Poster Session C
Rheumatoid arthritis (RA)
Session: (2095–2140) RA – Diagnosis, Manifestations, and Outcomes Poster III
2098: Contribution of Rare Deleterious Exonic Variants in Telomere Related Genes to Interstitial Lung Disease Risk in Patients with Rheumatoid Arthritis
Tuesday, November 14, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- PJ
Pierre-Antoine Juge, MD, PhD (he/him/his)
Division of Rheumatology, Inflammation, and Immunity Brigham & Women’s Hospital
Boston, MA, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Pierre-Antoine Juge1, Leticia Kawano-Dourado2, Steven Gazal3, Gregory McDermott4, Keigo Hayashi4, Jing Cui5, Marie-Pierre Debray6, Lidwine Stervinou-Wemeau7, Syvain Marchand-Adam8, Christophe Richez9, Hilario Nunes10, Jérôme Avouac11, Rene-Marc Flipo12, Vincent Cottin13, Martin Soubrier14, Nathalie Saidenberg Kermanac'h10, Caroline Kannengiesser15, Raphael Borie16, Bruno Crestani17, Tracy J. Doyle4, Soumya Raychaudhuri4, Elizabeth Karlson4, Jeffrey Sparks18 and Philippe Dieudé19, 1Division of Rheumatology, Inflammation, and Immunity Brigham & Women's Hospital, Boston, MA, 2Hospital do Coração (HCor), São Paulo, Brazil, 3University of South California, Los Angeles, CA, 4Brigham and Women's Hospital, Boston, MA, 5Brigham and Women's Hospital, Boston, MA, 6CHU Bichat, Radiology, Paris, France, 7CHRU de Lille, Lille, France, 8CHU Tours, Tours, France, 9Université de Bordeaux, Bordeaux, France, 10CHU Avicenne, Bobigny, France, 11Service de Rhumatologie, Hôpital Cochin, AP-HP.Centre – Université Paris Cité, Paris, France, 12La Lettre du Rhumatologue, Paris, France, 13Coordinating Reference Center for Rare Pulmonary Diseases, Louis Pradel Hospital, University of Lyon, INRAE, Lyon, France, 14Gabriel-Montpied Hospital, Clermont-ferrand, France, 15CHU Bichat, Paris, France, 16Bichat-Claude Bernard, Universite de Paris, Paris, France, 17Hopital Bichat, Paris University, Paris, France, 18Division of Rheumatology, Inflammation, and Immunity, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, 19Assistance Publique-Hôpitaux de Paris, Bichat-Claude Bernard University Hospital, INSERM UMR1152, University de Paris Cité, Department of Rheumatology, Paris, France
Background/Purpose: RA-associated interstitial lung disease (ILD) and idiopathic pulmonary fibrosis (IPF) share genetic risk factors such as MUC5B rs35705950. The exact role of telomere related genes (TRG) in the RA-ILD genetic background is unclear. A previous work found an excess of TRG rare deleterious variants in RA-ILD compared to healthy controls but did not allow to conclude without a control population of patients with RA without ILD. Our aim was to test for association TRG rare deleterious exonic variants with ILD in patients with RA.
Methods: This genetic case-control association study was composed of a derivation (France) and a replication (US) population. Cases with RA-ILD and controls with RA without ILD (RA-noILD) that had whole exome sequencing (WES) data were included. ILD status and pattern (usual interstitial pattern, UIP or non-UIP) was determined by review of clinically-indicated high-resolution computed tomography (HRCT) chest imaging. Rare deleterious exonic variants from 14 candidate TRG previously associated with pulmonary fibrosis (TERT, TERC, PARN, RTEL1, CTC1, TINF2, ACD, POT1, NAF1, ZCCHC8, NHP2, NOP10, WRAP53, and DKC1) were selected using 1) a reported frequency in gnomAD database < 0.1%, 2) a deleterious impact predicted by SIFT, POLYPHEN-2, and 3) a CADD score > 15. Proportions of variants carriers in RA-ILD and RA-noILD were compared using a classical burden test adjusted for sex, age at RA, RA duration, MUC5B rs3570590 genotype and a principal component analysis using ancestry informative markers. Results were combined in a meta-analysis.
