Abstract Session
Epidemiology, health policy and outcomes
Session: Abstracts: Epidemiology & Public Health II (2449–2454)
2453: Development of a Hydroxychloroquine Retinopathy Prediction Score
Tuesday, November 14, 2023
3:00 PM - 3:10 PM PT
Location: Room 6E/6D

April Jorge, MD
Massachusetts General Hospital
Boston, MA, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Presenting Author(s)
April Jorge1, Ronald Melles2, Baijun Zhou1, Yuqing Zhang3 and Hyon K. Choi4, 1Massachusetts General Hospital, Boston, MA, 2Kaiser Permanente Northern California, Redwood City, CA, 3Division of Rheumatology, Allergy, and Immunology, Department of Medicine, Massachusetts General Hospital, Boston, MA, 4Massachusetts General Hospital and Harvard Medical School, Lexington, MA
Background/Purpose: Hydroxychloroquine (HCQ) is an important medication for SLE and other rheumatic diseases, but its major adverse event is HCQ retinopathy. Weight-based HCQ dose is known to influence the risk of retinopathy, but other risk factors have also been identified. We explored predictive models for HCQ retinopathy and developed a clinical risk score.
Methods: We used a longitudinal cohort of incident HCQ users enrolled in the United States integrated health network Kaiser Permanente Northern California. HCQ retinopathy outcomes were obtained by masked expert-adjudication of optical coherence tomography screening studies, as previously described (Melles RB, Jorge A, Ann Int Med 2023). Among patients using HCQ for at least 5 years, we assessed candidate predictors at 5 years of use including the weight-based HCQ dose, cumulative dose in the first 5-years, age, sex, race/ethnicity, biometrics, indication for HCQ use, comorbidities including diabetes, liver disease, estimated glomerular filtration rate (eGFR), tamoxifen use, and use of inhibitors of cytochrome P450 CYP2D6, CYP2C8, or CYP3A4. We used Cox proportional hazards regression, using backwards stepwise selection to develop a parsimonious model, and an alternate method of random survival forest (RSF) to identify predictors of the 10-year risk of HCQ retinopathy (i.e., risk within 15 