Abstract Session
Infection-related rheumatic syndromes
Session: Abstracts: Infection-related Rheumatic Disease (1669–1674)
1669: High Incidence of Immune-mediated Inflammatory Diseases in Sepsis Survivors: A Nationwide Exposed-non-exposed Epidemiological Study
Monday, November 13, 2023
4:00 PM - 4:10 PM PT
Location: Room 6E/6D
- AM
Presenting Author(s)
Arthur Mageau1, Alois Helary2, Stephane Ruckly3, Andrey Strukov2, Thomas Papo1, Jean-Francois Timsit1 and Karim Sacre1, 1Université Paris Cité, Paris, France, 2Assistance Publique Hopitaux de Paris, Paris, France, 3INSERM, Paris, France
Background/Purpose: Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection. Previous studies have shown that immune dysregulation associated with severe infection persists after discharge in two-thirds of surviving patients and is associated with worse long-term outcome. Hypothesizing that persistent immune dysregulation associated with sepsis may be involved in immune-mediated inflammatory diseases (IMIDs), we used a nationwide database to analyze the incidence of IMIDs after sepsis. We aim to analyze the incidence of IMIDs in patients who survived sepsis.
Methods: Comprehensive data on all exposed and non-exposed patients admitted to all French hospitals from January 2011 to November 2020 were collected from the national medical-administrative database, the PMSI (Programme de Médicalisation des Systèmes d'Information, Information system medicalization program). The PMSI provides a summary of diagnoses, procedures, and individual medical conditions at discharge from all French healthcare facilities. All data on adult patients admitted for sepsis between January to November 2020, in any of the French healthcare facilities were retrieved from the database. Exposure was sepsis requiring hospitalization. Sepsis was defined by the combination of at least one code of infection and one code referring to an organ failure diagnosis or procedure. Patients with a first sepsis (i.e. exposed) diagnosed in a French hospital in 2020 were randomly