Abstract Session
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: Abstracts: Spondyloarthritis Including Psoriatic Arthritis – Diagnosis, Manifestations, & Outcomes I: AxSpA (0841–0846)
0844: Facet Joint Inflammation Is Rare, but When Present It Is Associated with Facet Joint Ankylosis in Radiographic Axial Spondyloarthritis Patients from the SIAS Cohort
Sunday, November 12, 2023
4:45 PM - 4:55 PM PT
Location: Ballroom 20A
- Md
Manouk de Hooge, PhD
Ghent University Hospital
Hesperange, LuxembourgDisclosure information not submitted.
Presenting Author(s)
Manouk de Hooge1, Rosalinde Stal2, Alexandre Sepriano3, Xenofon Baraliakos4, Monique Reijnierse5, Juergen Braun6, Désirée van der Heijde7, Floris Van Gaalen2 and Sofia Ramiro7, 1Ghent University Hospital, Hesperange, Luxembourg, 2Leiden University Medical Center, Department of Rheumatology, Leiden, Netherlands, 3Leiden University Medical Centre, Portela Loures, Portugal, 4Rheumazentrum Ruhrgebiet Herne, Ruhr-University Bochum, Herne, Germany, 5Leiden University Medical Center, Leiden, Netherlands, 6Ruhr-Universität Bochum and Rheumazentrum Ruhrgebiet, Herne, Germany, 7Department of Rheumatology, Leiden University Medical Center, Leiden, Netherlands
Background/Purpose: To assess whether posterior element (PE) inflammation, in particular in the facet joints (FJ), is associated with new facet joint ankylosis on MRI one year later, in patients with radiographic axial spondyloarthritis (r-axSpA).
Methods: Patients with an r-axSpA diagnosis recruited from Germany (Herne) and the Netherlands (Leiden) were included in the Sensitive Imaging in Ankylosing Spondylitis (SIAS) observational cohort when all following criteria were met: 1) presenting with ≥1 inflammatory lesion on MRI-spine according to SPondyloArthritis Research Consortium of Canada score, 2) presenting with 1-18 syndesmophytes (assessed with modified Stoke Ankylosing Spondylitis Spinal Score), and 3) fulfilling the modified New York criteria. Spinal MRIs were performed at baseline, after 1 year and after 2 years. PE inflammatory lesions and facet joint ankylosis were assessed on MRI, per vertebral unit level (VU) by 3 readers independently. FJ inflammation in the cervical spine was not assessed. With conditional probability tables the probability of developing facet joint ankylosis after one year was described. Multilevel time-lagged auto-regressive GEE was used for the association between PE (or FJ) inflammation and the development of facet joint ankylosis one year later, taking the reader and VU levels into account.
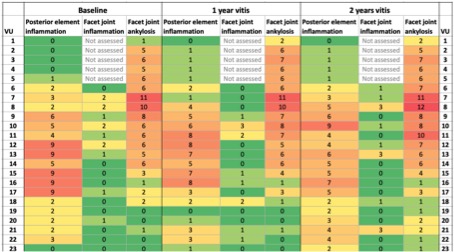
Results: In 58 patients MRI data of at least 2 readers was available. Their average age was 49±10 years and 85% was male. Inflammation in the PE or FJ at baseline was seen in 34 (58.6%) and 14 (24.1%) patients respectively. PE inflammation was distributed throughout the whole spine but emphatically more prevalent in the lower part of the thoracic spine (8.6%-15.5%). FJ inflammation was infrequently present, it was more often reported in the higher thoracic segment of the spine (1.7%-5.2%) (heatmap). Facet joint ankylosis was reported in 15 patients (25.9%) at baseline and in 17 patients (29.3%) with follow up visits. Facet joint ankylosis was mainly present in the upper half of the spine (heatmap). In 19 patients (32.8%) the development of new facet joint ankylosis over 1 or 2 years was seen by at least 1 reader.
