Poster Session A
Diversity, inclusion and racial disparities
Session: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
0179: Social Disparities and Pathology Markers at Lupus Nephritis Diagnosis Predict Worse Kidney Outcomes
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- SG
Shivani Garg, MD, MS
University of Madison, School of Medicine and Public Health
Madison, WI, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Shivani Garg1, Brad Astor2, Amish Raval2, S. Sam Lim3, Weixiong Zhong2, Sarah Panzer2, Brad Rovin4 and Christie M. Bartels2, 1Department of Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI, 2University of Wisconsin, School of Medicine and Public Health, Madison, WI, 3Emory University, Atlanta, GA, 4Ohio State University, Columbus, OH
Background/Purpose: At diagnosis, a typical 30-year-old with lupus nephritis (LN) already has 10-fold higher chronic kidney disease (CKD) risk than peers and LN is a leading cause of end-stage kidney disease (ESKD) in young patients. Moreover, Black race is associated with a 6-fold higher risk of developing LN associated ESKD suggesting interactions between biological, socio-economic, and pathological factors can accelerate CKD progression and ESKD risk in LN. Examining early risk factors and interactions between socio-economic and biological factors can improve precision in identifying high-risk patients, yet these are under-examined in LN. Thus, we examined socio-economic and biological factors at LN diagnosis, and pathological markers in index kidney biopsies as predictors of CKD progression and ESKD among a longitudinal inception LN cohort.
Methods: Data including demographics, social factors, comorbidities, LN therapy, and pathology reports at LN diagnosis were abstracted from adult LN patients who underwent index kidney biopsy between 1994-2021. We abstracted LN chronicity and activity indices from index kidney biopsy slides and reports, and re-read biopsy slides to grade renal arteriosclerosis (ASCL) by calculating percent luminal narrowing. We measured two outcomes: a) time to CKD progression defined as a sustained decrease in eGFR ≥30% below the baseline, confirmed by ≥3 values for ≥ 3 months and progression to CKD stage ≥2 (eGFR < 90); b) time to ESKD with up to 12 years follow-up. Cox hazards models and Kaplan Meier (KM) survival analyses were used to examine whether socio-economic factors and pathology markers such as ASCL and activity and chronicity indices predict CKD progression and ESKD.
