Abstract Session
Imaging
Session: Abstracts: Imaging of Rheumatic Diseases (0745–0750)
0747: Clinical Phenotype of Patients with Subclinical Giant Cell Arteritis in Polymyalgia Rheumatica
Sunday, November 12, 2023
2:30 PM - 2:40 PM PT
Location: Room 24A-C
- SC
Sharon Cowley, MRCP, MBBCH
Tallaght University Hospital, Dublin
Dublin, Dublin, IrelandDisclosure information not submitted.
Presenting Author(s)
Sharon Cowley1, Colm Kirby2, Patricia Harkins3, Richard Conway4 and David Kane5, 1Tallaght University Hospital, Dublin, Dublin, Ireland, 2Tallaght University Hospital, Dublin, Ireland, 3St James's Hospital, Dublin, Ireland, 4Trinity College Dublin, Dublin, Ireland, 5Tallaght University Hospital & Trinity College Dublin, Dublin, Ireland
Background/Purpose: It has been reported that more than a quarter of patients with polymyalgia rheumatica (PMR) have subclinical giant cell arteritis (GCA). It remains unclear if all PMR patients should have ultrasound assessment for subclinical GCA or if there are certain phenotypes of patients that are more at risk of having subclinical GCA.
Methods: Newly diagnosed PMR patients who met a clinical diagnosis for PMR, verified by two rheumatologists were examined with vascular ultrasound (US) of their temporal and axillary arteries. US of all 6 branches of the superficial temporal and both axillary arteries was performed using a GE P9 device. Sonographic abnormalities considered indicative of vasculitis in the temporal arteries included the halo sign and non-compressible arteries with a thickened intima-media complex. An intima-media thickness of 0.42mm for the common superficial temporal branch, 0.34mm for the frontal branch, and 0.29mm for the parietal branch was considered positive. In the axillary arteries, a halo sign, and an intima-media thickness of >1.0mm was considered positive. Clinical and laboratory characteristics were recorded. Halo scores were calculated for positive cases. Ultrasound findings were compared to a cohort of GCA patients.
Results: 91 patients with newly diagnosed PMR and 57 patients with newly diagnosed GCA were included. ACR/EULAR classification criteria were met in 67 of those with PMR (primarily due to prior corticosteroid use in primary care resulting in normal ESR/CRP) and all of those with GCA. Of the 91 patients with PMR, 16 were identified as having subclinical GCA on ultrasound (17.5%).
The mean age at time of diagnosis was 69 years for those with PMR, 70 years for those with subclinical GCA in PMR and 74 years for those with GCA. Males were more likely to have subclinical GCA in PMR, accounting for 12 (75%) of the subclinical GCA group compared to 27 (36%) of the pure PMR group (p=0.045). The mean ESR at baseline for those with subclinical GCA in PMR was higher than those with isolated PMR; 49mm/hr compared to 38mm/hr (p=0.18).
The extent of involvement of the temporal and axillary arteries of the 16 patients in the subclinical GCA group was compared to a cohort of 57 GCA patients. The total halo count was similar for both subclinical GCA in PMR and classic GCA patients at 4.33 and 4.36 respectively. However, GCA patients had higher halo scores in both temporal and axillary vessels of 13.17 and 13.28 respectively, compared to those with subclinical GCA with halo scores of 4.68 and 9.75. This suggests that patients with subclinical GCA in PMR have less vessel wall oedema than those with GCA. The subclinical GCA group had higher halo scores in the axillary arteries versus the temporal arteries, (p=0.0074) suggesting a predilection for the axillary vessels.
Conclusion: Patients with subclinical GCA had higher halo scores in the axillary arteries compared to the temporal arteries suggesting an extracranial phenotype. Male gender and a higher ESR at the time of PMR diagnosis appear to be risk markers for subclinical GCA though this requires analysis in larger cohorts of patients.
.jpg)
S. Cowley: None; C. Kirby: None; P. Harkins: Janssen, 5; R. Conway: AbbVie/Abbott, 5, 6, Celltrion, 5, Fresenius Kabi, 6, Galapagos, 6, Janssen, 5, 6, Nordic Pharma, 5, Novartis, 5, UCB, 6, Viatris, 6; D. Kane: None.
Background/Purpose: It has been reported that more than a quarter of patients with polymyalgia rheumatica (PMR) have subclinical giant cell arteritis (GCA). It remains unclear if all PMR patients should have ultrasound assessment for subclinical GCA or if there are certain phenotypes of patients that are more at risk of having subclinical GCA.
Methods: Newly diagnosed PMR patients who met a clinical diagnosis for PMR, verified by two rheumatologists were examined with vascular ultrasound (US) of their temporal and axillary arteries. US of all 6 branches of the superficial temporal and both axillary arteries was performed using a GE P9 device. Sonographic abnormalities considered indicative of vasculitis in the temporal arteries included the halo sign and non-compressible arteries with a thickened intima-media complex. An intima-media thickness of 0.42mm for the common superficial temporal branch, 0.34mm for the frontal branch, and 0.29mm for the parietal branch was considered positive. In the axillary arteries, a halo sign, and an intima-media thickness of >1.0mm was considered positive. Clinical and laboratory characteristics were recorded. Halo scores were calculated for positive cases. Ultrasound findings were compared to a cohort of GCA patients.