years from HCQ initiation). We created a comparator model using HCQ dose alone (weight-based dose at 5 years: > or ≤ 5 mg/kg). We assessed model discrimination with c-statistics, assessed model calibration using the Hosmer-Lemeshow statistic, and graphed deciles of predicted vs observed risk. We then developed an integer-based risk score from the optimal Cox model. Continuous variables were converted to categorical variables. We assessed net reclassification improvement and integrated discrimination improvement between the integer-based risk score and comparator model with HCQ dose alone.
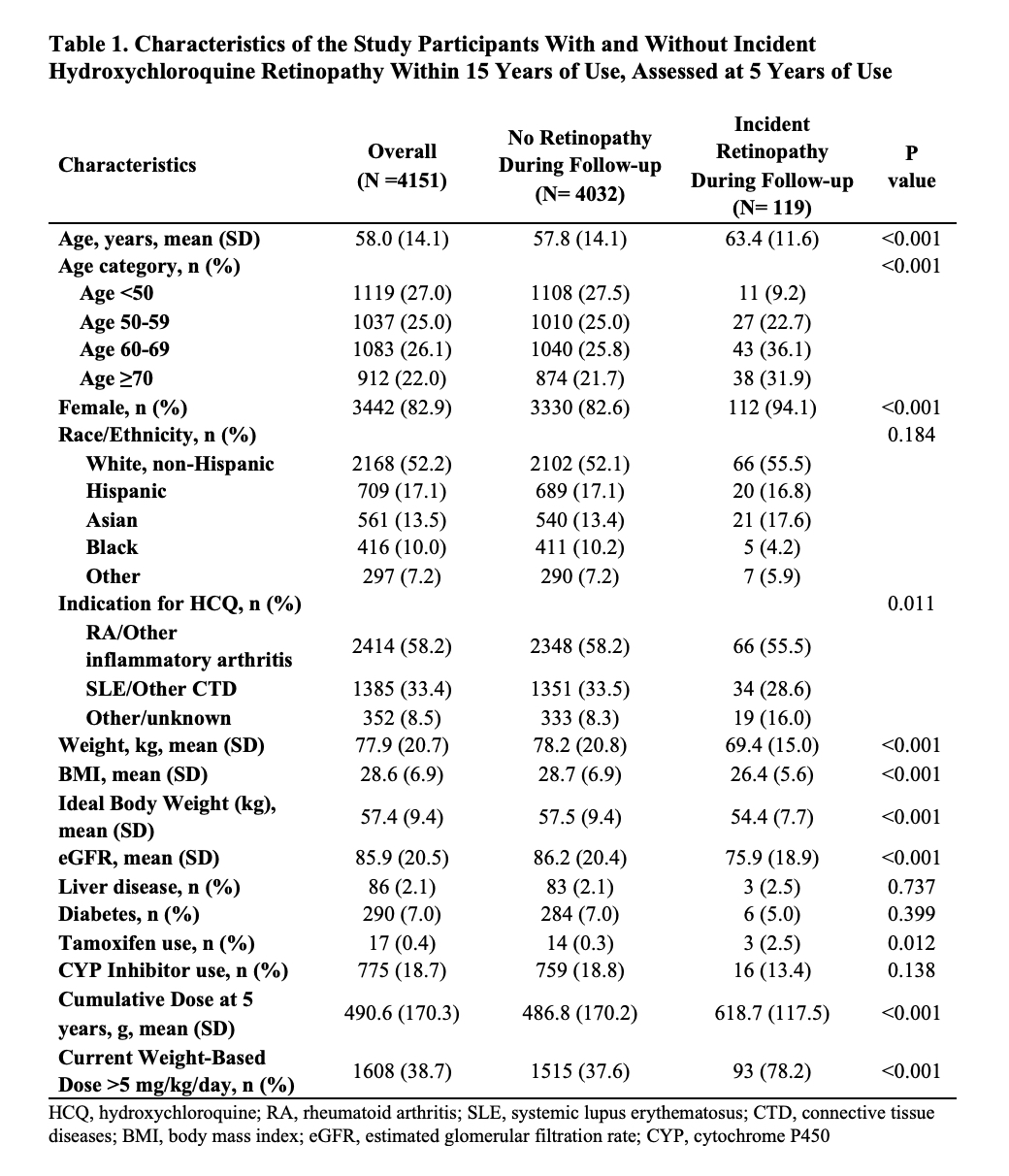
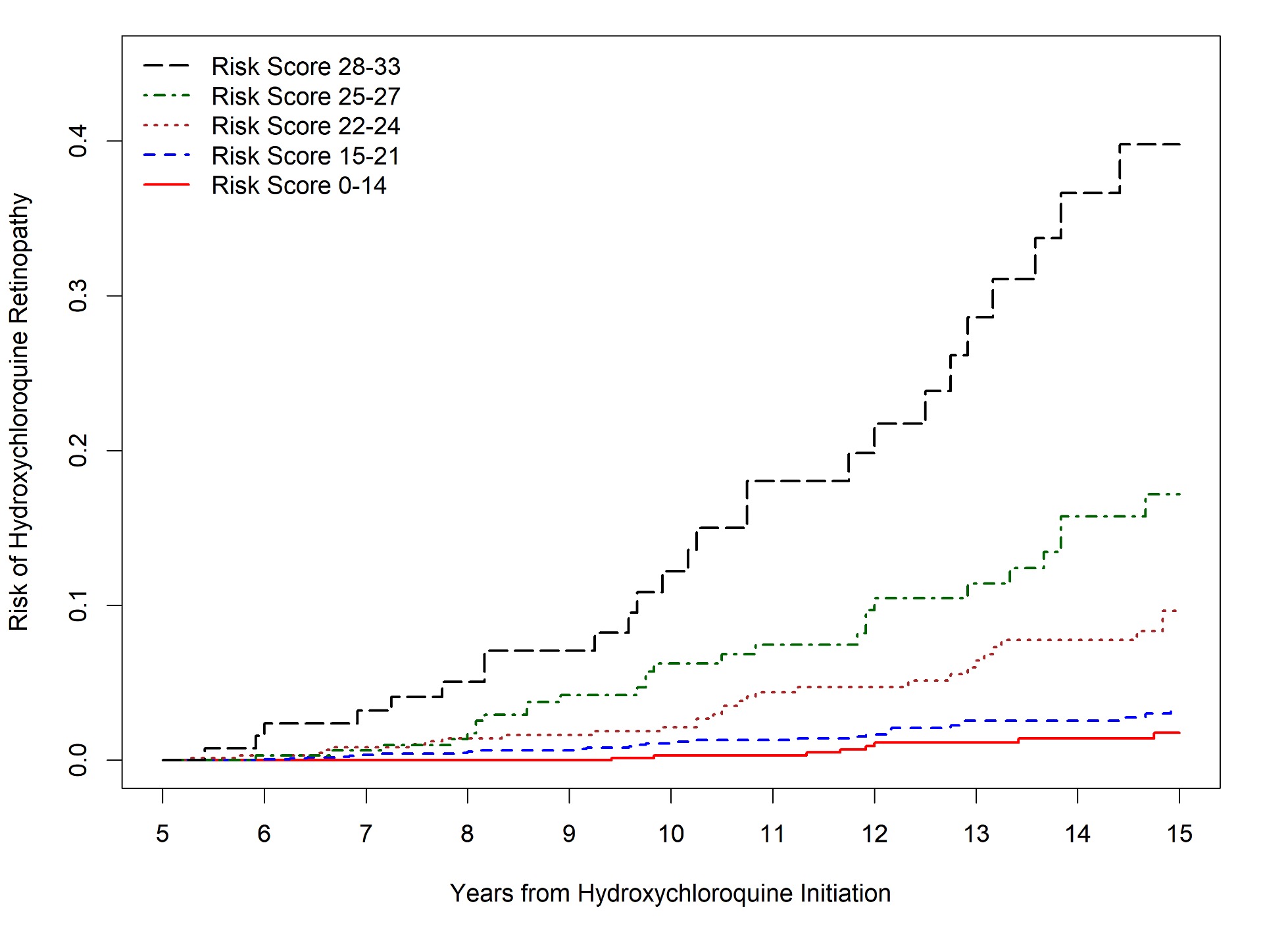
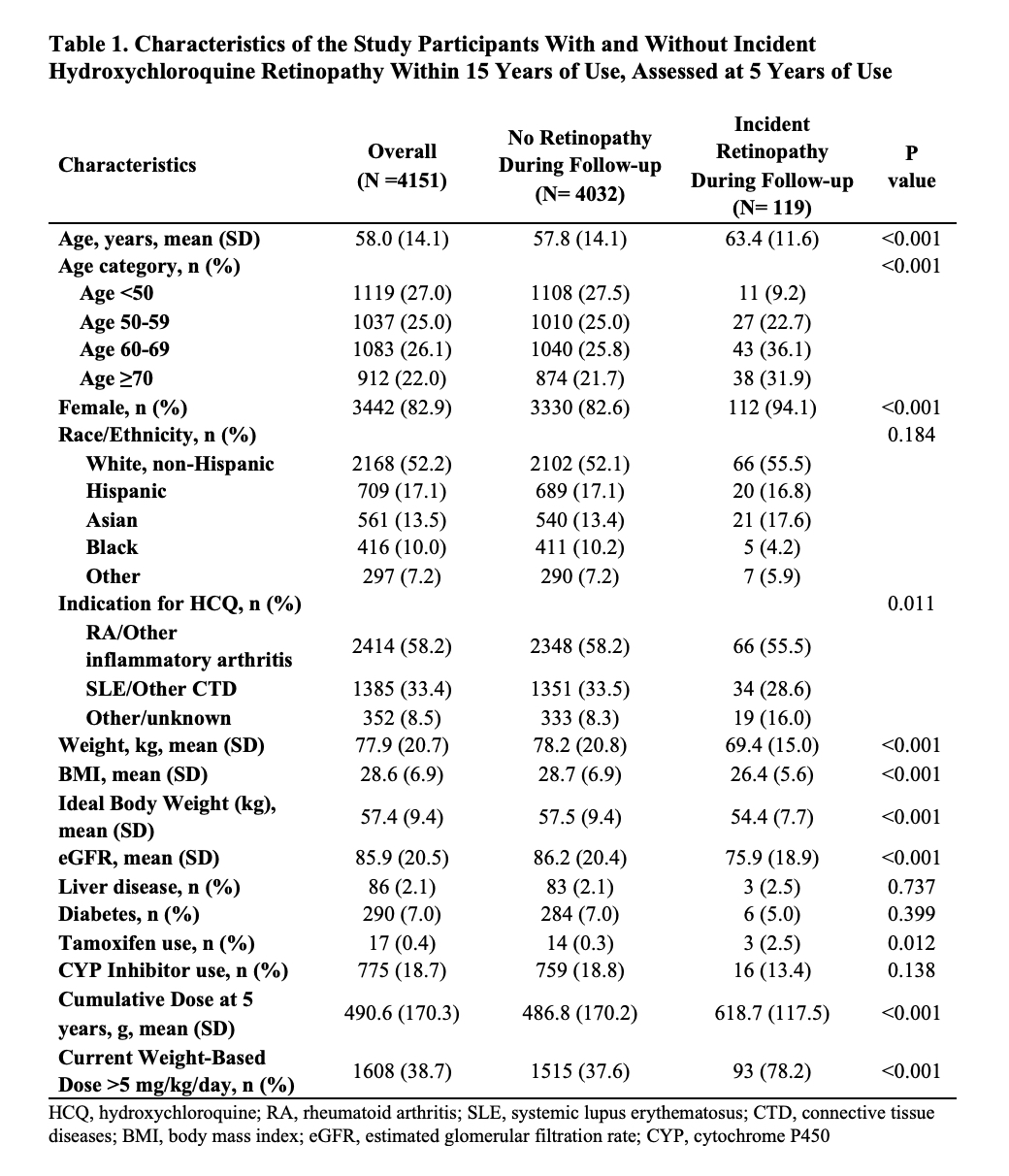
Results: Of 4,151 patients who initiated HCQ and continued for ≥5 years, 119 developed HCQ retinopathy within 15 years (Table 1). The final Cox model had better discrimination than the RSF model and than HCQ dose alone (C-statistic 0.80 [95% CI 0.77-0.83] versus 0.62 (95% CI 0.53-0.70) for the RSF model and 0.72 [95% CI 0.68-0.77] for the HCQ dose-only model. From the identified predictors in this model, an integer-based risk score for 10-year risk of HCQ retinopathy was created: B-SAFE (Body weight [kg], Sex, Age, glomerular Filtration rate, Exposure (cumulative dose in first 5 years since initiation [g] and current weight-based dose [mg/kg/day]). The B-SAFE model c-statistic was 0.78 (95% CI 0.75=0.82) with acceptable calibration (Figure 1). Compared with the HCQ dose-only model, the net reclassification index was 0.34 (95% CI 0.20-0.46). The risk score ranged from 0-33 points and can identify patients with HCQ retinopathy risk ranging from < 1% to >20% (Figure 2).
Conclusion: In addition to weight-based HCQ dose, we identified additional predictors of HCQ retinopathy. These clinical and laboratory variables were incorporated into a novel risk score that performs better than HCQ dose alone in predicting the 10-year risk of HCQ retinopathy among long-term users.
.jpg)
A. Jorge: None; R. Melles: None; B. Zhou: None; Y. Zhang: None; H. Choi: Ani, 2, Horizon, 2, 5, LG, 2, Protalix, 2, Shanton, 2.
