Poster Session A
Juvenile idiopathic arthritis (JIA) and pediatric joint disorders
Session: (0345–0379) Pediatric Rheumatology – Clinical Poster I: JIA
0348: The Use of Ruxolitinib for Improved Disease Control in Systemic Juvenile Idiopathic Arthritis (sJIA) and Recurrent Macrophage Activation Syndrome (MAS)
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- MH
Melissa Hines, MD
St Jude Children's Research Hospital
Memphis, TN, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Kathleen Collins1, Iman Abutineh1, Trisha Paul2, Parul Rai3, Grant Schulert4 and Melissa Hines2, 1University of Tennessee Health Science Center, Memphis, TN, 2St Jude Children's Research Hospital, Memphis, TN, 3St Jude Children's Reseaerch Hospital, Memphis, TN, 4Cincinnati Children's Hospital Medical Center, Cincinnati, OH
Background/Purpose: The advent of biologics such as IL-1 receptor antagonists has dramatically improved outcomes for children with pediatric rheumatic diseases and hyperinflammation. However, there remains a subset of patients with systemic juvenile idiopathic arthritis (sJIA) who develop life-threatening complications of macrophage activation syndrome (MAS) and interstitial lung disease (ILD) despite treatment with glucocorticoids and IL-1 inhibition. Recent findings point to robust interferon and IL-18 signature as drivers of persistent inflammation in sJIA, suggesting a potential role for inhibition of these pathways using Janus kinase inhibitors, such as ruxolitinib, as a viable therapeutic strategy.
Methods: We completed a retrospective chart review on three patients with sJIA or sJIA-like disease started on ruxolitinib for improved disease control or to allow for glucocorticoid weaning.
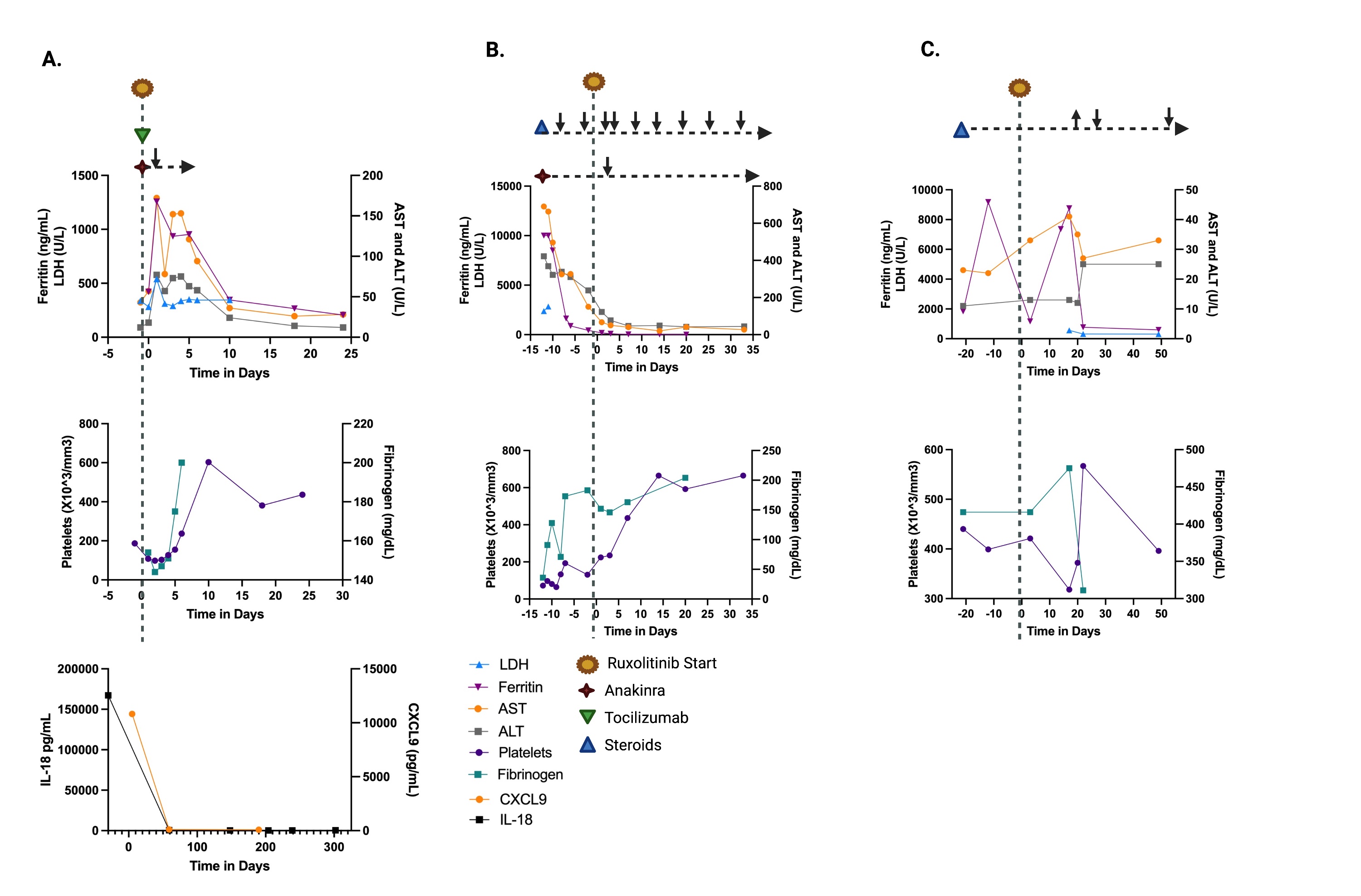
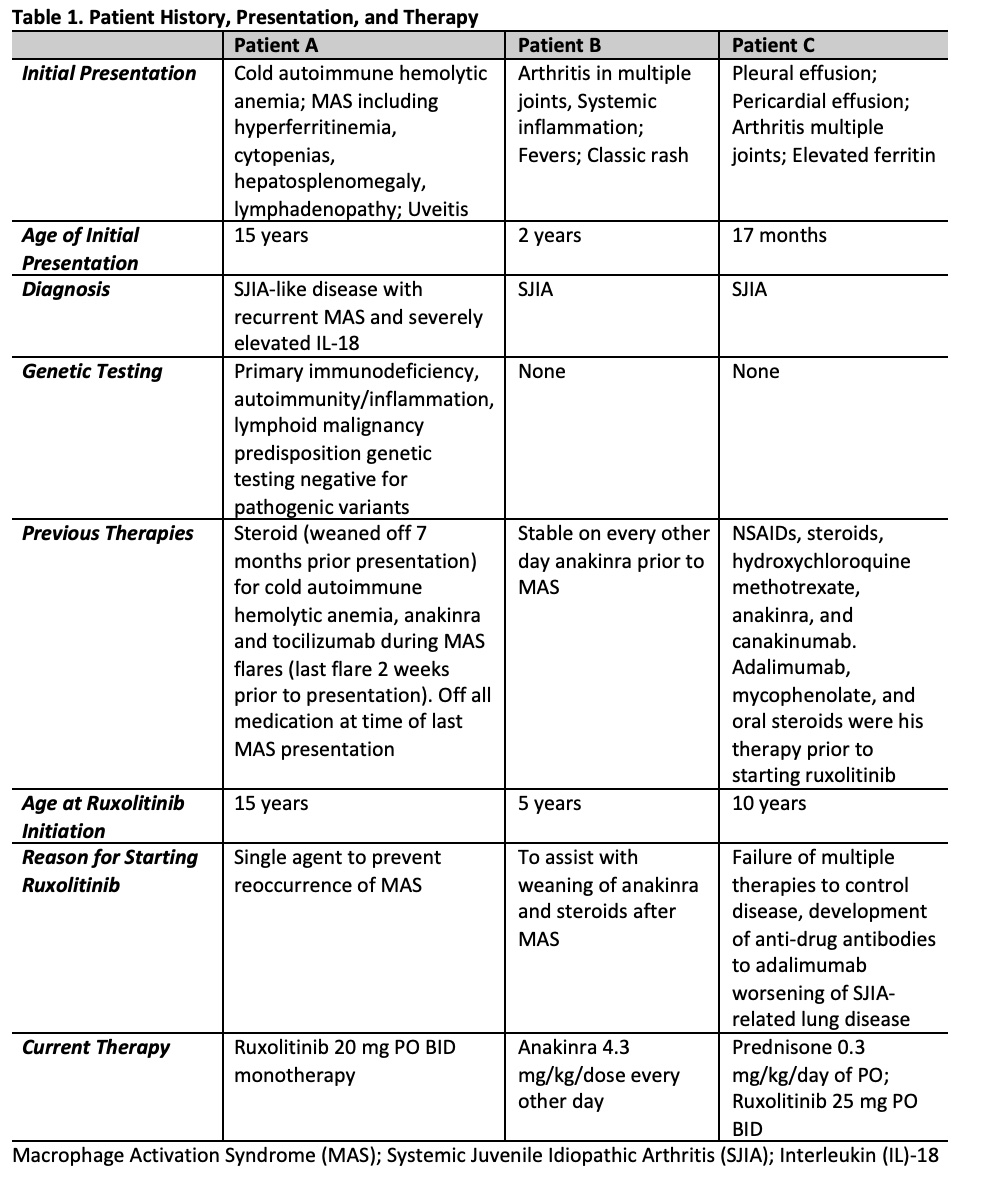
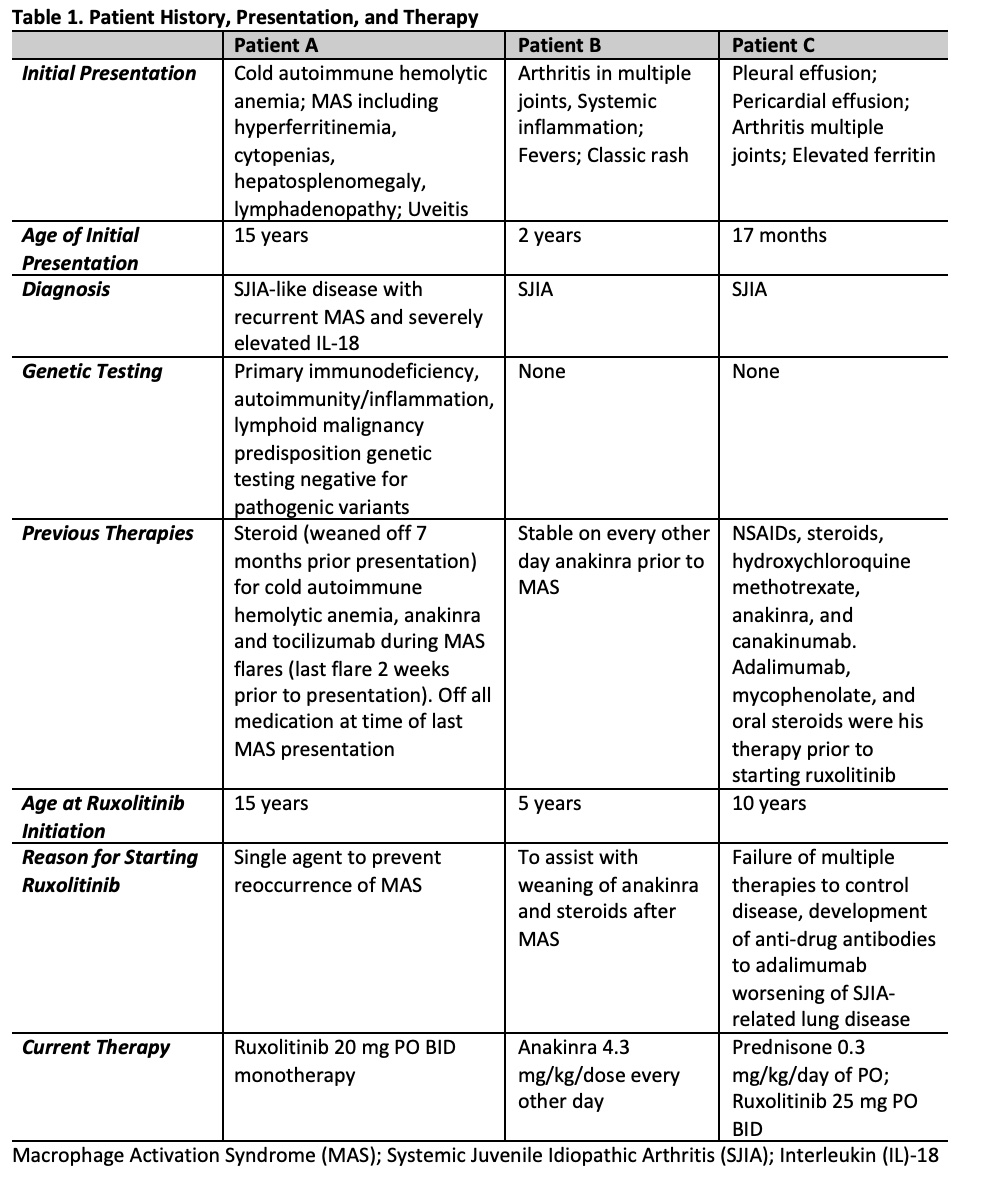
Results: Patients ages were 5-15 years of age with 2 females and 1 male (Table 1). Patient A with sJIA-like disease presented with recurrent MAS with fever and hypotension requiring vasopressor support and was treated with ruxolitinib, anakinra, and tocilizumab and MAS was controlled (Figure 1). Anakinra was weaned off prior to discharge home. Ruxolitinib was continued as a single agent and has maintained excellent control of the patient's disease with no further MAS flares or adverse events for the last 10 months. Patient B with previously diagnosed sJIA presented with fulminant MAS secondary to EBV. She was treated with pulse dose steroids and anakinra with some initial