Results: 91 patients with newly diagnosed PMR and 57 patients with newly diagnosed GCA were included. ACR/EULAR classification criteria were met in 67 of those with PMR (primarily due to prior corticosteroid use in primary care resulting in normal ESR/CRP) and all of those with GCA. Of the 91 patients with PMR, 16 were identified as having subclinical GCA on ultrasound (17.5%).
The mean age at time of diagnosis was 69 years for those with PMR, 70 years for those with subclinical GCA in PMR and 74 years for those with GCA. Males were more likely to have subclinical GCA in PMR, accounting for 12 (75%) of the subclinical GCA group compared to 27 (36%) of the pure PMR group (p=0.045). The mean ESR at baseline for those with subclinical GCA in PMR was higher than those with isolated PMR; 49mm/hr compared to 38mm/hr (p=0.18).
The extent of involvement of the temporal and axillary arteries of the 16 patients in the subclinical GCA group was compared to a cohort of 57 GCA patients. The total halo count was similar for both subclinical GCA in PMR and classic GCA patients at 4.33 and 4.36 respectively. However, GCA patients had higher halo scores in both temporal and axillary vessels of 13.17 and 13.28 respectively, compared to those with subclinical GCA with halo scores of 4.68 and 9.75. This suggests that patients with subclinical GCA in PMR have less vessel wall oedema than those with GCA. The subclinical GCA group had higher halo scores in the axillary arteries versus the temporal arteries, (p=0.0074) suggesting a predilection for the axillary vessels.
Conclusion: Patients with subclinical GCA had higher halo scores in the axillary arteries compared to the temporal arteries suggesting an extracranial phenotype. Male gender and a higher ESR at the time of PMR diagnosis appear to be risk markers for subclinical GCA though this requires analysis in larger cohorts of patients.
.jpg)
Figure 1: Results
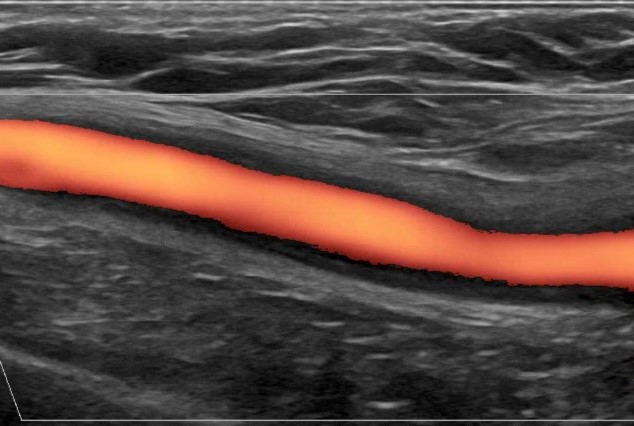
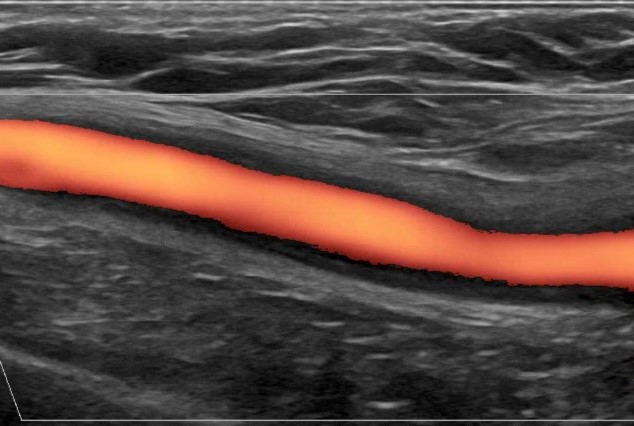
Figure 2: Axillary artery with halo sign
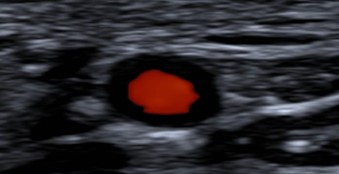
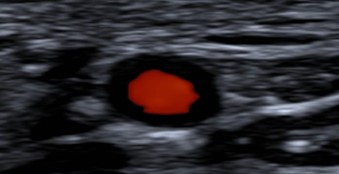
Figure 3: Temporal artery with halo sign
S. Cowley: None; C. Kirby: None; P. Harkins: Janssen, 5; R. Conway: AbbVie/Abbott, 5, 6, Celltrion, 5, Fresenius Kabi, 6, Galapagos, 6, Janssen, 5, 6, Nordic Pharma, 5, Novartis, 5, UCB, 6, Viatris, 6; D. Kane: None.