Background/Purpose: Hydroxychloroquine (HCQ) is an important medication for SLE and other rheumatic diseases, but its major adverse event is HCQ retinopathy. Weight-based HCQ dose is known to influence the risk of retinopathy, but other risk factors have also been identified. We explored predictive models for HCQ retinopathy and developed a clinical risk score.
Methods: We used a longitudinal cohort of incident HCQ users enrolled in the United States integrated health network Kaiser Permanente Northern California. HCQ retinopathy outcomes were obtained by masked expert-adjudication of optical coherence tomography screening studies, as previously described (Melles RB, Jorge A, Ann Int Med 2023). Among patients using HCQ for at least 5 years, we assessed candidate predictors at 5 years of use including the weight-based HCQ dose, cumulative dose in the first 5-years, age, sex, race/ethnicity, biometrics, indication for HCQ use, comorbidities including diabetes, liver disease, estimated glomerular filtration rate (eGFR), tamoxifen use, and use of inhibitors of cytochrome P450 CYP2D6, CYP2C8, or CYP3A4. We used Cox proportional hazards regression, using backwards stepwise selection to develop a parsimonious model, and an alternate method of random survival forest (RSF) to identify predictors of the 10-year risk of HCQ retinopathy (i.e., risk within 15 years from HCQ initiation). We created a comparator model using HCQ dose alone (weight-based dose at 5 years: > or ≤ 5 mg/kg). We assessed model discrimination with c-statistics, assessed model calibration using the Hosmer-Lemeshow statistic, and graphed deciles of predicted vs observed risk. We then developed an integer-based risk score from the optimal Cox model. Continuous variables were converted to categorical variables. We assessed net reclassification improvement and integrated discrimination improvement between the integer-based risk score and comparator model with HCQ dose alone.
Results: Of 4,151 patients who initiated HCQ and continued for ≥5 years, 119 developed HCQ retinopathy within 15 years (Table 1). The final Cox model had better discrimination than the RSF model and than HCQ dose alone (C-statistic 0.80 [95% CI 0.77-0.83] versus 0.62 (95% CI 0.53-0.70) for the RSF model and 0.72 [95% CI 0.68-0.77] for the HCQ dose-only model. From the identified predictors in this model, an integer-based risk score for 10-year risk of HCQ retinopathy was created: B-SAFE (Body weight [kg], Sex, Age, glomerular Filtration rate, Exposure (cumulative dose in first 5 years since initiation [g] and current weight-based dose [mg/kg/day]). The B-SAFE model c-statistic was 0.78 (95% CI 0.75=0.82) with acceptable calibration (Figure 1). Compared with the HCQ dose-only model, the net reclassification index was 0.34 (95% CI 0.20-0.46). The risk score ranged from 0-33 points and can identify patients with HCQ retinopathy risk ranging from < 1% to >20% (Figure 2).
Conclusion: In addition to weight-based HCQ dose, we identified additional predictors of HCQ retinopathy. These clinical and laboratory variables were incorporated into a novel risk score that performs better than HCQ dose alone in predicting the 10-year risk of HCQ retinopathy among long-term users.
.jpg)
Figure 1. Calibration of the B-SAFE risk score model. Predicted vs. observed 10-year incidence of hydroxychloroquine retinopathy based on deciles of predicted risk. Hosmer-Lemeshow statistic x2 =3.19, P =0.67. Q1 to Q10 refer to deciles of risk score.
