Abstract Session
Rheumatoid arthritis (RA)
Session: Abstracts: RA – Treatments II: RA Treatment Safety (1675–1680)
1680: What Trade-offs Are Acceptable to Rheumatoid Arthritis Patients During Treatment Selection?
Monday, November 13, 2023
5:15 PM - 5:25 PM PT
Location: Exhibit Hall A-B
.jpg)
Rieke Alten, MD, PhD
SCHLOSSPARK KLINIK, University Medicine Berlin
Berlin, GermanyDisclosure information not submitted.
Presenting Author(s)
Rieke Alten1, Juan carlos Nieto-Gonzalez2, Peggy Jacques3, Carlomaurizio Montecucco4, Robert Moots5, Helga Radner6, Sebastian Heidenreich7, Chiara Whichello7, Nicolas Krucien7, Monia Zignani8, Harald Vonkeman9 and Katrien Van Beneden10, 1Department of Internal Medicine and Rheumatology, Schlosspark Klinik, University Medicine Berlin, Berlin, Germany, 2Servicio de Reumatología, Hospital General Universitario Gregorio Marañón, Madrid, Spain, 3Department of Rheumatology and VIB Inflammation Research Center, University Hospital Ghent, Ghent, Belgium, 4Division of Rheumatology, University of Pavia and Fondazione IRCCS Policlinico San Matteo, Pavia, Italy, 5Department of Rheumatology, Aintree University Hospital, Liverpool, United Kingdom, 6Department of Internal Medicine III, Division of Rheumatology, Medical University Vienna, Vienna, Austria, 7Patient-centred Research, Evidera Inc., London, United Kingdom, 8Medical Affairs, Galapagos GmbH, Basel, Switzerland, 9Department of Rheumatology, Medisch Spectrum Twente and University of Twente, Enschede, Netherlands, 10Medical Safety, Galapagos NV, Mechelen, Belgium
Background/Purpose: Multiple RA therapies are available that differ in attributes such as mode of administration and benefit-risk profile. Challenging trade-offs are made during treatment selection to accommodate patients' circumstances and ensure comprehensive disease management. EULAR recommendations for RA management emphasize the need to recognize patient preferences in shared decision-making (SDM). This study elicited trade-offs that RA patients were willing to make during treatment selection, accounting for preference heterogeneity.
Methods: An online discrete choice experiment was conducted from Sep–Oct 2021; RA patients were required to elicit their preferences for RA treatment attributes (Figure) and make trade-offs between them. Attributes were chosen based on literature review and qualitative patient interviews; these were tested in a quantitative pilot. Main data collection was via an online survey which asked participants to choose between hypothetical treatments. Patients were ≥18 years old, diagnosed with RA, currently received systemic DMARD therapy for RA, and resident in France, Germany, Italy, Spain, United Kingdom, or United States. Male patients were oversampled to support subgroup analysis of preferences for effects on sperm parameters. Data were analyzed using a correlated mixed logit model; differences in preferences by sex and age were explored. Relative attribute importance (RAI) scores and maximum acceptable risk (MAR) measures were derived.
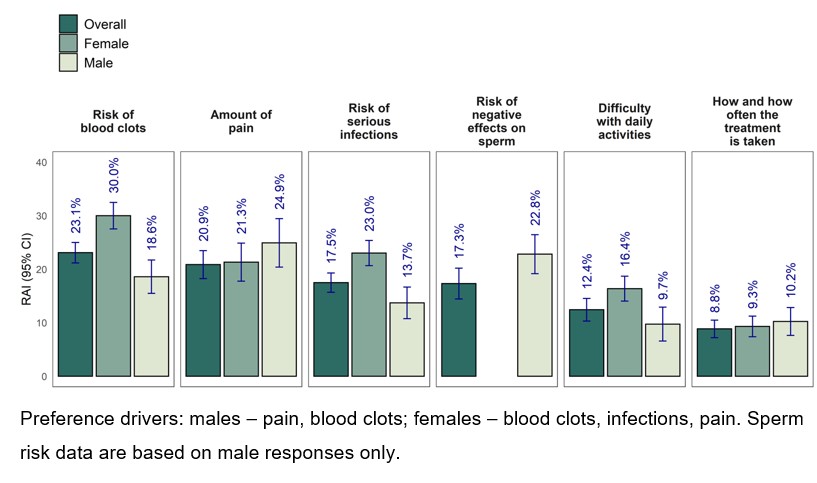
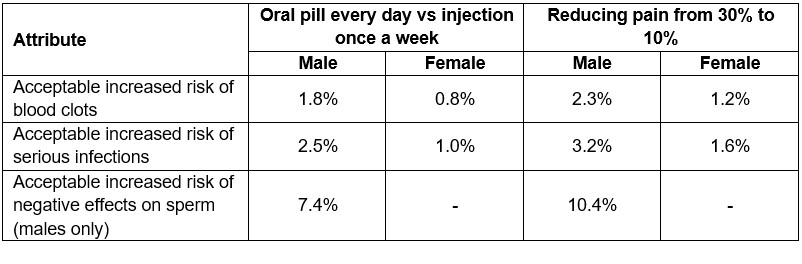
Results: In total, 2,090 patients participated; 42% were female with predefined oversampling of males; mean age was 45.2 years (range 18–83). Estimated effects were significant for all attributes (p< 0.001), implying that they all influenced treatment choice and that preferences differed between participants. RAI scores revealed different priorities between males and females (Figure). Reducing pain and negative effect on semen parameters was most important to males; females were most concerned by risk of blood clots and serious infections. Remaining attributes were of lower importance. No single attribute explained treatment preferences by more than 30%. Patients aged 18-44 years placed less importance on frequency and mode of treatment administration than older patients. Patients accepted extra risks of blood clots, serious infections, or negative effects on sperm for an oral pill every day vs injection once a week, and for reducing amount of pain from 30% to 10% (Table). Similar observations were made for improved performance of daily activities. Acceptable trade-offs varied between patients.