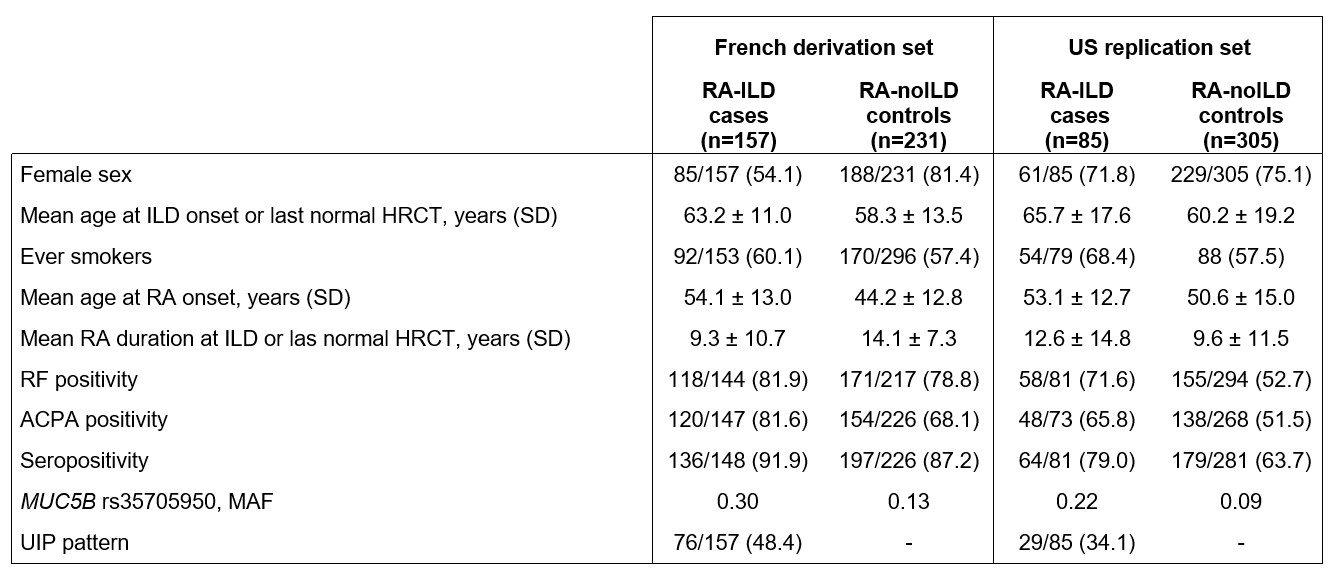
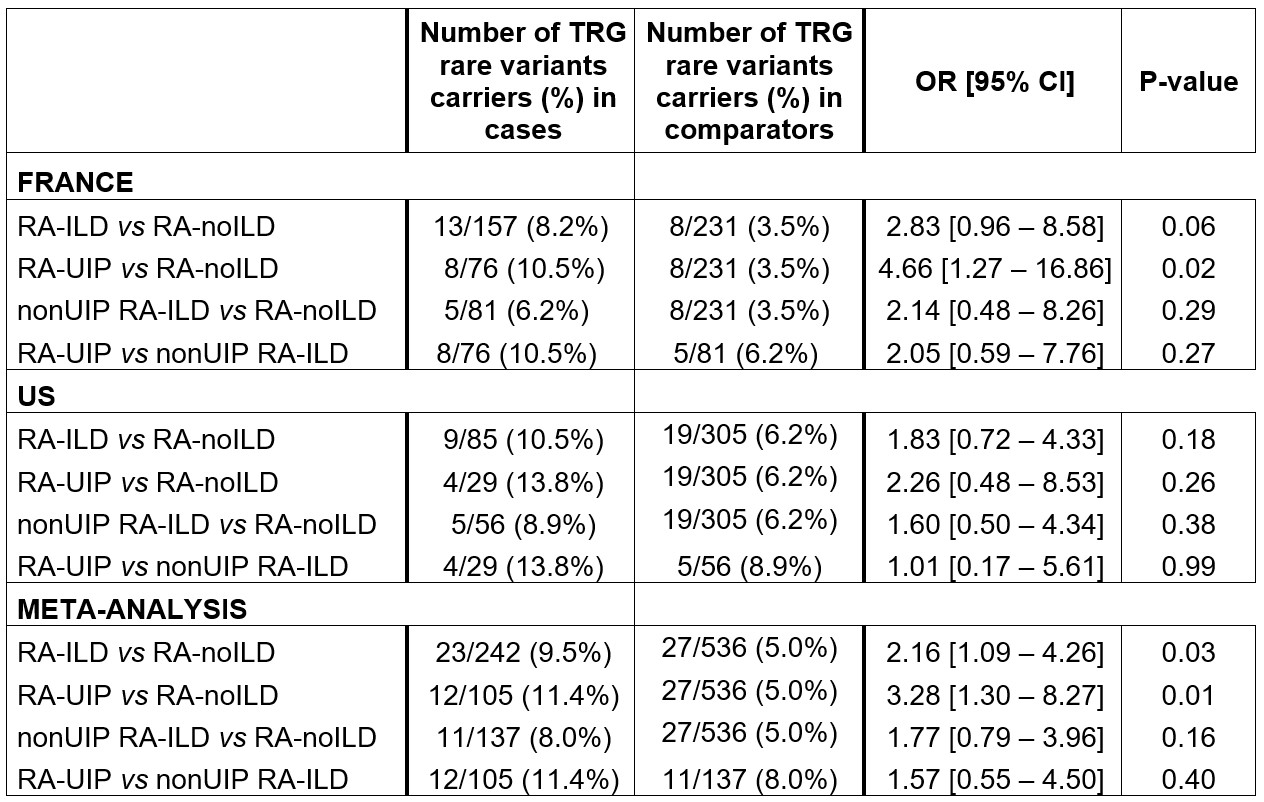
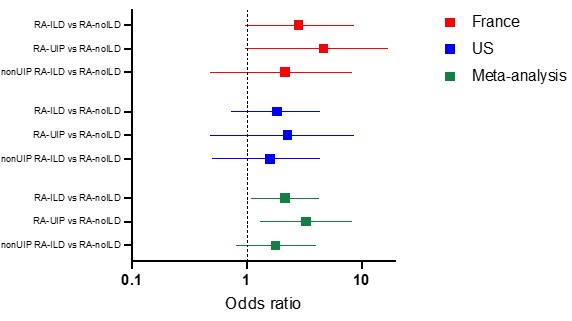
Results: The French derivation dataset included 388 patients, 157 cases (40.5%), mean age at ILD or last normal HRTC 60.1 years, 273 female (70.4%); Table 1. 22 rare deleterious variants were identified in 13/157 cases (8.3%) and 8/231 controls (3.5%). The burden test suggested an excess of TRG rare variants in RA-ILD (OR 2.83, 95% CI 0.96-8.58; p=0.06); (Table 2, Figure 1). A significant association was observed for usual interstitial pneumonia (UIP) HRCT pattern (OR 4.66, 95% CI 1.27-16.86; p=0.02) whereas no association was detected for patients with RA-ILD and a non-UIP HRCT patterns (OR 2.14, 95% CI 0.48-8.26; p=0.29). The US replication dataset included 390 patients, 85 cases (21.8%), mean age at ILD or last normal HRCT was 61.4 years and 74.4% were female. Similar trend for an excess of TRG rare variants was observed with 28 variants identified in 9/85 cases and 19/305 controls (10.5% vs 6.2%, OR 1.83, 95% CI 0.72-4.33; p=0.18); (Table 2, Figure 1). Like in the derivation population, the excess of rare variants was more pronounced for RA-UIP: 13.8% vs 6.2% (OR 2.26, 95% CI 0.48-8.53; p=0.26) The meta-analysis provide evidence for a significant contribution of TRGs rare variants to RA-ILD (OR 2.16, 95% CI 1.09-4.26; p=0.03), more specifically for the UIP pattern (OR 3.28, 95% CI 1.30-8.27; p=0.01). No significant association was found for non-UIP patterns in the meta-analysis (OR 1.77, 95% CI 0.79-3.96; p=0.16).
Conclusion: TRG rare deleterious exonic variants contribute to the risk of ILD in patients with RA, more specifically in RA-UIP. These results confirmed the shared genetic architecture between RA-ILD and IPF.