stabilization. Ruxolitinib was started due to lack of further improvement in MAS. The addition of ruxolitinib controlled her MAS and steroid and anakinra doses were tapered (Table 2; Figure 1). Oral steroids were discontinued 9 weeks after starting ruxolitinib. Ruxolitinib was discontinued at 3 months. Patient was continued on anakinra. Patient C with previously diagnosed sJIA developed sJIA-associated lung disease on canakinumab therapy. Ruxolitinib was added to his therapy (Table 1, 2) due to continued systemic inflammation and inability to wean steroids. Within the 4 weeks the patient reported improvement in joint pain and had no oxygen desaturations with walking. Within 6 weeks, lung function improved with FEV1 increasing from 85% to 91% predicted. Ruxolitinib dose was increased to 25 mg twice a day at 4 months based on patient toleration and to optimize disease control, allowing successful weaning of steroids by 50%. Patients have not had any infectious complications while on ruxoltinib. One adverse event reported was Grade 1 elevated cholesterol. Mean follow-up time is 214 days (146-322). Mean time patients were on ruxolitinib was 189 days (100-322).
Conclusion: Ruxolitinib was well tolerated in these patients with sJIA or sJIA-like disease with no significant adverse events, including cytopenias, transaminitis, or infections. Use of ruxoltinib provided improved disease control as a single agent or in combination with other immunomodulators and allowed reduction of other therapies, such as steroids. Based on our experience, patients may require and can tolerate higher doses than previously used for other indications with titration up and down to affect.
.jpg)
K. Collins: None; I. Abutineh: None; T. Paul: None; P. Rai: None; G. Schulert: IpiNovyx, 5, SOBI, 2; M. Hines: Incyte, 5.
Background/Purpose: The advent of biologics such as IL-1 receptor antagonists has dramatically improved outcomes for children with pediatric rheumatic diseases and hyperinflammation. However, there remains a subset of patients with systemic juvenile idiopathic arthritis (sJIA) who develop life-threatening complications of macrophage activation syndrome (MAS) and interstitial lung disease (ILD) despite treatment with glucocorticoids and IL-1 inhibition. Recent findings point to robust interferon and IL-18 signature as drivers of persistent inflammation in sJIA, suggesting a potential role for inhibition of these pathways using Janus kinase inhibitors, such as ruxolitinib, as a viable therapeutic strategy.