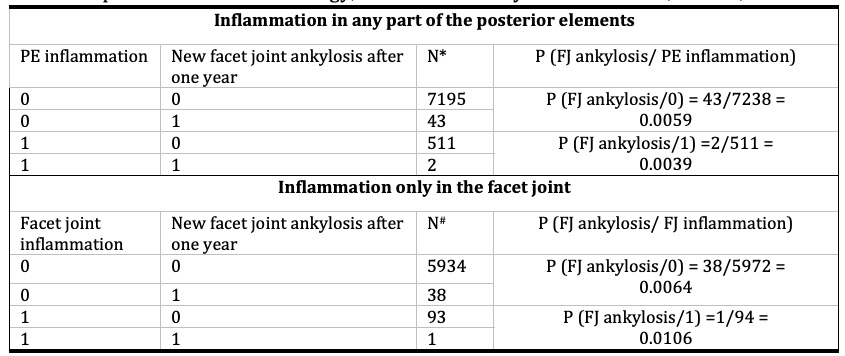
Of the VU levels with PE or FJ inflammation only very few showed new facet joint ankylosis after one year; 2 and 1 VU levels, respectively (table). There was no association between PE inflammation and the development of new facet joint ankylosis in the same level after one year (OR=1.15, 95%CI 0.55-2.42). However, FJ inflammation was associated with the development new facet joint ankylosis one year later (OR=3.79, 95%CI 1.47-9.75).
Conclusion: PE inflammation and facet joint ankylosis on MRI were uncommonly present in r-axSpA patients. No association was found between inflammation in the PE and the development of facet joint ankylosis. However, when inflammation in the FJ is present the likelihood of developing facet joint ankylosis after 1 year is over 3 times higher compared to FJ without inflammation. This finding adds to the pathophysiological relationship between inflammation and damage at the same anatomical location.
M. de Hooge: UCB, 6; R. Stal: None; A. Sepriano: None; X. Baraliakos: AbbVie, 2, 6, BMS, 2, 6, Chugai, 2, 6, Eli Lilly, 2, 6, Galapagos, 2, 6, Gilead, 2, 6, MSD, 2, 6, Novartis, 2, 6, Pfizer Inc, 2, 6, UCB, 2, 6; M. Reijnierse: None; J. Braun: None; D. van der Heijde: AbbVie, 2, Bayer, 2, BMS, 2, Eli Lilly, 2, Galapagos, 2, Gilead, 2, GSK, 2, Imaging Rheumatology BV, 12, Director, Janssen, 2, Novartis, 2, Pfizer, 2, Takeda, 2, UCB Pharma, 2; F. Van Gaalen: AbbVie, 12, Personal fees, BMS, 12, Personal fees, Eli Lilly, 12, Personal fees, Jacobus Stichting, 5, MSD, 12, Personal fees, Novartis, 5, 12, Fees, Stichting ASAS, 5, Stichting Vrienden van Sole Mio, 5, UCB Pharma, 5; S. Ramiro: AbbVie, 2, 5, Eli Lilly, 2, Galapagos, 5, MSD, 2, 5, Novartis, 2, 5, Pfizer, 2, 5, Sanofi, 2, UCB Pharma, 2, 5.
Background/Purpose: To assess whether posterior element (PE) inflammation, in particular in the facet joints (FJ), is associated with new facet joint ankylosis on MRI one year later, in patients with radiographic axial spondyloarthritis (r-axSpA).
Methods: Patients with an r-axSpA diagnosis recruited from Germany (Herne) and the Netherlands (Leiden) were included in the Sensitive Imaging in Ankylosing Spondylitis (SIAS) observational cohort when all following criteria were met: 1) presenting with ≥1 inflammatory lesion on MRI-spine according to SPondyloArthritis Research Consortium of Canada score, 2) presenting with 1-18 syndesmophytes (assessed with modified Stoke Ankylosing Spondylitis Spinal Score), and 3) fulfilling the modified New York criteria. Spinal MRIs were performed at baseline, after 1 year and after 2 years. PE inflammatory lesions and facet joint ankylosis were assessed on MRI, per vertebral unit level (VU) by 3 readers independently. FJ inflammation in the cervical spine was not assessed. With conditional probability tables the probability of developing facet joint ankylosis after one year was described. Multilevel time-lagged auto-regressive GEE was used for the association between PE (or FJ) inflammation and the development of facet joint ankylosis one year later, taking the reader and VU levels into account.
Results: In 58 patients MRI data of at least 2 readers was available. Their average age was 49±10 years and 85% was male. Inflammation in the PE or FJ at baseline was seen in 34 (58.6%) and 14 (24.1%) patients respectively. PE inflammation was distributed throughout the whole spine but emphatically more prevalent in the lower part of the thoracic spine (8.6%-15.5%). FJ inflammation was infrequently present, it was more often reported in the higher thoracic segment of the spine (1.7%-5.2%) (heatmap). Facet joint ankylosis was reported in 15 patients (25.9%) at baseline and in 17 patients (29.3%) with follow up visits. Facet joint ankylosis was mainly present in the upper half of the spine (heatmap). In 19 patients (32.8%) the development of new facet joint ankylosis over 1 or 2 years was seen by at least 1 reader.
