Poster Session A
Diversity, inclusion and racial disparities
Session: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
0182: Impact of Neighborhood-level Child Opportunity on Disease Activity in Children with Lupus
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
.png)
Joyce Chang, MD, MSCE (she/her/hers)
Boston Children's Hospital
Brookline, MA, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Joyce Chang1, Gabrielle Alonzi1, Emily Smitherman2, Pooja Patel3, Gabrielle Morgan4, Livie Huie5, Karen Costenbader6 and Mary Beth Son7, 1Boston Children's Hospital, Boston, MA, 2University of Alabama at Birmingham, Birmingham, AL, 3Ann and Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, 4Ann & Robert H. Lurie Children's Hospital of Chicago and Northwestern University Feinberg School of Medicine, Chicago, IL, 5University of Alabama at Birmingham, Gardendale, AL, 6Brigham and Women's Hospital and Harvard Medical School, Boston, MA, 7Division of Immunology, Boston Children's Hospital, Boston, MA
Background/Purpose: Racial disparities in outcomes of pediatric SLE (pSLE) have persisted over time. This may be mediated by structural racism, which segregates children belonging to minority groups into neighborhoods with lower childhood opportunity, defined as resources and conditions that promote healthy childhood development across domains of education, socioeconomics, and physical environment. We determined whether lower neighborhood-level opportunity associates with greater disease activity at initial SLE presentation or over time.
Methods: We conducted a cohort study of children newly diagnosed with SLE between 2016-2022, inclusive, in the Boston Children's Hospital Lupus Registry. The index visit was the first inpatient or outpatient rheumatology encounter with a physician diagnosis of SLE. The primary outcome was the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K). Geocoded addresses were linked to the Child Opportunity Index 2.0 (2015) by census