Abstract Session
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: Abstracts: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science I (2461–2466)
2462: Mitochondrial-Mediated Neutrophil Activation in Dermatomyositis (DM) and Inclusion Body Myositis (IBM): Insights into Pathogenesis and Therapeutic Implications
Tuesday, November 14, 2023
2:15 PM - 2:25 PM PT
Location: Room 25A-C
- JG
Jorge Gonzalez Chapa, MD, PhD
University of Washington
Seattle, WA, United StatesDisclosure information not submitted.
Presenting Author(s)
Jorge Armando Gonzalez-Chapa1, Jemima Albayda2, Begum Horuluoglu3, Despina Michailidou1, Marina Barguil Macedo1, Lisa Christopher-Stine2, Ingrid Lundberg4 and Christian Lood1, 1University of Washington, Seattle, WA, 2Johns Hopkins University, Baltimore, MD, 3Karolinska Institutet, Stockholm, Sweden, 4Division of Rheumatology, Department of Medicine, Karolinska Institutet; Department of Gastroenterology, Dermatotology, Rhematology, Karolinska Universitetssjukhuset, Stockholm, Sweden
Background/Purpose: Dermatomyositis (DM) and inclusion body myositis (IBM) are characterized by muscle weakness and inflammation, with emerging evidence of mitochondrial and neutrophil involvement. Prior work from our group has demonstrated the important role of mitochondrial-derived danger-associated molecular patterns to promote neutrophil activation in inflammatory conditions. In the current study, we aimed to investigate whether patients with myopathies had elevated levels of extracellular mitochondrial biomarkers promoting neutrophil-mediated inflammation.