matched (ratio 1/1) with patients admitted during the same period for acute myocardial infarction (i.e. non-exposed). An exact matching procedure taking age ±2 years, gender, and comorbidities as matching variables was performed. The main outcome was a diagnosis of IMID based on specific ICD-10 codes during a 9-month follow up. Only patients with i) a first diagnosis of sepsis (exposed) or AMI (non-exposed) in 2020 and ii) no history of IMIDs reported in PMSI between January 1, 2010 and the index stay were included.
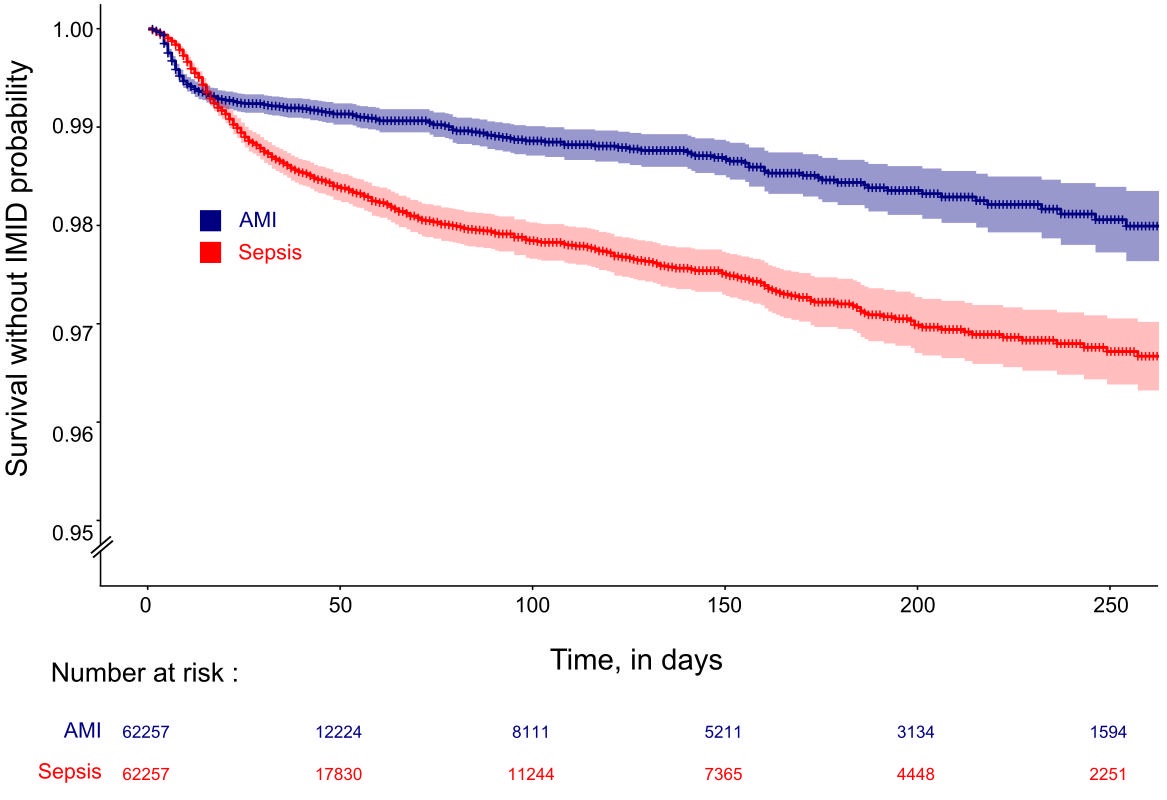
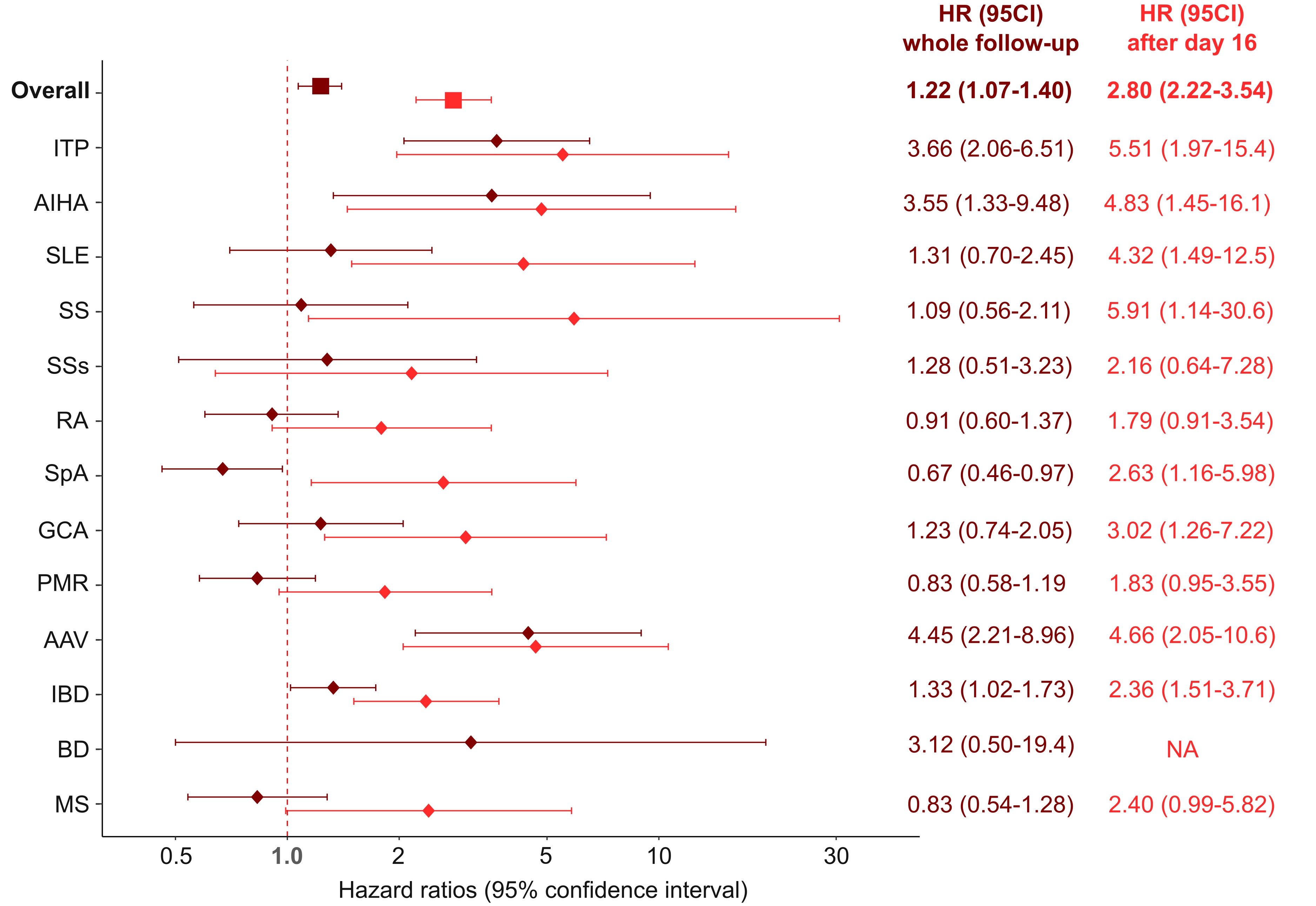
Results: In France, the incidence rate of IMIDs after a sepsis in 2020 - analyzed in 62,257 patients – was of 7,956 [95CI 7,392-8,520] per 100,000 patient-years. As compared to the non-exposed admitted population (Table 1), the IMID-free survival analysis showed an increased risk for IMIDs of 2.80 (HR; 95%CI [2.22-3.54]) starting from day 16 after admission (Figure 1). Risk of IMIDs following severe infection differed according to the nature of the autoimmune disease and were higher for immune thrombocytopenia (5.51 [1.97-15.4]), autoimmune hemolytic anemia (4.83 [1.45-16.1]) and ANCA associated vasculitis (4.66 [2.05-10.6]) (Figure 2).
Conclusion: Our study shows an intriguing and extremely high incidence of IMIDs among survivors of severe infections.
.jpg)
A. Mageau: None; A. Helary: None; S. Ruckly: None; A. Strukov: None; T. Papo: None; J. Timsit: None; K. Sacre: None.
Background/Purpose: Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection. Previous studies have shown that immune dysregulation associated with severe infection persists after discharge in two-thirds of surviving patients and is associated with worse long-term outcome. Hypothesizing that persistent immune dysregulation associated with sepsis may be involved in immune-mediated inflammatory diseases (IMIDs), we used a nationwide database to analyze the incidence of IMIDs after sepsis. We aim to analyze the incidence of IMIDs in patients who survived sepsis.