Conclusion: Preferences of RA patients were driven by benefits and risks of RA treatments, with no single attribute dominating the decision making. Patients were willing to accept higher risk of serious infections and blood clots in exchange for improvements in pain, daily activities, or administration convenience. These findings emphasize the importance of considering the entire treatment profile, including benefits, risks, and administration to support SDM between providers and patients.
R. Alten: AbbVie, 2, 6, Amgen, 2, 6, Biogen, 2, 6, BMS, 2, 6, Celltrion, 2, 6, Gilead, 2, 6, Janssen, 2, 6, Lilly, 2, 6, Medac, 2, 6, MSD, 2, 6, Mylan, 2, 6, Novartis, 2, 6, Pfizer, 2, 6, Roche, 2, 6, Sandoz, 2, 6, Sanofi-Genzyme, 2, 6, UCB, 2, 6, Viatris, 2, 6; J. Nieto-Gonzalez: AbbVie, 2, 6, Amgen, 2, 6, Biogen, 6, Bristol-Myers Squibb(BMS), 6, FAES Farma, 6, Galapagos, 2, GSK, 2, Janssen, 2, 6, Lilly, 6, MSD, 2, 6, Novartis, 6, Pfizer, 6, Roche, 6, Sanofi, 6, UCB, 6; P. Jacques: AbbVie, 12, Support for meeting attendance, Eli Lilly, 6, Galapagos, 12, Support for meeting attendance, Pfizer, 5, Roche, 5, UCB, 12, Support for meeting attendance; C. Montecucco: AbbVie, 2, 6, BMS, 2, 6, Boehringer Ingelheim, 6, Eli Lilly, 6, Galapagos, 6, Gilead, 2, Pfizer, 6, Roche, 6, Sanofi, 6; R. Moots: Amgen, 6, Ferring, 2, Galapagos, 6, Novartis, 5; H. Radner: Gilead, 6, Janssen, 6, MSD, 6, Pfizer Cooperation Austria, 6; S. Heidenreich: Evidera Inc., 3, 11; C. Whichello: Evidera Inc., 3; N. Krucien: Evidera Inc., 3, 11; M. Zignani: Galapagos, 3, 11; H. Vonkeman: AbbVie, 5, 6, Boehringer Ingelheim, 5, 6, Galapagos, 5, 6, Janssen, 5, 6, Novartis, 5, 6, Pfizer, 5, 6, UCB, 5, 6; K. Van Beneden: Galapagos, 3, 11.
Background/Purpose: Multiple RA therapies are available that differ in attributes such as mode of administration and benefit-risk profile. Challenging trade-offs are made during treatment selection to accommodate patients' circumstances and ensure comprehensive disease management. EULAR recommendations for RA management emphasize the need to recognize patient preferences in shared decision-making (SDM). This study elicited trade-offs that RA patients were willing to make during treatment selection, accounting for preference heterogeneity.
Methods: An online discrete choice experiment was conducted from Sep–Oct 2021; RA patients were required to elicit their preferences for RA treatment attributes (Figure) and make trade-offs between them. Attributes were chosen based on literature review and qualitative patient interviews; these were tested in a quantitative pilot. Main data collection was via an online survey which asked participants to choose between hypothetical treatments. Patients were ≥18 years old, diagnosed with RA, currently received systemic DMARD therapy for RA, and resident in France, Germany, Italy, Spain, United Kingdom, or United States. Male patients were oversampled to support subgroup analysis of preferences for effects on sperm parameters. Data were analyzed using a correlated mixed logit model; differences in preferences by sex and age were explored. Relative attribute importance (RAI) scores and maximum acceptable risk (MAR) measures were derived.
Results: In total, 2,090 patients participated; 42% were female with predefined oversampling of males; mean age was 45.2 years (range 18–83). Estimated effects were significant for all attributes (p< 0.001), implying that they all influenced treatment choice and that preferences differed between participants. RAI scores revealed different priorities between males and females (Figure). Reducing pain and negative effect on semen parameters was most important to males; females were most concerned by risk of blood clots and serious infections. Remaining attributes were of lower importance. No single attribute explained treatment preferences by more than 30%. Patients aged 18-44 years placed less importance on frequency and mode of treatment administration than older patients. Patients accepted extra risks of blood clots, serious infections, or negative effects on sperm for an oral pill every day vs injection once a week, and for reducing amount of pain from 30% to 10% (Table). Similar observations were made for improved performance of daily activities. Acceptable trade-offs varied between patients.