Of the VU levels with PE or FJ inflammation only very few showed new facet joint ankylosis after one year; 2 and 1 VU levels, respectively (table). There was no association between PE inflammation and the development of new facet joint ankylosis in the same level after one year (OR=1.15, 95%CI 0.55-2.42). However, FJ inflammation was associated with the development new facet joint ankylosis one year later (OR=3.79, 95%CI 1.47-9.75).
Conclusion: PE inflammation and facet joint ankylosis on MRI were uncommonly present in r-axSpA patients. No association was found between inflammation in the PE and the development of facet joint ankylosis. However, when inflammation in the FJ is present the likelihood of developing facet joint ankylosis after 1 year is over 3 times higher compared to FJ without inflammation. This finding adds to the pathophysiological relationship between inflammation and damage at the same anatomical location.
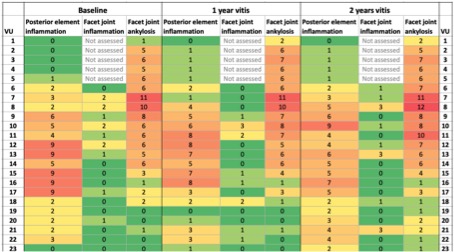
The extent of posterior element lesions on MRI across the 23 vertebral units (VU) in radiographic axial spondyloarthritis patients with 2 years follow-up.
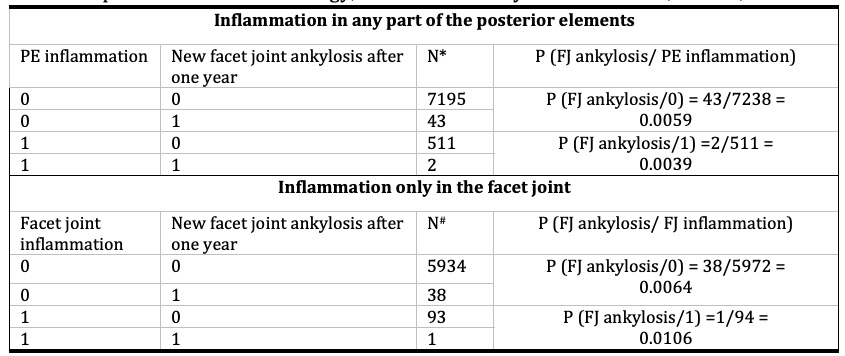
Table. Probability of developing facet joint ankylosis with and without posterior element inflammation present one year before, in r-axSpA patients from the SIAS cohort. PE; posterior elements, *; number of VU levels with inflammation in at least 1 part of the posterior elements (pedicle, facet joint, processes spinosi, soft tissue), #; number of facet joints, FJ; facet joint, P; probability
M. de Hooge: UCB, 6; R. Stal: None; A. Sepriano: None; X. Baraliakos: AbbVie, 2, 6, BMS, 2, 6, Chugai, 2, 6, Eli Lilly, 2, 6, Galapagos, 2, 6, Gilead, 2, 6, MSD, 2, 6, Novartis, 2, 6, Pfizer Inc, 2, 6, UCB, 2, 6; M. Reijnierse: None; J. Braun: None; D. van der Heijde: AbbVie, 2, Bayer, 2, BMS, 2, Eli Lilly, 2, Galapagos, 2, Gilead, 2, GSK, 2, Imaging Rheumatology BV, 12, Director, Janssen, 2, Novartis, 2, Pfizer, 2, Takeda, 2, UCB Pharma, 2; F. Van Gaalen: AbbVie, 12, Personal fees, BMS, 12, Personal fees, Eli Lilly, 12, Personal fees, Jacobus Stichting, 5, MSD, 12, Personal fees, Novartis, 5, 12, Fees, Stichting ASAS, 5, Stichting Vrienden van Sole Mio, 5, UCB Pharma, 5; S. Ramiro: AbbVie, 2, 5, Eli Lilly, 2, Galapagos, 5, MSD, 2, 5, Novartis, 2, 5, Pfizer, 2, 5, Sanofi, 2, UCB Pharma, 2, 5.



