Poster Session A
Systemic lupus erythematosus (SLE)
Session: (0543–0581) SLE – Diagnosis, Manifestations, & Outcomes Poster I
0546: Markers of Oxidative Stress in Systemic Lupus Erythematosus Patients with Nephritis
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- LL
Lu Liu, PhD (she/her/hers)
University Medical Center Groningen
Groningen, NetherlandsDisclosure information not submitted.
Abstract Poster Presenter(s)
Lu Liu, Karina de Leeuw, Suzanne Arends, Berber Doornbos-van der Meer, Harry van Goor and Johanna Westra, University Medical Center Groningen, Groningen, Netherlands
Background/Purpose: Lupus nephritis (LN) is regarded as one of the most severe manifestations of systemic lupus erythematosus (SLE). This inflammation in the kidneys may lead to excessive production of reactive oxygen species (ROS), which can induce oxidative stress, creating a pathogenic loop. Potential biomarkers of oxidative stress are plasma-free thiols, soluble receptors for advanced glycation end-products (sRAGE), and malondialdehyde (MDA). To analyze whether levels of thiols, sRAGE and MDA are different in SLE, and especially in active LN. Moreover, associations between oxidative stress biomarkers and clinical characteristics were investigated.
Methods: Forty-seven SLE patients with quiescent disease (Q-SLE) without renal involvement, 23 SLE patients with active proliferative LN, who previously participated in Dutch Lupus Nephritis studies and 23 healthy controls (HC) were included. Of the SLE patients with active LN follow-up samples were also analyzed. Thiols levels were measured as previously described. sRAGE levels were measured by ELISA. MDA levels were measured by Lipid Peroxidation (MDA) Assay Kit. Clinical parameters, including disease activity using the Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score, were documented. Longitudinal changes in thiols, sRAGE, and MDA levels were compared to clinical parameters using generalized estimating equations (GEE).
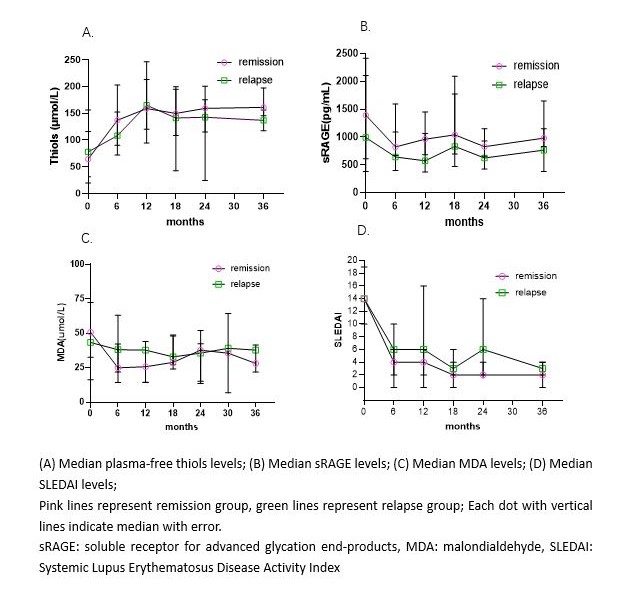
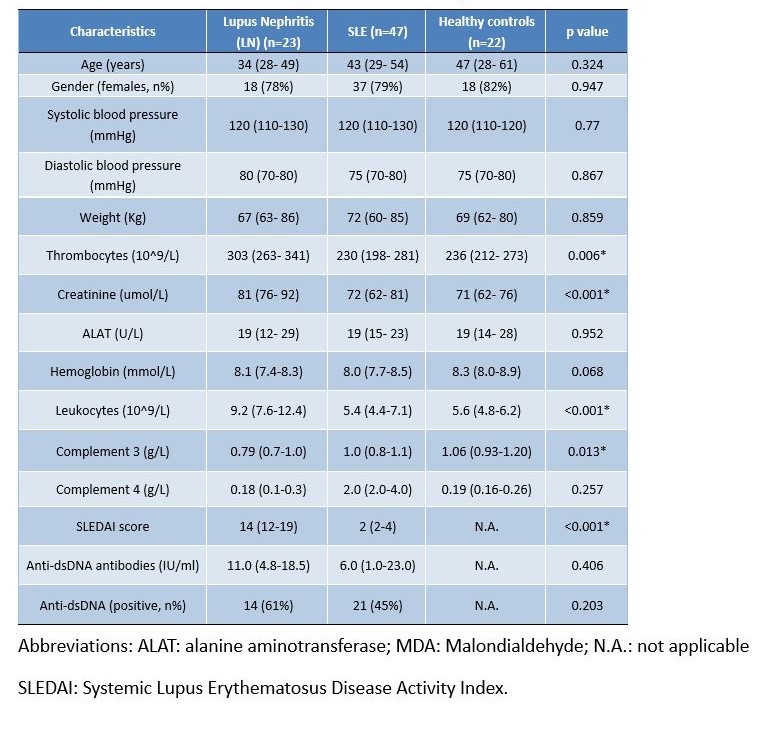
Results: Demographic characteristics are shown in Table 1. Thiols levels were significantly lower in active LN (at baseline) and Q-SLE patients compared to HC (Figure 1A). There was no significant difference in sRAGE levels among the groups (Figure 1B). Q-SLE patients exhibited significantly elevated levels of MDA compared to HC (Figure 1C). In SLE patients with LN, changes over time in thiols, sRAGE, MDA and SLEDAI during the 36-month follow-up are shown in Figure 2. We divided the patients into relapse and remission subgroups, defined as having remission when SLEDAI was < 5 during follow-up. Six patients experienced a flare-up resulting in a recurrence rate of 26%. In the univariate GEE model, changes of thiols were negatively correlated with SLEDAI (p < 0.001). Changes in sRAGE and MDA were positively correlated with SLEDAI (p =0.035 and p = 0.016, respectively).