Methods: Plasma samples were obtained from patients with inclusion body myositis (IBM, n=46), dermatomyositis (DM, n=40), and healthy individuals (HC, n=40) from Karolinska Institutet, Stockholm, Sweden; Johns Hopkins, Baltimore, USA; and University of Washington, Seattle, USA. DM patients were further categorized based on the presence of autoantibodies towards MDA5 (n= 19) and TIF1-gamma (n=21). Plasma levels of neutrophil-derived calprotectin and neutrophil elastase (NE)-DNA complexes, as well as mitochondrial-derived GDF-15, and N-formyl methionine (fMET), which are valuable indicators of potential mitochondrial driven-pathological processes, cellular stress, and/or tissue damage, were measured using ELISA. Statistical analysis was performed using GraphPad Prism 9.4.0.
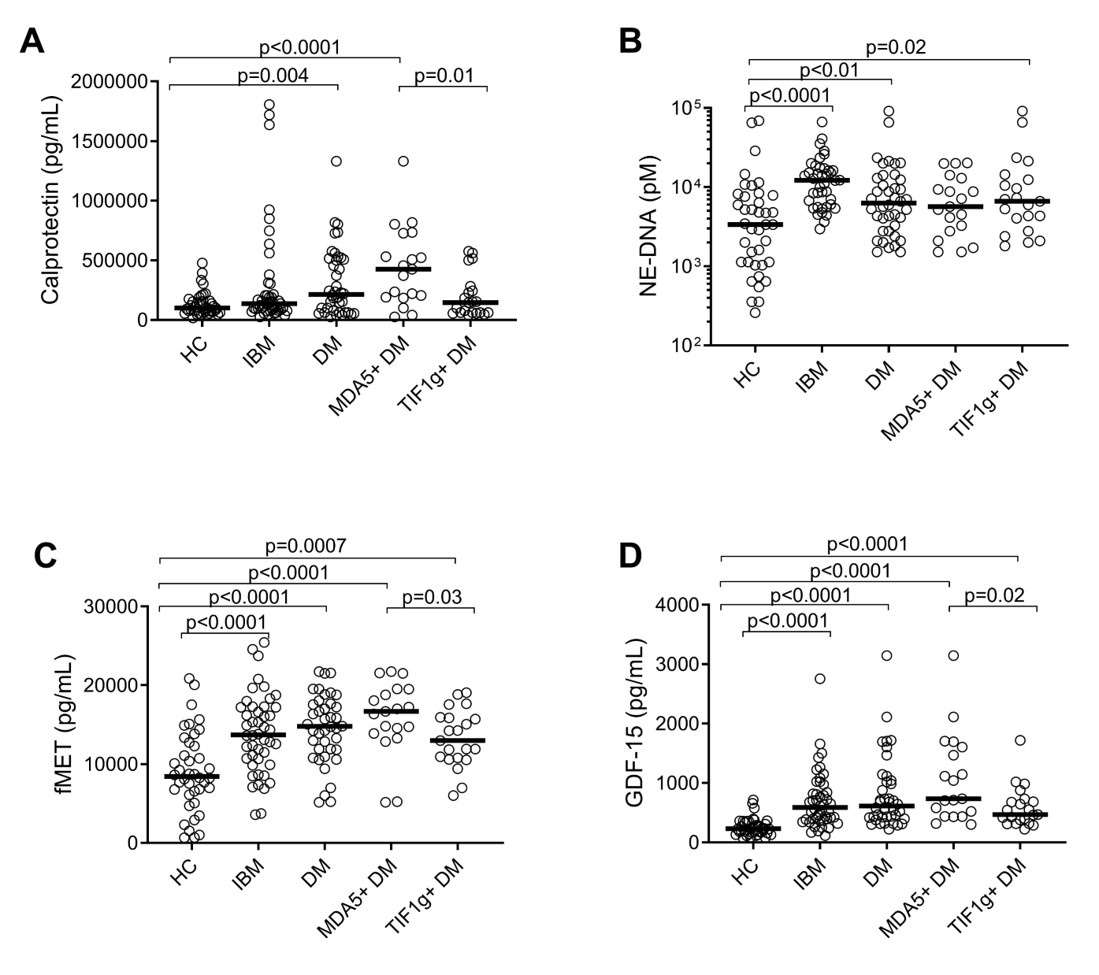
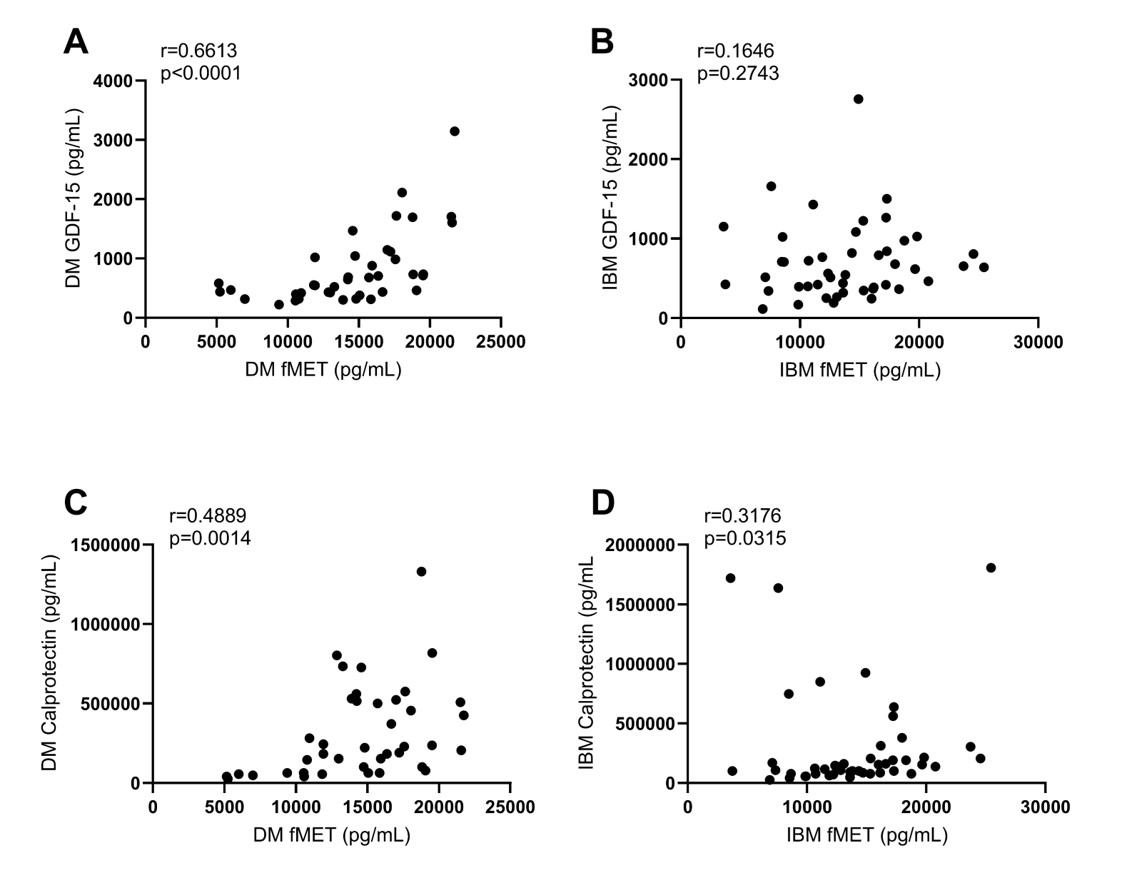
Results: Calprotectin levels were significantly elevated in DM patients, with the highest concentrations observed in those with MDA5 subtype (Figure 1A). Patients with IBM had similar levels of calprotectin as compared to HC. In contrast, levels of neutrophil extracellular traps, NETs (NE-DNA), were elevated in both DM and IBM patients, as compared to HC (Figure 1B). Both IBM and DM patients exhibited higher levels of mitochondrial-derived fMET and GDF-15 as compared to HC (Figures 1C and D), supporting a role for mitochondrial dysfunction and extrusion in these myopathies. Levels of GDF-15 and fMET were strongly correlated in DM but surprisingly no association was found in IBM (Figures 2A and B). Of