Results: Among 173 incident adult patients with LN, 75% were female and 35% were from Black and other racial groups. Mean age at LN diagnosis was 38±17 years, and 46% had public or no insurance. Mean renal ASCL (percent luminal narrowing), activity, and chronicity indices were 23%, 2.2, 1.9, respectively.
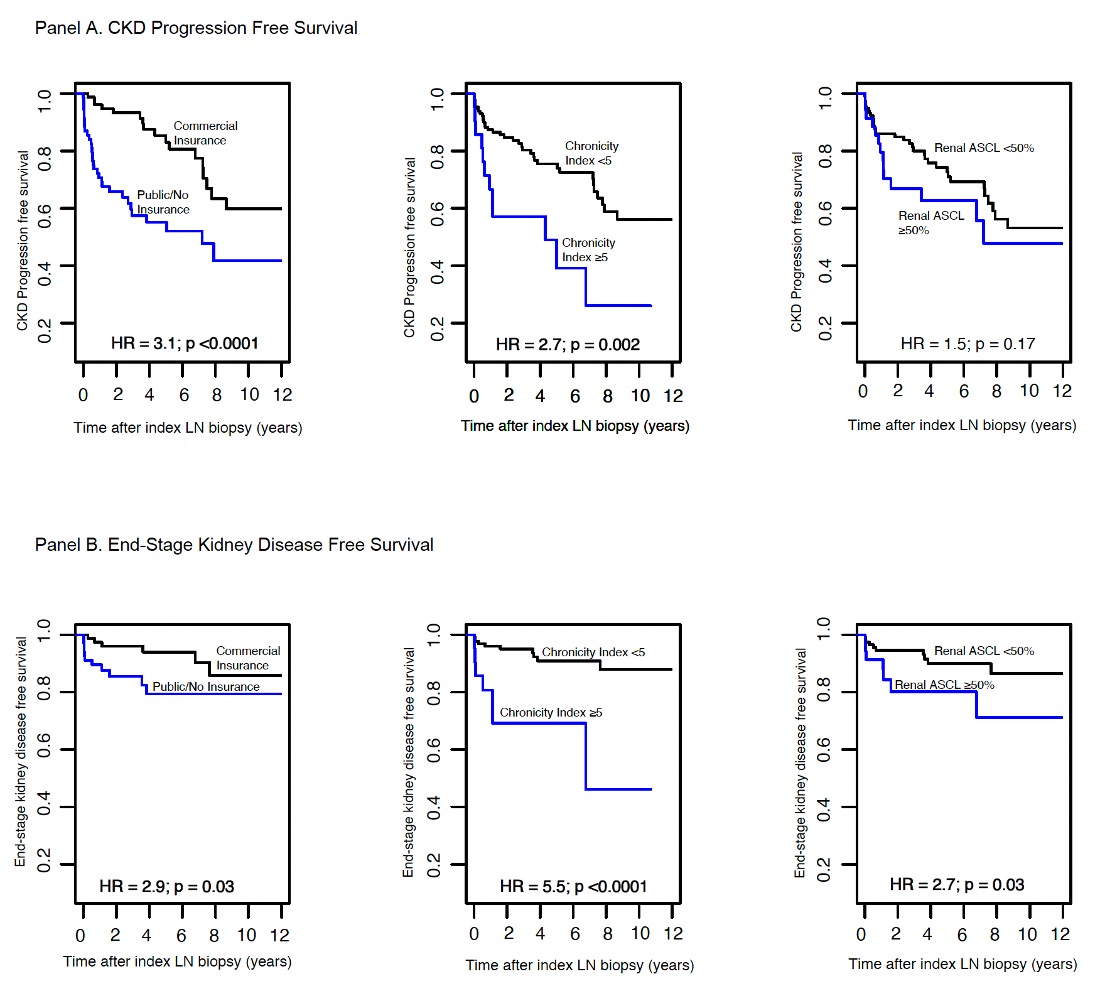
A total of 49 patients developed CKD progression over 12 years after LN diagnosis. KM survival curves highlighted accelerated CKD progression in patients with public or no insurance and LN chronicity index ≥5 (Fig. 1A). Patients with public or no insurance had 2-fold higher risk of CKD progression (Adjusted HR 2.2; Table 1). Increase in LN chronicity determined 40% higher CKD progression (Table 1).
Next, 19 patients developed ESKD. KM survival curves noted higher ESKD risk in patients with public or no insurance, severe renal ASCL, and LN chronicity index ≥5 at diagnosis (Fig. 1B). In a limited multivariable model, not including LN chronicity, severe renal ASCL was associated with 2.7 fold higher ESKD risk (Table 2). However, after including LN chronicity, only LN chronicity was associated with 40% higher ESKD risk (Table 2).
Conclusion: Socioeconomic barriers such as public or no insurance at diagnosis were the strongest, independent risk factor of CKD progression to stage ≥2. Additionally, higher LN chronicity in diagnostic biopsies was associated with greater ESKD risk. Future CKD prevention efforts should focus on patients with socioeconomic barriers and those with high LN chronicity index at LN diagnosis to improve outcomes in LN.
.jpg)
.jpg)
S. Garg: None; B. Astor: None; A. Raval: None; S. Lim: None; W. Zhong: None; S. Panzer: None; B. Rovin: AstraZeneca, 2, 5, Aurinia, 2, 5, Biogen, 2, F. Hoffmann-La Roche Ltd, 2, Genentech, 2, GlaxoSmithKlein(GSK), 2, Novartis, 2; C. Bartels: Pfizer, 5.
