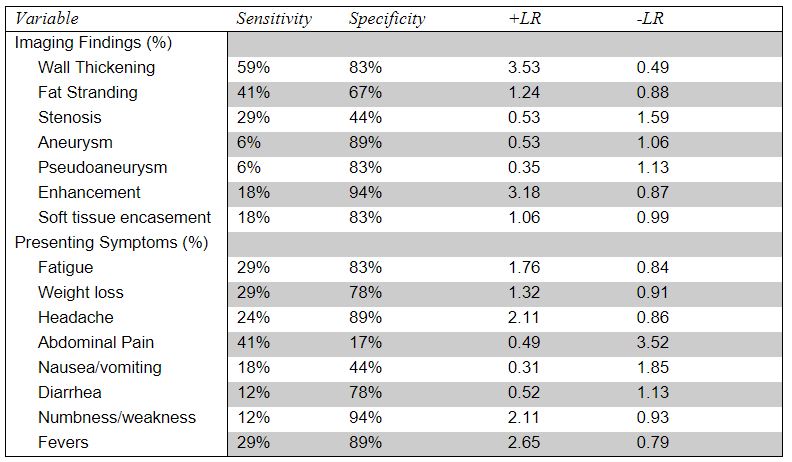
Results: Of 683 candidate patients, 63 were seen by rheumatology for the question of RAV. 27 were excluded for insufficient data, 1 was excluded for question of vasculitis surrounding a stent, and 35 were included in the final analysis. Of these, 17 were ultimately determined to have vasculitis, and 18 were determined to not have vasculitis. Baseline patient characteristics are available in table 1. Notably 2 patients ultimately found to not have vasculitis received treatment for vasculitis in the follow up period, and 1 patient ultimately found to have vasculitis was managed as non-vasculitis with observation before treatment was initiated. Analysis of the predictive value of imaging findings and presenting symptoms are reported in table 2. Notably, wall thickening of the relevant vessels was found to be the most helpful finding with a specificity of 83% and positive likelihood ratio (+LR) of 3.53. Interestingly fat stranding was found to be less helpful with a specificity of 67% and +LR of 1.2. Wall enhancement was rarely seen but was highly specific for vasculitis with a specificity of 94% and +LR of 3.18. None of the presenting symptoms were found to be especially predictive of vasculitis. Analysis of laboratory findings on presentation revealed initial white blood cell count (WBC) and platelet count (Plt) were significantly higher in patients with vasculitis (Table 3).
Conclusion: Our study identified wall thickening, wall enhancement, and elevations in WBC and Plt as being predictive of having abdominal vasculitis. While commonly reported, fat stranding was non-specific. Interestingly the tested presenting symptoms were not successful in delineating which patients were ultimately determined to have vasculitis. Confirmation of these findings with larger prospective studies is warranted.
.jpg)
J. haigney: None; L. Fandino: None; V. Kyttaris: AbbVie/Abbott, 5, AstraZeneca, 2, Aurinia, 1, EMD Serono, 5, Exagen, 2, 5, Fresenius Kabi, 1, Horizon Pharmaceuticals, 1, Novartis, 5, Scipher, 1, Takeda, 5, Vertex, 2.
Background/Purpose: As the resolution of Computed Tomography Angiography (CTA) has improved, rheumatologists have faced an increased volume of consults to evaluate patients for the presence of radiographic abdominal vasculitis (RAV). Biopsy is often not possible due to the nature of the lesion. In our experience, a large portion of these patients are ultimately not found to have vasculitis after a thorough evaluation. In this study we sought to identify the most predictive symptoms, laboratory, and imaging findings of having RAV at the first point of contact with the rheumatology consult service.
Methods: Patients with billing codes for vasculitis or non-inflammatory arteriopathies (NIA) evaluated by the rheumatology service between January 1, 2016 and December 31, 2021 were considered for inclusion in this study. Of these, only patients with question of vasculitis by imaging of the renal arteries, abdominal aorta, or mesenteric arteries and their branches (celiac, inferior and superior mesenteric arteries) with >1 year of follow up were included in the final analysis. Biographic data, presenting symptoms, laboratory data, and imaging reports were extracted. Patients were classified by their final diagnosis at the 1-year time point as either having vasculitis or NIA as determined by the treating physician based on their clinical course and response to treatment. Statistical analysis was conducted using STATA software.