tract and categorized as: very high, high, moderate, low, or very low opportunity, based on national and state level rankings. Median SLEDAI-2K at the index visit for children in each state-ranked COI category was compared to those living in very high COI areas using Wilcoxon rank sum tests. Associations between COI and disease activity over time were estimated using linear mixed effects models adjusted for time, insurance status, nephritis and neurologic involvement at presentation; additional covariates tested included age at SLE onset, sex assigned at birth, race and ethnicity, non-English primary language, and initial SLEDAI-2K.
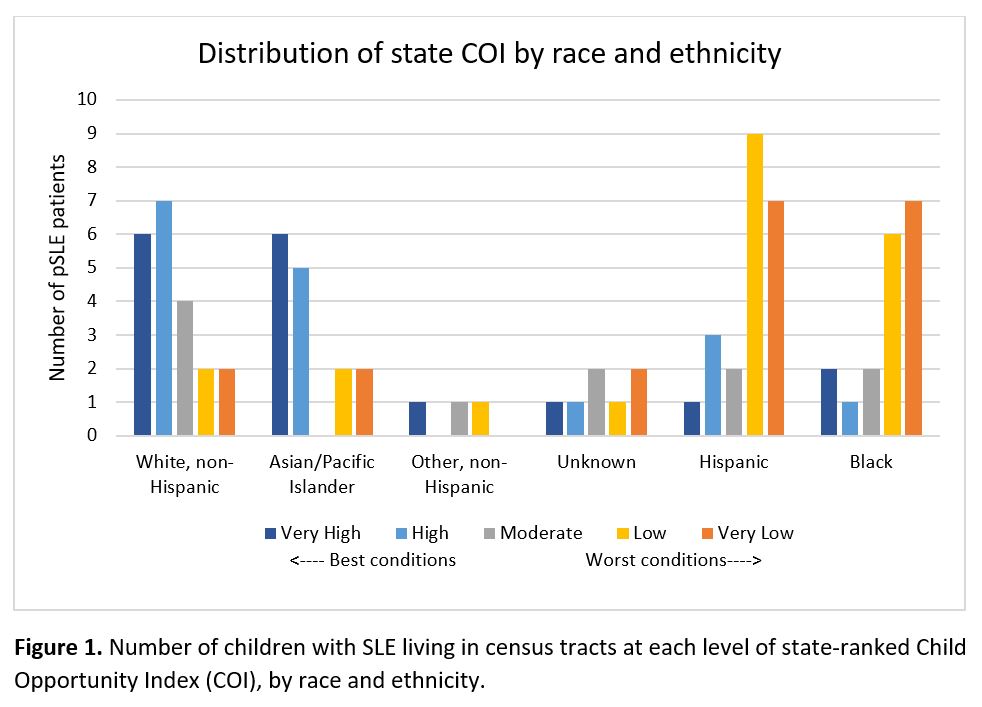
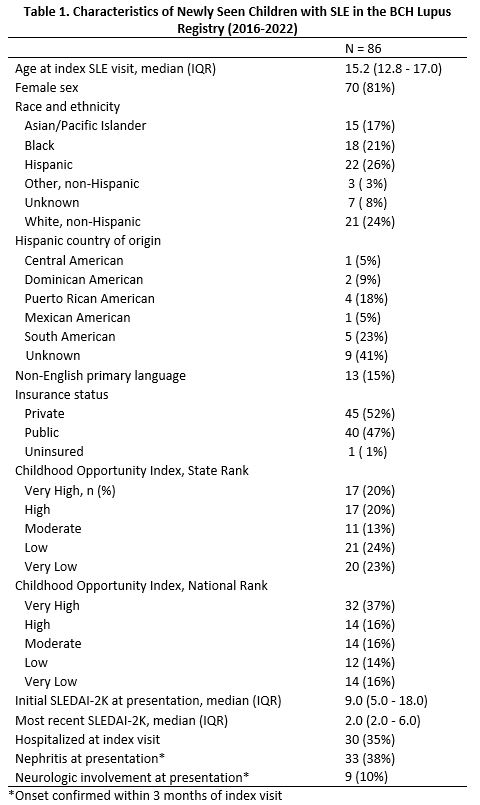
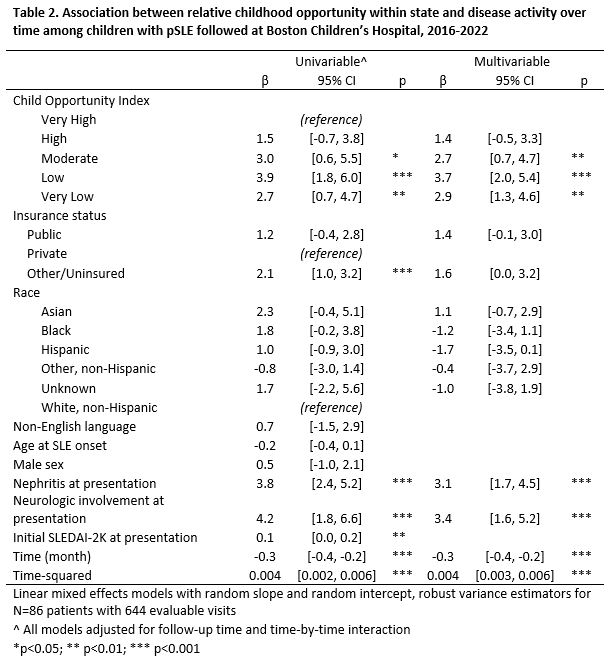
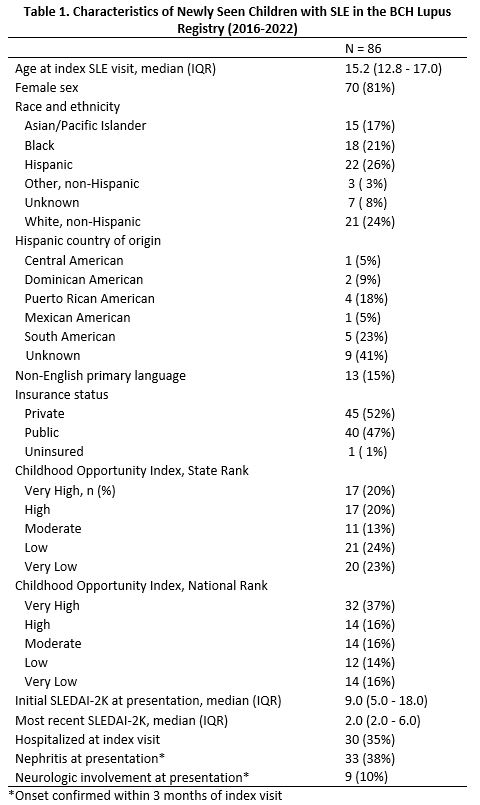
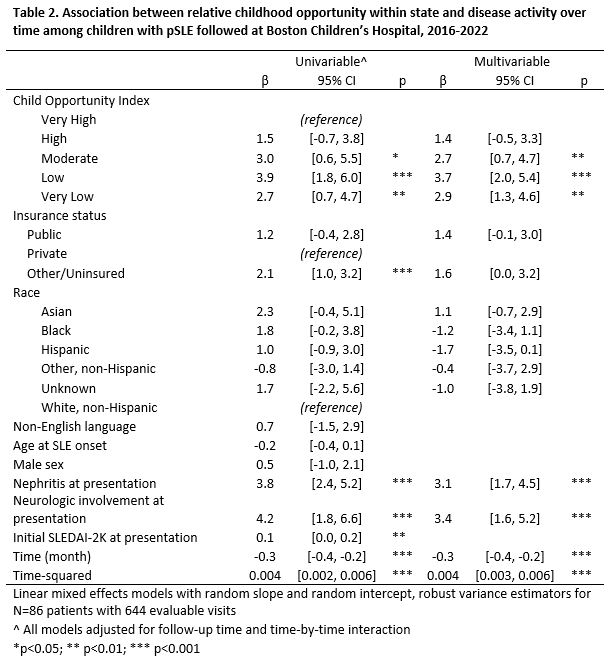
Results: We included 644 visits with calculable SLEDAI-2K scores, comprised by 86 patients with pSLE, with a median of 7 visits/patient [2-11] during the study period. The majority of Black (13/18, 72%) and Hispanic children (16/22, 73%) lived in low or very low state-ranked COI areas, whereas a 62% of Non-Hispanic White and 73% of Asian children lived in high or very high COI areas (Figure 1). In this cohort, nationally ranked COI was skewed towards very high (37%) and high (16%) average opportunity (Table 1). Children living in low opportunity areas ranked within state had higher SLEDAI scores at initial presentation compared to patients living in very high opportunity areas (median 14 [6-22] vs. 7 [4-8.5], p=0.03). Living in census tracts with moderate, low or very low COI (vs. very high) associated with significantly higher SLEDAI-2K over time compared to living in very high COI areas, both with or without adjustment for time, insurance status, race and ethnicity, and major organ involvement (Table 2). There was a significant test of trend (p=0.001). Results were similar when adjusting for initial SLEDAI-2K at presentation.