Background/Purpose: At diagnosis, a typical 30-year-old with lupus nephritis (LN) already has 10-fold higher chronic kidney disease (CKD) risk than peers and LN is a leading cause of end-stage kidney disease (ESKD) in young patients. Moreover, Black race is associated with a 6-fold higher risk of developing LN associated ESKD suggesting interactions between biological, socio-economic, and pathological factors can accelerate CKD progression and ESKD risk in LN. Examining early risk factors and interactions between socio-economic and biological factors can improve precision in identifying high-risk patients, yet these are under-examined in LN. Thus, we examined socio-economic and biological factors at LN diagnosis, and pathological markers in index kidney biopsies as predictors of CKD progression and ESKD among a longitudinal inception LN cohort.
Methods: Data including demographics, social factors, comorbidities, LN therapy, and pathology reports at LN diagnosis were abstracted from adult LN patients who underwent index kidney biopsy between 1994-2021. We abstracted LN chronicity and activity indices from index kidney biopsy slides and reports, and re-read biopsy slides to grade renal arteriosclerosis (ASCL) by calculating percent luminal narrowing. We measured two outcomes: a) time to CKD progression defined as a sustained decrease in eGFR ≥30% below the baseline, confirmed by ≥3 values for ≥ 3 months and progression to CKD stage ≥2 (eGFR < 90); b) time to ESKD with up to 12 years follow-up. Cox hazards models and Kaplan Meier (KM) survival analyses were used to examine whether socio-economic factors and pathology markers such as ASCL and activity and chronicity indices predict CKD progression and ESKD.
Results: Among 173 incident adult patients with LN, 75% were female and 35% were from Black and other racial groups. Mean age at LN diagnosis was 38±17 years, and 46% had public or no insurance. Mean renal ASCL (percent luminal narrowing), activity, and chronicity indices were 23%, 2.2, 1.9, respectively.
A total of 49 patients developed CKD progression over 12 years after LN diagnosis. KM survival curves highlighted accelerated CKD progression in patients with public or no insurance and LN chronicity index ≥5 (Fig. 1A). Patients with public or no insurance had 2-fold higher risk of CKD progression (Adjusted HR 2.2; Table 1). Increase in LN chronicity determined 40% higher CKD progression (Table 1).
Next, 19 patients developed ESKD. KM survival curves noted higher ESKD risk in patients with public or no insurance, severe renal ASCL, and LN chronicity index ≥5 at diagnosis (Fig. 1B). In a limited multivariable model, not including LN chronicity, severe renal ASCL was associated with 2.7 fold higher ESKD risk (Table 2). However, after including LN chronicity, only LN chronicity was associated with 40% higher ESKD risk (Table 2).
Conclusion: Socioeconomic barriers such as public or no insurance at diagnosis were the strongest, independent risk factor of CKD progression to stage ≥2. Additionally, higher LN chronicity in diagnostic biopsies was associated with greater ESKD risk. Future CKD prevention efforts should focus on patients with socioeconomic barriers and those with high LN chronicity index at LN diagnosis to improve outcomes in LN.