note, consistent with other inflammatory conditions, levels of mitochondrial-derived fMET correlated strongly with neutrophil activation marker calprotectin in both IBM and DM (Figures 2C and D) suggesting that similar mechanisms, e.g. activation of neutrophils through fMET receptor FPR1, may operate in these subgroups of myopathies.
Conclusion: Our findings reveal distinct biomarker profiles in DM and IBM, highlighting the potential roles of mitochondria and neutrophils in myopathies. The differences and similarities observed between the subgroups suggest that calprotectin and NETs may play distinct roles in DM and IBM, while elevated levels of mitochondrial-derived fMET and GDF-15 indicate the potential involvement of mitochondrial dysfunction suggesting a common pathological mechanism. Further studies are warranted to determine the role of mitochondria and neutrophils in disease pathogenesis, as well as their clinical implications in monitoring disease activity.
J. Armando Gonzalez-Chapa: None; J. Albayda: Amgen, 5, Janssen, 5; B. Horuluoglu: None; D. Michailidou: Chemocentryx, 1; M. Barguil Macedo: None; L. Christopher-Stine: None; I. Lundberg: Argenx, 6, Astra-Zeneca, 5, Boehringer-Ingelheim, 6, Bristol-Myers Squibb(BMS), 1, Corbus Pharmaceutical, 6, EMD Serono Research & Development Institute, 6, Janssen, 6, Kezar, 6, Novartis, 11, Octapharma, 6, Orphazyme, 6, Pfizer, 1, Roche, 11, Xencor, 6; C. Lood: Amytryx, 5, Boehringer-Ingelheim, 5, Bristol-Myers Squibb(BMS), 5, Citryll, 2, Eli Lilly, 5, Gilead, 5, Horizon Therapeutics, 5, Pfizer, 5, Redd Pharma, 5, 11.