P. Juge: None; L. Kawano-Dourado: None; S. Gazal: None; G. McDermott: None; K. Hayashi: None; J. Cui: None; M. Debray: None; L. Stervinou-Wemeau: None; S. Marchand-Adam: None; C. Richez: AbbVie/Abbott, 2, 6, Amgen, 6, AstraZeneca, 2, 6, Bristol-Myers Squibb(BMS), 6, Eli Lilly, 6, 12, receipt of drugs, GlaxoSmithKlein(GSK), 2, 6, Novartis, 2, 6, Pfizer, 2, 6; H. Nunes: None; J. Avouac: AbbVie, 6, AstraZeneca, 6, Biogen, 6, BMS, 5, 6, Fresenius Kabi, 5, 6, Galapagos, 5, 6, Janssen, 6, Lilly, 6, Medac, 6, MSD, 6, Nordic Pharma, 6, Novartis, 6, Novartis (Dreamer), 5, Pfizer, 6, Pfizer (Passerelle), 5, Roche-Chugai, 6, Sandoz, 6, Sanofi, 6; R. Flipo: AbbVie, 2, Bristol-Myers Squibb(BMS), 2, Eli Lilly, 2, Janssen, 2, Medac, 2, MSD, 2, Nordic Pharma, 2, Novartis, 2, Pfizer, 2, Roche-Chugaï, 2, Sandoz, 2, Sanofi, 2; V. Cottin: Boehringer Ingelheim, 2, 5, 6, 12, Support for attending meetings, Celgene/BMS, 1, 2, CSL Behring, 2, Ferrer, 2, 6, 12, Support for attending meetings, FibroGen, 1, Galapagos, 1, 2, Galecto, 1, GlaxoSmithKline, 2, Pliant, 2, Pure Tech, 2, Redx, 2, Roche, 1, 2, 6, 12, Support for attending meetings, Sanofi, 2, Shionogi, 2; M. Soubrier: None; N. Saidenberg Kermanac'h: None; C. Kannengiesser: None; R. Borie: None; B. Crestani: None; T. Doyle: None; S. Raychaudhuri: AbbVie, 6, Janssen, 1, Mestag, Inc, 2, 8, Pfizer, 1, Sanofi, 1, Sonoma, 1, 8; E. Karlson: None; J. Sparks: AbbVie, 2, Amgen, 2, Boehringer Ingelheim, 2, Bristol-Myers Squibb, 2, 5, Gilead, 2, Inova Diagnostics, 2, Janssen, 2, Optum, 2, Pfizer, 2, ReCor, 2; P. Dieudé: AbbVie, 2, 6, Boehringer Ingelheim, 1, 2, 6, Bristol-Myers Squibb, 1, 2, 5, 6, Chugai, 5, Galapagos, 5, 6, Janssen, 2, 6, Novartis, 2, Pfizer, 1, 2, 5, 6.