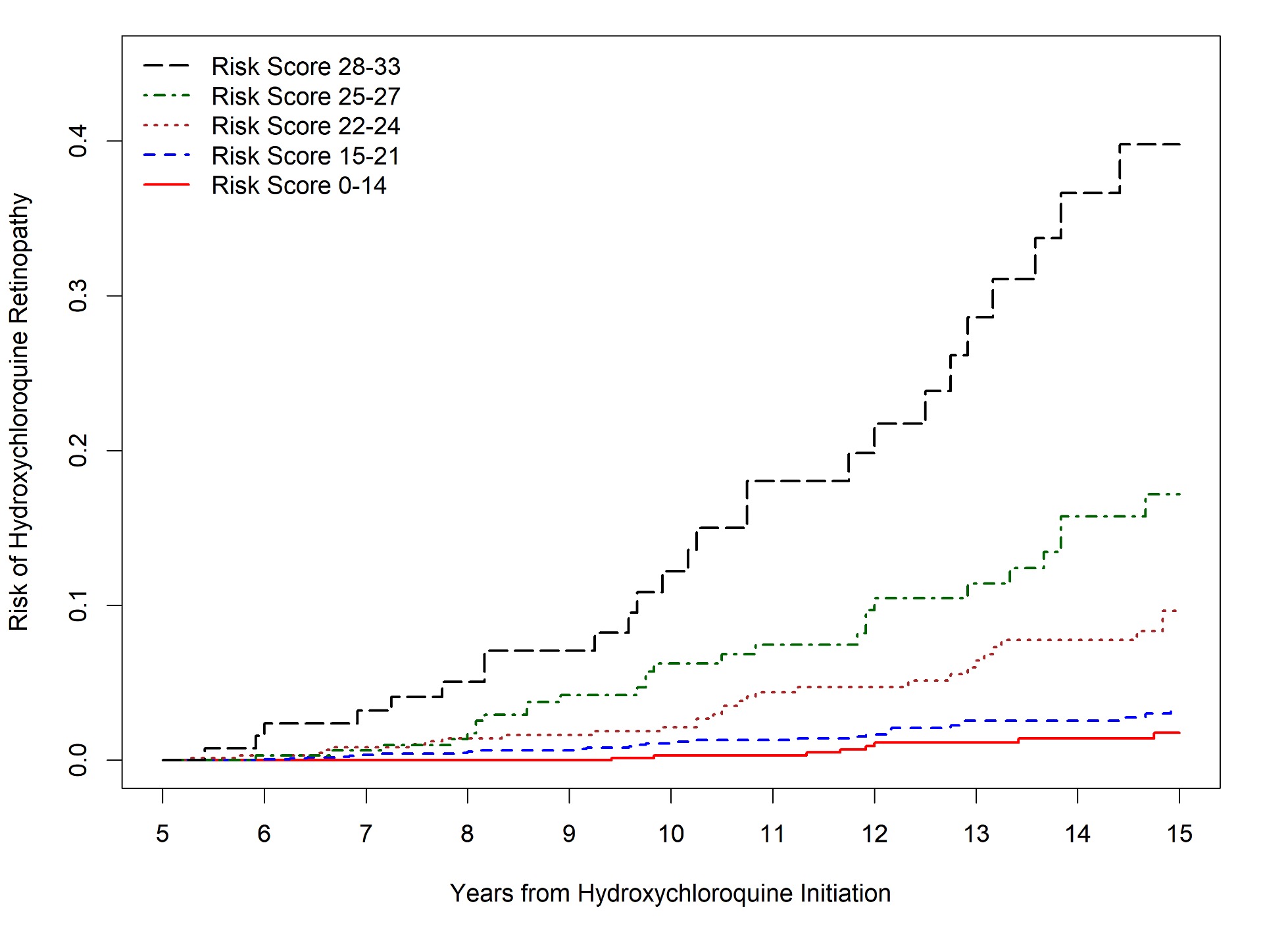
Figure 2. Cumulative Incidence of HCQ Retinopathy According to Risk Score Groups. Risk scores were divided into 5-groups based on 10-year retinopathy risk, ranging from <1% corresponding with scores 0-14, 1-5% corresponding with scores 15-21, >5-10% corresponding with scores 22-24, >10-20% corresponding with scores 25-27, and >20% corresponding with scores 28-33.
A. Jorge: None; R. Melles: None; B. Zhou: None; Y. Zhang: None; H. Choi: Ani, 2, Horizon, 2, 5, LG, 2, Protalix, 2, Shanton, 2.