Background/Purpose: Dermatomyositis (DM) and inclusion body myositis (IBM) are characterized by muscle weakness and inflammation, with emerging evidence of mitochondrial and neutrophil involvement. Prior work from our group has demonstrated the important role of mitochondrial-derived danger-associated molecular patterns to promote neutrophil activation in inflammatory conditions. In the current study, we aimed to investigate whether patients with myopathies had elevated levels of extracellular mitochondrial biomarkers promoting neutrophil-mediated inflammation.
Methods: Plasma samples were obtained from patients with inclusion body myositis (IBM, n=46), dermatomyositis (DM, n=40), and healthy individuals (HC, n=40) from Karolinska Institutet, Stockholm, Sweden; Johns Hopkins, Baltimore, USA; and University of Washington, Seattle, USA. DM patients were further categorized based on the presence of autoantibodies towards MDA5 (n= 19) and TIF1-gamma (n=21). Plasma levels of neutrophil-derived calprotectin and neutrophil elastase (NE)-DNA complexes, as well as mitochondrial-derived GDF-15, and N-formyl methionine (fMET), which are valuable indicators of potential mitochondrial driven-pathological processes, cellular stress, and/or tissue damage, were measured using ELISA. Statistical analysis was performed using GraphPad Prism 9.4.0.
Results: Calprotectin levels were significantly elevated in DM patients, with the highest concentrations observed in those with MDA5 subtype (Figure 1A). Patients with IBM had similar levels of calprotectin as compared to HC. In contrast, levels of neutrophil extracellular traps, NETs (NE-DNA), were elevated in both DM and IBM patients, as compared to HC (Figure 1B). Both IBM and DM patients exhibited higher levels of mitochondrial-derived fMET and GDF-15 as compared to HC (Figures 1C and D), supporting a role for mitochondrial dysfunction and extrusion in these myopathies. Levels of GDF-15 and fMET were strongly correlated in DM but surprisingly no association was found in IBM (Figures 2A and B). Of note, consistent with other inflammatory conditions, levels of mitochondrial-derived fMET correlated strongly with neutrophil activation marker calprotectin in both IBM and DM (Figures 2C and D) suggesting that similar mechanisms, e.g. activation of neutrophils through fMET receptor FPR1, may operate in these subgroups of myopathies.
Conclusion: Our findings reveal distinct biomarker profiles in DM and IBM, highlighting the potential roles of mitochondria and neutrophils in myopathies. The differences and similarities observed between the subgroups suggest that calprotectin and NETs may play distinct roles in DM and IBM, while elevated levels of mitochondrial-derived fMET and GDF-15 indicate the potential involvement of mitochondrial dysfunction suggesting a common pathological mechanism. Further studies are warranted to determine the role of mitochondria and neutrophils in disease pathogenesis, as well as their clinical implications in monitoring disease activity.