Methods: We completed a retrospective chart review on three patients with sJIA or sJIA-like disease started on ruxolitinib for improved disease control or to allow for glucocorticoid weaning.
Results: Patients ages were 5-15 years of age with 2 females and 1 male (Table 1). Patient A with sJIA-like disease presented with recurrent MAS with fever and hypotension requiring vasopressor support and was treated with ruxolitinib, anakinra, and tocilizumab and MAS was controlled (Figure 1). Anakinra was weaned off prior to discharge home. Ruxolitinib was continued as a single agent and has maintained excellent control of the patient's disease with no further MAS flares or adverse events for the last 10 months. Patient B with previously diagnosed sJIA presented with fulminant MAS secondary to EBV. She was treated with pulse dose steroids and anakinra with some initial stabilization. Ruxolitinib was started due to lack of further improvement in MAS. The addition of ruxolitinib controlled her MAS and steroid and anakinra doses were tapered (Table 2; Figure 1). Oral steroids were discontinued 9 weeks after starting ruxolitinib. Ruxolitinib was discontinued at 3 months. Patient was continued on anakinra. Patient C with previously diagnosed sJIA developed sJIA-associated lung disease on canakinumab therapy. Ruxolitinib was added to his therapy (Table 1, 2) due to continued systemic inflammation and inability to wean steroids. Within the 4 weeks the patient reported improvement in joint pain and had no oxygen desaturations with walking. Within 6 weeks, lung function improved with FEV1 increasing from 85% to 91% predicted. Ruxolitinib dose was increased to 25 mg twice a day at 4 months based on patient toleration and to optimize disease control, allowing successful weaning of steroids by 50%. Patients have not had any infectious complications while on ruxoltinib. One adverse event reported was Grade 1 elevated cholesterol. Mean follow-up time is 214 days (146-322). Mean time patients were on ruxolitinib was 189 days (100-322).