Conclusion: Levels of thiols are significantly reduced in patients with Q-SLE and active LN compared to HC. In Q-SLE, levels of MDA were increased compared to HC. During follow-up of SLE patients with LN, thiols levels are significantly negatively correlated to SLEDAI. sRAGE and MDA levels are slightly positively correlated with SLEDAI. These results indicated that SLE patients with or without nephritis have increased oxidative stress levels compared with HC, associated with disease activity. Furthermore, free thiols might be a better biomarker of oxidative stress in LN compared to sRAGE and MDA.
.jpg)
L. Liu: None; K. de Leeuw: None; S. Arends: None; B. Doornbos-van der Meer: None; H. van Goor: None; J. Westra: None.
Background/Purpose: Lupus nephritis (LN) is regarded as one of the most severe manifestations of systemic lupus erythematosus (SLE). This inflammation in the kidneys may lead to excessive production of reactive oxygen species (ROS), which can induce oxidative stress, creating a pathogenic loop. Potential biomarkers of oxidative stress are plasma-free thiols, soluble receptors for advanced glycation end-products (sRAGE), and malondialdehyde (MDA). To analyze whether levels of thiols, sRAGE and MDA are different in SLE, and especially in active LN. Moreover, associations between oxidative stress biomarkers and clinical characteristics were investigated.
Methods: Forty-seven SLE patients with quiescent disease (Q-SLE) without renal involvement, 23 SLE patients with active proliferative LN, who previously participated in Dutch Lupus Nephritis studies and 23 healthy controls (HC) were included. Of the SLE patients with active LN follow-up samples were also analyzed. Thiols levels were measured as previously described. sRAGE levels were measured by ELISA. MDA levels were measured by Lipid Peroxidation (MDA) Assay Kit. Clinical parameters, including disease activity using the Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score, were documented. Longitudinal changes in thiols, sRAGE, and MDA levels were compared to clinical parameters using generalized estimating equations (GEE).
Results: Demographic characteristics are shown in Table 1. Thiols levels were significantly lower in active LN (at baseline) and Q-SLE patients compared to HC (Figure 1A). There was no significant difference in sRAGE levels among the groups (Figure 1B). Q-SLE patients exhibited significantly elevated levels of MDA compared to HC (Figure 1C). In SLE patients with LN, changes over time in thiols, sRAGE, MDA and SLEDAI during the 36-month follow-up are shown in Figure 2. We divided the patients into relapse and remission subgroups, defined as having remission when SLEDAI was < 5 during follow-up. Six patients experienced a flare-up resulting in a recurrence rate of 26%. In the univariate GEE model, changes of thiols were negatively correlated with SLEDAI (p < 0.001). Changes in sRAGE and MDA were positively correlated with SLEDAI (p =0.035 and p = 0.016, respectively).