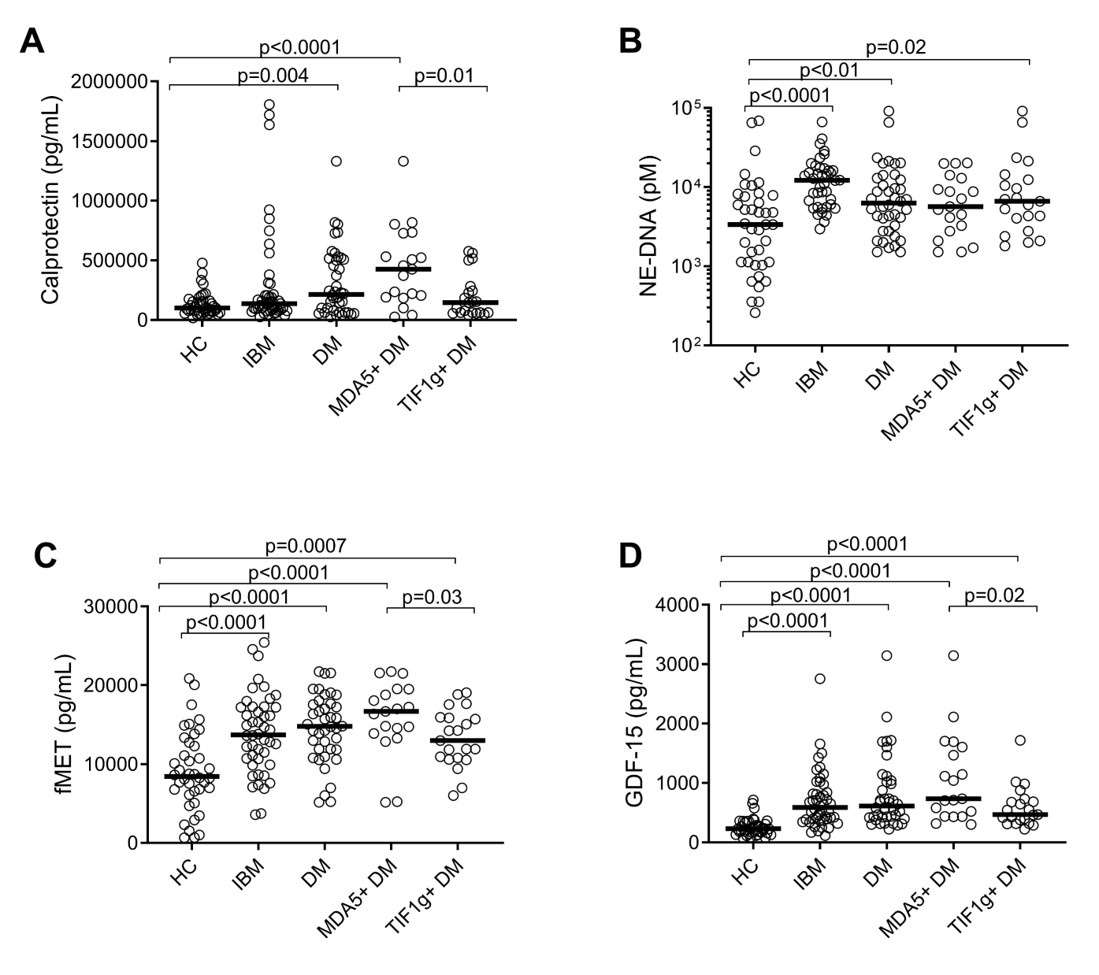
Figure 1. Neutrophil and mitochondrial biomarkers in IBM and DM.
Levels of A) Calprotectin, B) NE-DNA, C) fMET, and D) GDF-15 in patients with Inclusion Body Myositis (IBM), Dermatomyositis (DM), and Healthy Controls (HC). DM patients were subdivided into MDA5 (n=19) and TIF-1 gamma (n=21) subgroups. Mann-Whitney U test was used for statistical analyses.
Levels of A) Calprotectin, B) NE-DNA, C) fMET, and D) GDF-15 in patients with Inclusion Body Myositis (IBM), Dermatomyositis (DM), and Healthy Controls (HC). DM patients were subdivided into MDA5 (n=19) and TIF-1 gamma (n=21) subgroups. Mann-Whitney U test was used for statistical analyses.