Conclusion: Preferences of RA patients were driven by benefits and risks of RA treatments, with no single attribute dominating the decision making. Patients were willing to accept higher risk of serious infections and blood clots in exchange for improvements in pain, daily activities, or administration convenience. These findings emphasize the importance of considering the entire treatment profile, including benefits, risks, and administration to support SDM between providers and patients.
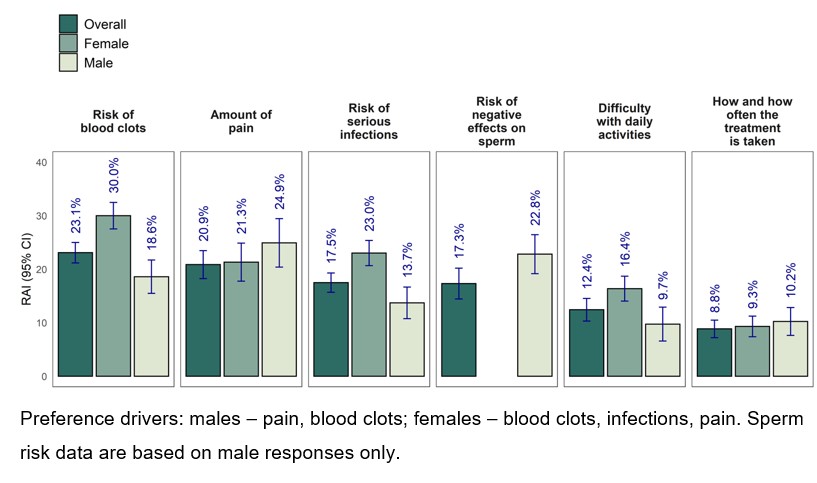
Figure. RAI overall and by sex
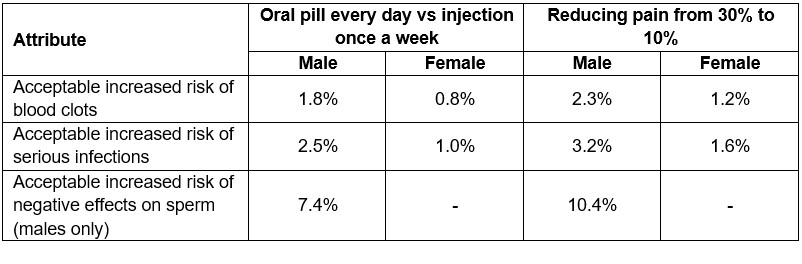
Table. Benefit-risk trade-offs: willingness to accept extra risk
R. Alten: AbbVie, 2, 6, Amgen, 2, 6, Biogen, 2, 6, BMS, 2, 6, Celltrion, 2, 6, Gilead, 2, 6, Janssen, 2, 6, Lilly, 2, 6, Medac, 2, 6, MSD, 2, 6, Mylan, 2, 6, Novartis, 2, 6, Pfizer, 2, 6, Roche, 2, 6, Sandoz, 2, 6, Sanofi-Genzyme, 2, 6, UCB, 2, 6, Viatris, 2, 6; J. Nieto-Gonzalez: AbbVie, 2, 6, Amgen, 2, 6, Biogen, 6, Bristol-Myers Squibb(BMS), 6, FAES Farma, 6, Galapagos, 2, GSK, 2, Janssen, 2, 6, Lilly, 6, MSD, 2, 6, Novartis, 6, Pfizer, 6, Roche, 6, Sanofi, 6, UCB, 6; P. Jacques: AbbVie, 12, Support for meeting attendance, Eli Lilly, 6, Galapagos, 12, Support for meeting attendance, Pfizer, 5, Roche, 5, UCB, 12, Support for meeting attendance; C. Montecucco: AbbVie, 2, 6, BMS, 2, 6, Boehringer Ingelheim, 6, Eli Lilly, 6, Galapagos, 6, Gilead, 2, Pfizer, 6, Roche, 6, Sanofi, 6; R. Moots: Amgen, 6, Ferring, 2, Galapagos, 6, Novartis, 5; H. Radner: Gilead, 6, Janssen, 6, MSD, 6, Pfizer Cooperation Austria, 6; S. Heidenreich: Evidera Inc., 3, 11; C. Whichello: Evidera Inc., 3; N. Krucien: Evidera Inc., 3, 11; M. Zignani: Galapagos, 3, 11; H. Vonkeman: AbbVie, 5, 6, Boehringer Ingelheim, 5, 6, Galapagos, 5, 6, Janssen, 5, 6, Novartis, 5, 6, Pfizer, 5, 6, UCB, 5, 6; K. Van Beneden: Galapagos, 3, 11.