Methods: Comprehensive data on all exposed and non-exposed patients admitted to all French hospitals from January 2011 to November 2020 were collected from the national medical-administrative database, the PMSI (Programme de Médicalisation des Systèmes d'Information, Information system medicalization program). The PMSI provides a summary of diagnoses, procedures, and individual medical conditions at discharge from all French healthcare facilities. All data on adult patients admitted for sepsis between January to November 2020, in any of the French healthcare facilities were retrieved from the database. Exposure was sepsis requiring hospitalization. Sepsis was defined by the combination of at least one code of infection and one code referring to an organ failure diagnosis or procedure. Patients with a first sepsis (i.e. exposed) diagnosed in a French hospital in 2020 were randomly matched (ratio 1/1) with patients admitted during the same period for acute myocardial infarction (i.e. non-exposed). An exact matching procedure taking age ±2 years, gender, and comorbidities as matching variables was performed. The main outcome was a diagnosis of IMID based on specific ICD-10 codes during a 9-month follow up. Only patients with i) a first diagnosis of sepsis (exposed) or AMI (non-exposed) in 2020 and ii) no history of IMIDs reported in PMSI between January 1, 2010 and the index stay were included.
Results: In France, the incidence rate of IMIDs after a sepsis in 2020 - analyzed in 62,257 patients – was of 7,956 [95CI 7,392-8,520] per 100,000 patient-years. As compared to the non-exposed admitted population (Table 1), the IMID-free survival analysis showed an increased risk for IMIDs of 2.80 (HR; 95%CI [2.22-3.54]) starting from day 16 after admission (Figure 1). Risk of IMIDs following severe infection differed according to the nature of the autoimmune disease and were higher for immune thrombocytopenia (5.51 [1.97-15.4]), autoimmune hemolytic anemia (4.83 [1.45-16.1]) and ANCA associated vasculitis (4.66 [2.05-10.6]) (Figure 2).