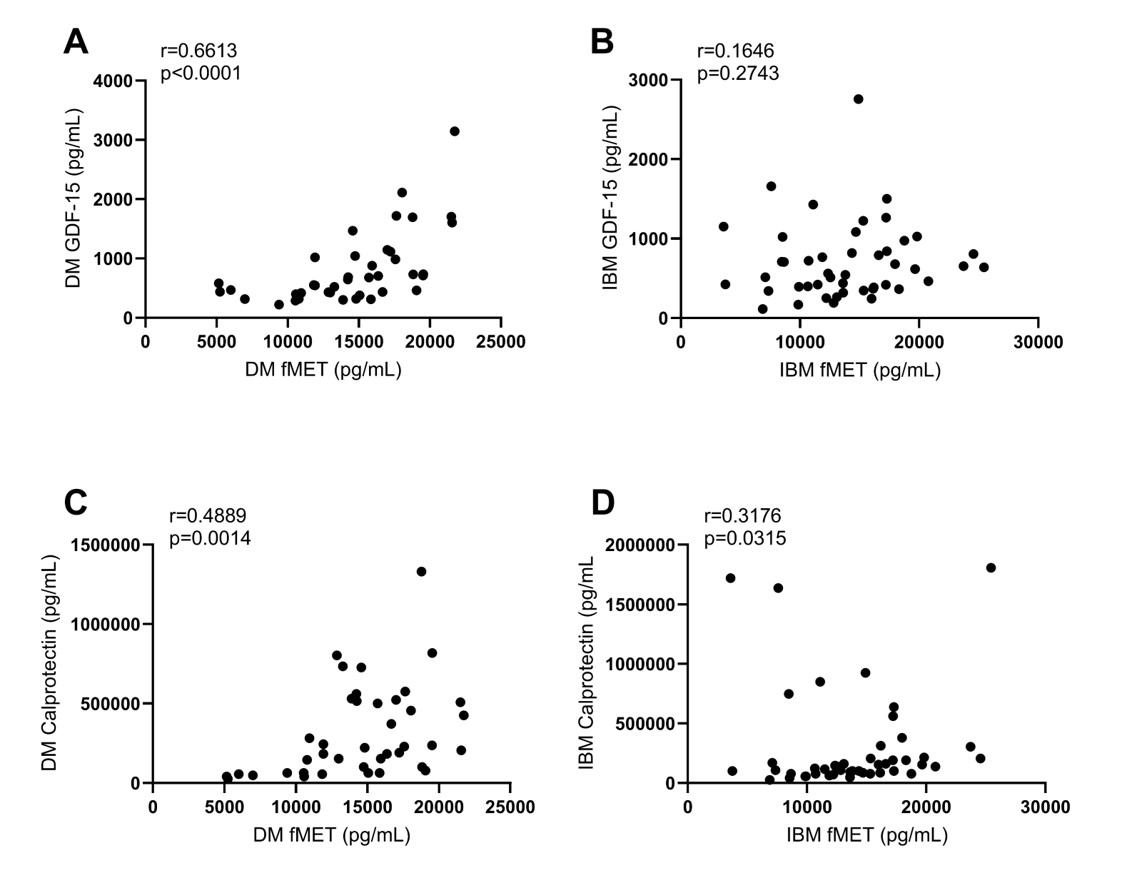
Figure 2. DM and IBM correlations between neutrophil and mitochondrial biomarkers
Correlations between GDF-15 and fMET in A) DM and B) IBM patients. Correlations between calprotectin and fMET in C) DM and D) IBM patients.
Spearman’s correlation coefficient test.
Correlations between GDF-15 and fMET in A) DM and B) IBM patients. Correlations between calprotectin and fMET in C) DM and D) IBM patients.
Spearman’s correlation coefficient test.
J. Armando Gonzalez-Chapa: None; J. Albayda: Amgen, 5, Janssen, 5; B. Horuluoglu: None; D. Michailidou: Chemocentryx, 1; M. Barguil Macedo: None; L. Christopher-Stine: None; I. Lundberg: Argenx, 6, Astra-Zeneca, 5, Boehringer-Ingelheim, 6, Bristol-Myers Squibb(BMS), 1, Corbus Pharmaceutical, 6, EMD Serono Research & Development Institute, 6, Janssen, 6, Kezar, 6, Novartis, 11, Octapharma, 6, Orphazyme, 6, Pfizer, 1, Roche, 11, Xencor, 6; C. Lood: Amytryx, 5, Boehringer-Ingelheim, 5, Bristol-Myers Squibb(BMS), 5, Citryll, 2, Eli Lilly, 5, Gilead, 5, Horizon Therapeutics, 5, Pfizer, 5, Redd Pharma, 5, 11.