Results: Of 683 candidate patients, 63 were seen by rheumatology for the question of RAV. 27 were excluded for insufficient data, 1 was excluded for question of vasculitis surrounding a stent, and 35 were included in the final analysis. Of these, 17 were ultimately determined to have vasculitis, and 18 were determined to not have vasculitis. Baseline patient characteristics are available in table 1. Notably 2 patients ultimately found to not have vasculitis received treatment for vasculitis in the follow up period, and 1 patient ultimately found to have vasculitis was managed as non-vasculitis with observation before treatment was initiated. Analysis of the predictive value of imaging findings and presenting symptoms are reported in table 2. Notably, wall thickening of the relevant vessels was found to be the most helpful finding with a specificity of 83% and positive likelihood ratio (+LR) of 3.53. Interestingly fat stranding was found to be less helpful with a specificity of 67% and +LR of 1.2. Wall enhancement was rarely seen but was highly specific for vasculitis with a specificity of 94% and +LR of 3.18. None of the presenting symptoms were found to be especially predictive of vasculitis. Analysis of laboratory findings on presentation revealed initial white blood cell count (WBC) and platelet count (Plt) were significantly higher in patients with vasculitis (Table 3).
Conclusion: Our study identified wall thickening, wall enhancement, and elevations in WBC and Plt as being predictive of having abdominal vasculitis. While commonly reported, fat stranding was non-specific. Interestingly the tested presenting symptoms were not successful in delineating which patients were ultimately determined to have vasculitis. Confirmation of these findings with larger prospective studies is warranted.
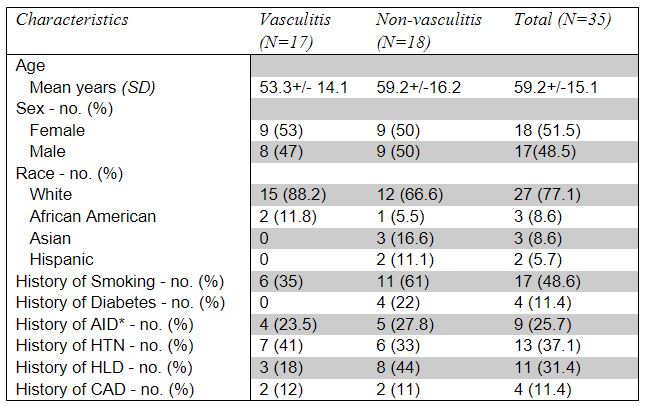
Table 1: Demographics and clinical characteristics of patients at baseline diagnosed with vasculitis vs non-vasculitis after consultation for question of RAV. AID denotes autoimmune disease, HTN smoking, HLD hyperlipidemia, and CAD coronary artery disease.
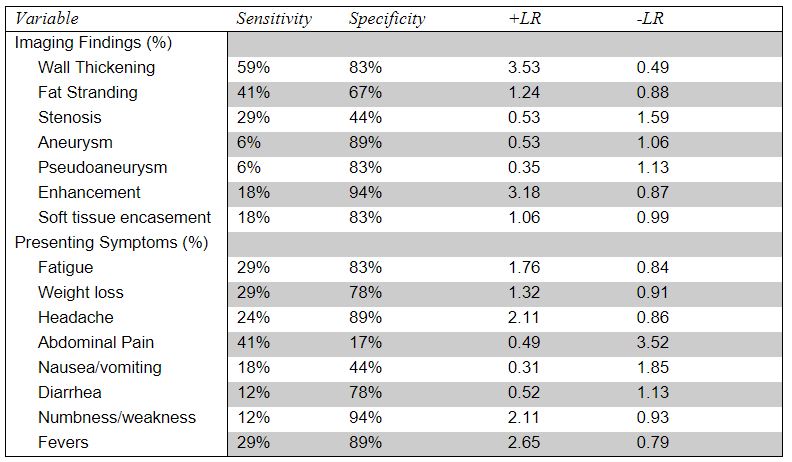
Table 2: Sensitivity, specificity, and positive/negative likelihood ratios (+LR/-LR) of presenting symptoms and CTA findings of patients with and without vasculitis.
.jpg)
Table 3: Comparison of baseline laboratory values (P < 0.05 is statistically significant). CRP denotes C-reactive protein, WBC white blood cell count, Plt platelets, AST aspartate aminotransferase, ALT alanine aminotransferase, ALP alkaline phosphatase, and IQR interquartile range. CRP is in mg/L. AST, ALT, and ALP are in mg/dL. WBC and Plt are in K/µL.
J. haigney: None; L. Fandino: None; V. Kyttaris: AbbVie/Abbott, 5, AstraZeneca, 2, Aurinia, 1, EMD Serono, 5, Exagen, 2, 5, Fresenius Kabi, 1, Horizon Pharmaceuticals, 1, Novartis, 5, Scipher, 1, Takeda, 5, Vertex, 2.