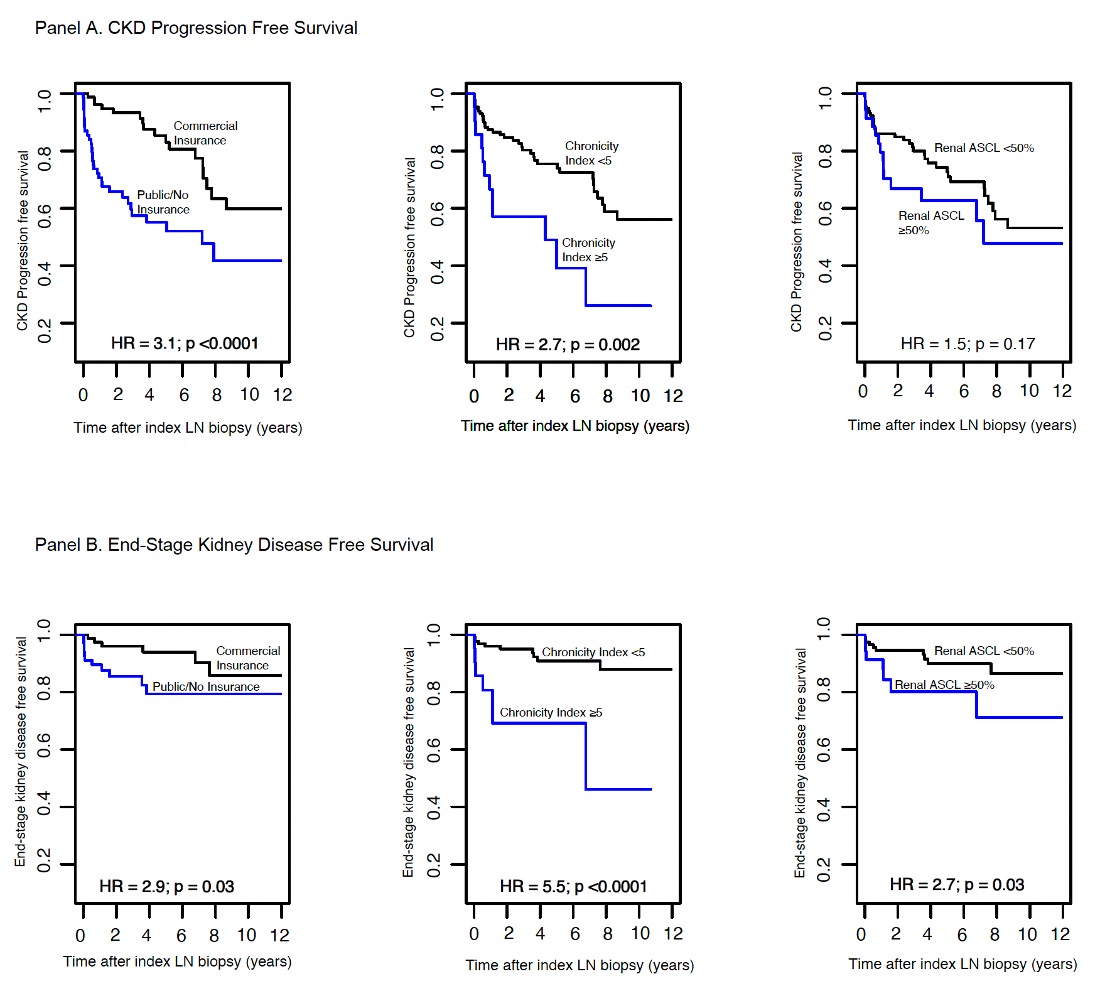
Figure 1. Kaplan Meier Curve shows: Panel A. CKD progression defined as kidney function impairment with sustained decrease in eGFR by 30% and eGFR <90 (CKD stage ≥2); Panel B. ESKD occurrence over 12-year follow-up period after LN diagnosis.
.jpg)
Table 1. Cox models showing risk factors at LN diagnosis of CKD progression defined as kidney function impairment with sustained decrease in eGFR by 30% and eGFR <90 (CKD stage ≥2) (Moroni et al., Kidney360, 2022)
.jpg)
Table 2. Cox models showing risk factors at LN diagnosis for end-stage kidney disease (ESKD) over 12 years follow up.
S. Garg: None; B. Astor: None; A. Raval: None; S. Lim: None; W. Zhong: None; S. Panzer: None; B. Rovin: AstraZeneca, 2, 5, Aurinia, 2, 5, Biogen, 2, F. Hoffmann-La Roche Ltd, 2, Genentech, 2, GlaxoSmithKlein(GSK), 2, Novartis, 2; C. Bartels: Pfizer, 5.