Conclusion: Our study shows an intriguing and extremely high incidence of IMIDs among survivors of severe infections.
.jpg)
Table 1 Characteristics of the matched populations
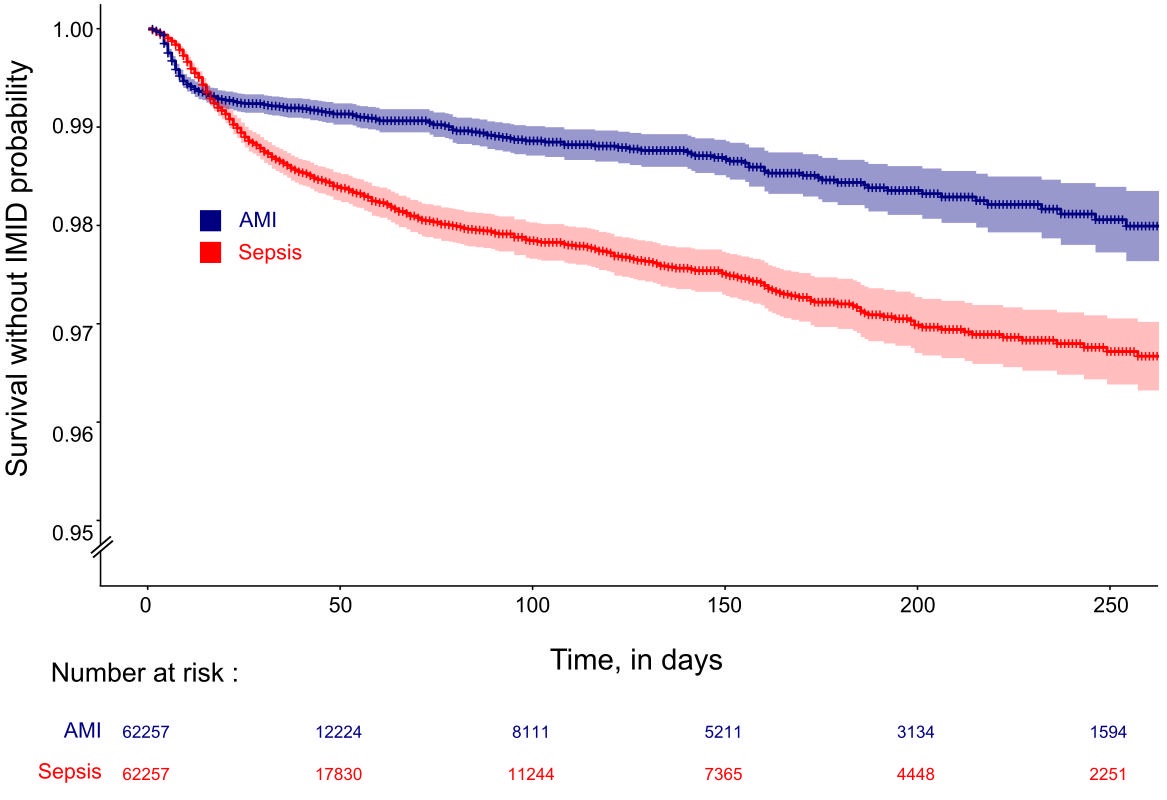
Figure 1 Survival without IMIDs among matched populations
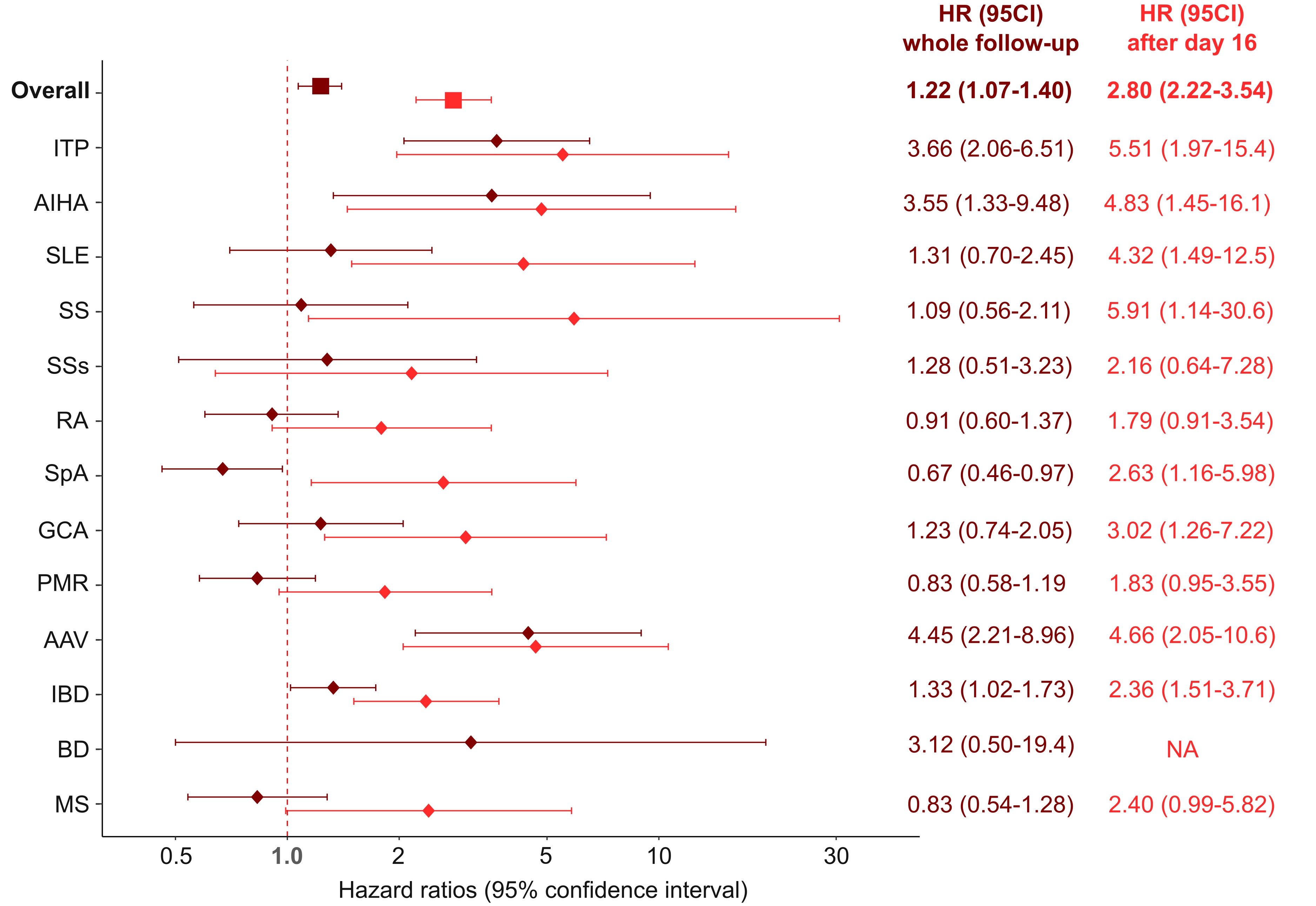
Figure 2 Risk for IMIDs onset after sepsis
IMIDs, immune-mediated inflammatory diseases; ITP, immune thrombocytopenia; AIHA, autoimmune hemolytic anemia; SLE, systemic lupus erythematosus; SS, Sjögren’s syndrome; SSs, systemic sclerosis; RA, rheumatoid arthritis; GCA, giant cell arteritis; PMR, polymyalgia rheumatica; AAV, ANCA-associated vasculitis; ANCA, anti-neutrophil cytoplasmic antibody; IBD, inflammatory bowel disease; UC, ulcerative colitis; MS, multiple sclerosis.
IMIDs, immune-mediated inflammatory diseases; ITP, immune thrombocytopenia; AIHA, autoimmune hemolytic anemia; SLE, systemic lupus erythematosus; SS, Sjögren’s syndrome; SSs, systemic sclerosis; RA, rheumatoid arthritis; GCA, giant cell arteritis; PMR, polymyalgia rheumatica; AAV, ANCA-associated vasculitis; ANCA, anti-neutrophil cytoplasmic antibody; IBD, inflammatory bowel disease; UC, ulcerative colitis; MS, multiple sclerosis.
A. Mageau: None; A. Helary: None; S. Ruckly: None; A. Strukov: None; T. Papo: None; J. Timsit: None; K. Sacre: None.