Conclusion: Ruxolitinib was well tolerated in these patients with sJIA or sJIA-like disease with no significant adverse events, including cytopenias, transaminitis, or infections. Use of ruxoltinib provided improved disease control as a single agent or in combination with other immunomodulators and allowed reduction of other therapies, such as steroids. Based on our experience, patients may require and can tolerate higher doses than previously used for other indications with titration up and down to affect.
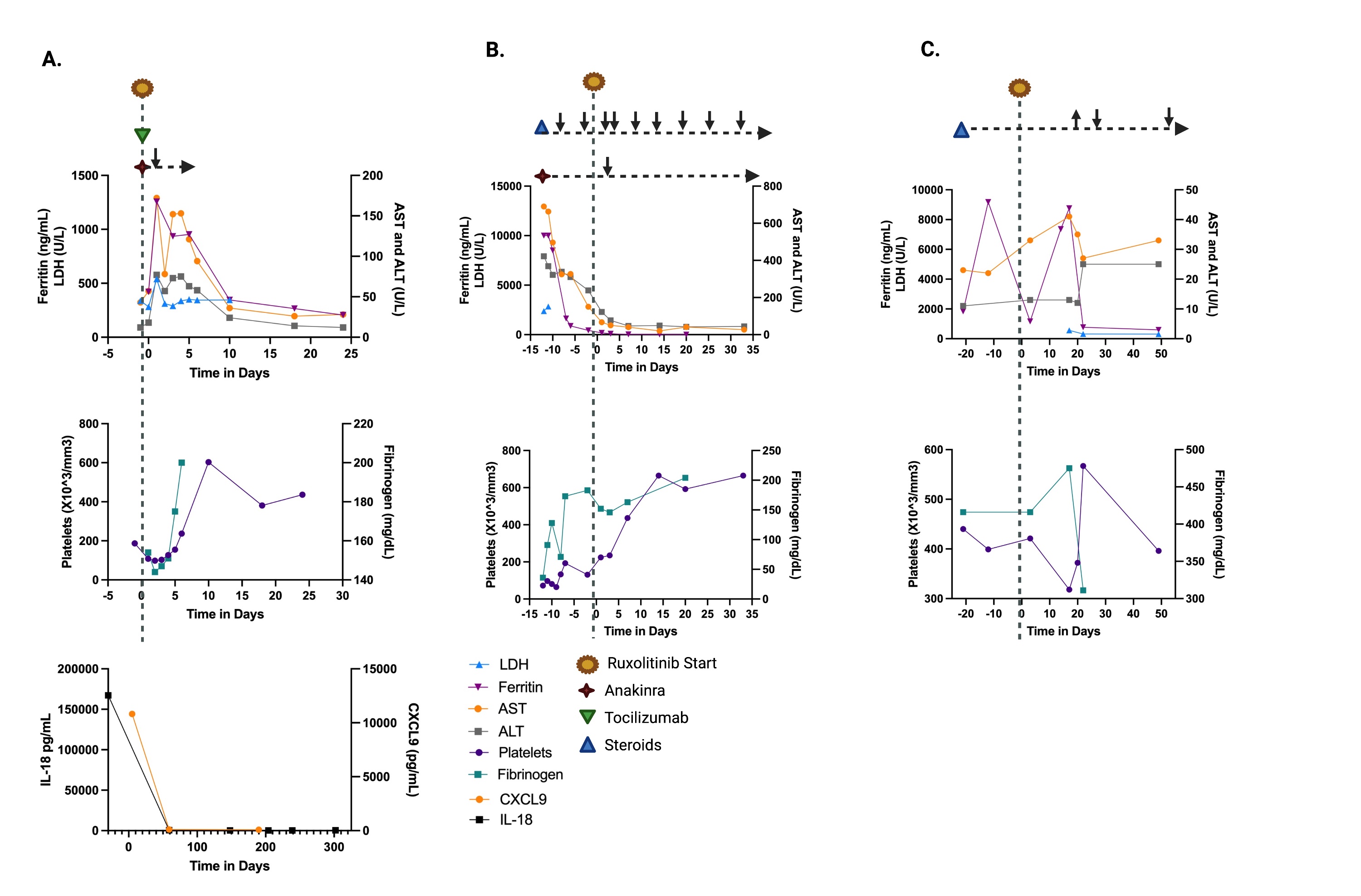
Figure 1. Clinical Details. Day 0 represents first day of ruxolitinib in all patients. Overall, patients had improvement in cytopenias and transaminitis if present. A. On Day 0, patient required ICU admission for MAS with hypotension and fever and was given tocilizumab 800 mg once, ruxolitinib, and anakinra 100 mg q6h (weaned off by day 5). Patient had improvement in ferritin, cytopenias, and transaminitis within 15 days. Patient had significant improvement in IL-18 and CXCL9 levels with continued ruxolitinib monotherapy. B. On day -12, patient was admitted for MAS related to EBV and had initial improvement in ferritin, thrombocytopenia, hypofibrinogenemia and transaminitis with a single dose of rituximab (to aid with EBV clearance), anakinra 12.5 mg/kg/day divided IV q6h and pulse dose steroids (30 mg/kg x 3 days). There was some initial improvement of MAS, but team was unable to wean steroids or anakinra. Ruxolitinib was started which allowed for anakinra to be weaned to 6.25 mg/kg/day SQ dosing by day 3. Patient was discharged on ruxolitinib, anakinra 6.25 mg/kg/day once a day, and 1.5 mg/kg/day prednisolone. While on ruxolitinib, patient continued to tolerate steroid weans as an outpatient. C. Patient was started on ruxolitinib in addition to oral steroids, adalimumab, and mycophenolate for management of SJIA with lung involvement. Patient tolerated slow wean of steroids (methylprednisolone 40 mg/day max to prednisone 15 mg/day) over the course of 4 months. Figure created with GraphPad PRISM and Biorender.
.jpg)
K. Collins: None; I. Abutineh: None; T. Paul: None; P. Rai: None; G. Schulert: IpiNovyx, 5, SOBI, 2; M. Hines: Incyte, 5.