Conclusion: Levels of thiols are significantly reduced in patients with Q-SLE and active LN compared to HC. In Q-SLE, levels of MDA were increased compared to HC. During follow-up of SLE patients with LN, thiols levels are significantly negatively correlated to SLEDAI. sRAGE and MDA levels are slightly positively correlated with SLEDAI. These results indicated that SLE patients with or without nephritis have increased oxidative stress levels compared with HC, associated with disease activity. Furthermore, free thiols might be a better biomarker of oxidative stress in LN compared to sRAGE and MDA.
.jpg)
Figure 1. Levels of thiols, sRAGE and MDA at baseline
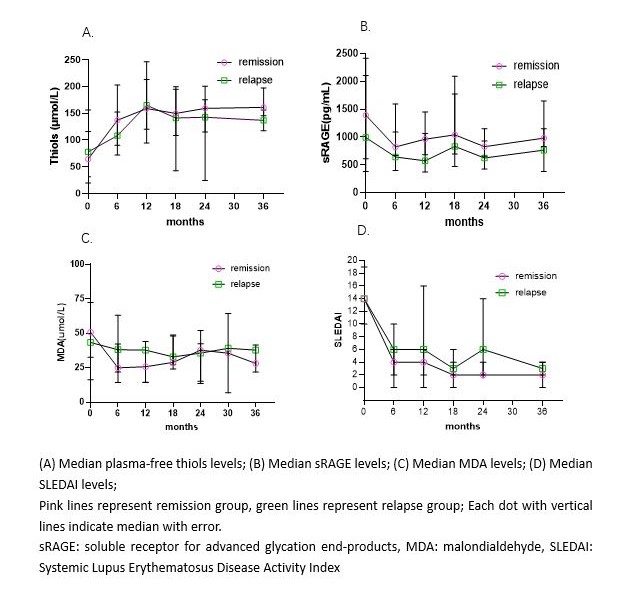
Figure 2. Median oxidative stress biomarkers and SLEDAI levels during 36-month follow-up of SLE patients with LN
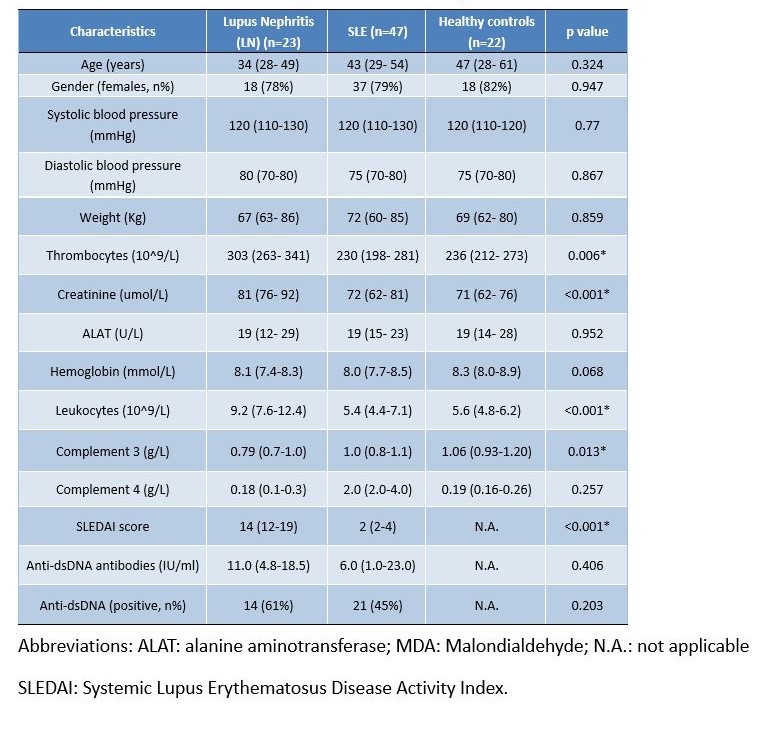
Table 1. Baseline characteristics of patients and healthy controls
L. Liu: None; K. de Leeuw: None; S. Arends: None; B. Doornbos-van der Meer: None; H. van Goor: None; J. Westra: None.