Conclusion: For children with pSLE in an area of the U.S. with high average opportunity levels, lower relative neighborhood-level childhood opportunity associated with higher SLE disease activity at initial presentation to care and during follow-up, independent of initial disease severity. Area-level conditions, among other factors in lower resourced areas, may mediate inequitable outcomes of pSLE at numerous points, including initial access to subspecialty care and after establishing care.
J. Chang: None; G. Alonzi: None; E. Smitherman: None; P. Patel: AbbVie/Abbott, 12, Site Principal Investagator, Pfizer, 12, Site Principal Investigator; G. Morgan: None; L. Huie: None; K. Costenbader: Amgen, 2, 5, AstraZeneca, 5, Bristol-Myers Squibb(BMS), 2, Cabaletta, 2, Eli Lilly, 2, Exagen Diagnostics, 5, Gilead, 5, GlaxoSmithKlein(GSK), 2, 5, Janssen, 2, 5; M. Son: None.
Background/Purpose: Racial disparities in outcomes of pediatric SLE (pSLE) have persisted over time. This may be mediated by structural racism, which segregates children belonging to minority groups into neighborhoods with lower childhood opportunity, defined as resources and conditions that promote healthy childhood development across domains of education, socioeconomics, and physical environment. We determined whether lower neighborhood-level opportunity associates with greater disease activity at initial SLE presentation or over time.
Methods: We conducted a cohort study of children newly diagnosed with SLE between 2016-2022, inclusive, in the Boston Children's Hospital Lupus Registry. The index visit was the first inpatient or outpatient rheumatology encounter with a physician diagnosis of SLE. The primary outcome was the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K). Geocoded addresses were linked to the Child Opportunity Index 2.0 (2015) by census tract and categorized as: very high, high, moderate, low, or very low opportunity, based on national and state level rankings. Median SLEDAI-2K at the index visit for children in each state-ranked COI category was compared to those living in very high COI areas using Wilcoxon rank sum tests. Associations between COI and disease activity over time were estimated using linear mixed effects models adjusted for time, insurance status, nephritis and neurologic involvement at presentation; additional covariates tested included age at SLE onset, sex assigned at birth, race and ethnicity, non-English primary language, and initial SLEDAI-2K.
Results: We included 644 visits with calculable SLEDAI-2K scores, comprised by 86 patients with pSLE, with a median of 7 visits/patient [2-11] during the study period. The majority of Black (13/18, 72%) and Hispanic children (16/22, 73%) lived in low or very low state-ranked COI areas, whereas a 62% of Non-Hispanic White and 73% of Asian children lived in high or very high COI areas (Figure 1). In this cohort, nationally ranked COI was skewed towards very high (37%) and high (16%) average opportunity (Table 1). Children living in low opportunity areas ranked within state had higher SLEDAI scores at initial presentation compared to patients living in very high opportunity areas (median 14 [6-22] vs. 7 [4-8.5], p=0.03). Living in census tracts with moderate, low or very low COI (vs. very high) associated with significantly higher SLEDAI-2K over time compared to living in very high COI areas, both with or without adjustment for time, insurance status, race and ethnicity, and major organ involvement (Table 2). There was a significant test of trend (p=0.001). Results were similar when adjusting for initial SLEDAI-2K at presentation.
Conclusion: For children with pSLE in an area of the U.S. with high average opportunity levels, lower relative neighborhood-level childhood opportunity associated with higher SLE disease activity at initial presentation to care and during follow-up, independent of initial disease severity. Area-level conditions, among other factors in lower resourced areas, may mediate inequitable outcomes of pSLE at numerous points, including initial access to subspecialty care and after establishing care.
J. Chang: None; G. Alonzi: None; E. Smitherman: None; P. Patel: AbbVie/Abbott, 12, Site Principal Investagator, Pfizer, 12, Site Principal Investigator; G. Morgan: None; L. Huie: None; K. Costenbader: Amgen, 2, 5, AstraZeneca, 5, Bristol-Myers Squibb(BMS), 2, Cabaletta, 2, Eli Lilly, 2, Exagen Diagnostics, 5, Gilead, 5, GlaxoSmithKlein(GSK), 2, 5, Janssen, 2, 5; M. Son: None.