Background/Purpose: RA-associated interstitial lung disease (ILD) and idiopathic pulmonary fibrosis (IPF) share genetic risk factors such as MUC5B rs35705950. The exact role of telomere related genes (TRG) in the RA-ILD genetic background is unclear. A previous work found an excess of TRG rare deleterious variants in RA-ILD compared to healthy controls but did not allow to conclude without a control population of patients with RA without ILD. Our aim was to test for association TRG rare deleterious exonic variants with ILD in patients with RA.
Methods: This genetic case-control association study was composed of a derivation (France) and a replication (US) population. Cases with RA-ILD and controls with RA without ILD (RA-noILD) that had whole exome sequencing (WES) data were included. ILD status and pattern (usual interstitial pattern, UIP or non-UIP) was determined by review of clinically-indicated high-resolution computed tomography (HRCT) chest imaging. Rare deleterious exonic variants from 14 candidate TRG previously associated with pulmonary fibrosis (TERT, TERC, PARN, RTEL1, CTC1, TINF2, ACD, POT1, NAF1, ZCCHC8, NHP2, NOP10, WRAP53, and DKC1) were selected using 1) a reported frequency in gnomAD database < 0.1%, 2) a deleterious impact predicted by SIFT, POLYPHEN-2, and 3) a CADD score > 15. Proportions of variants carriers in RA-ILD and RA-noILD were compared using a classical burden test adjusted for sex, age at RA, RA duration, MUC5B rs3570590 genotype and a principal component analysis using ancestry informative markers. Results were combined in a meta-analysis.
Results: The French derivation dataset included 388 patients, 157 cases (40.5%), mean age at ILD or last normal HRTC 60.1 years, 273 female (70.4%); Table 1. 22 rare deleterious variants were identified in 13/157 cases (8.3%) and 8/231 controls (3.5%). The burden test suggested an excess of TRG rare variants in RA-ILD (OR 2.83, 95% CI 0.96-8.58; p=0.06); (Table 2, Figure 1). A significant association was observed for usual interstitial pneumonia (UIP) HRCT pattern (OR 4.66, 95% CI 1.27-16.86; p=0.02) whereas no association was detected for patients with RA-ILD and a non-UIP HRCT patterns (OR 2.14, 95% CI 0.48-8.26; p=0.29). The US replication dataset included 390 patients, 85 cases (21.8%), mean age at ILD or last normal HRCT was 61.4 years and 74.4% were female. Similar trend for an excess of TRG rare variants was observed with 28 variants identified in 9/85 cases and 19/305 controls (10.5% vs 6.2%, OR 1.83, 95% CI 0.72-4.33; p=0.18); (Table 2, Figure 1). Like in the derivation population, the excess of rare variants was more pronounced for RA-UIP: 13.8% vs 6.2% (OR 2.26, 95% CI 0.48-8.53; p=0.26) The meta-analysis provide evidence for a significant contribution of TRGs rare variants to RA-ILD (OR 2.16, 95% CI 1.09-4.26; p=0.03), more specifically for the UIP pattern (OR 3.28, 95% CI 1.30-8.27; p=0.01). No significant association was found for non-UIP patterns in the meta-analysis (OR 1.77, 95% CI 0.79-3.96; p=0.16).
Conclusion: TRG rare deleterious exonic variants contribute to the risk of ILD in patients with RA, more specifically in RA-UIP. These results confirmed the shared genetic architecture between RA-ILD and IPF.
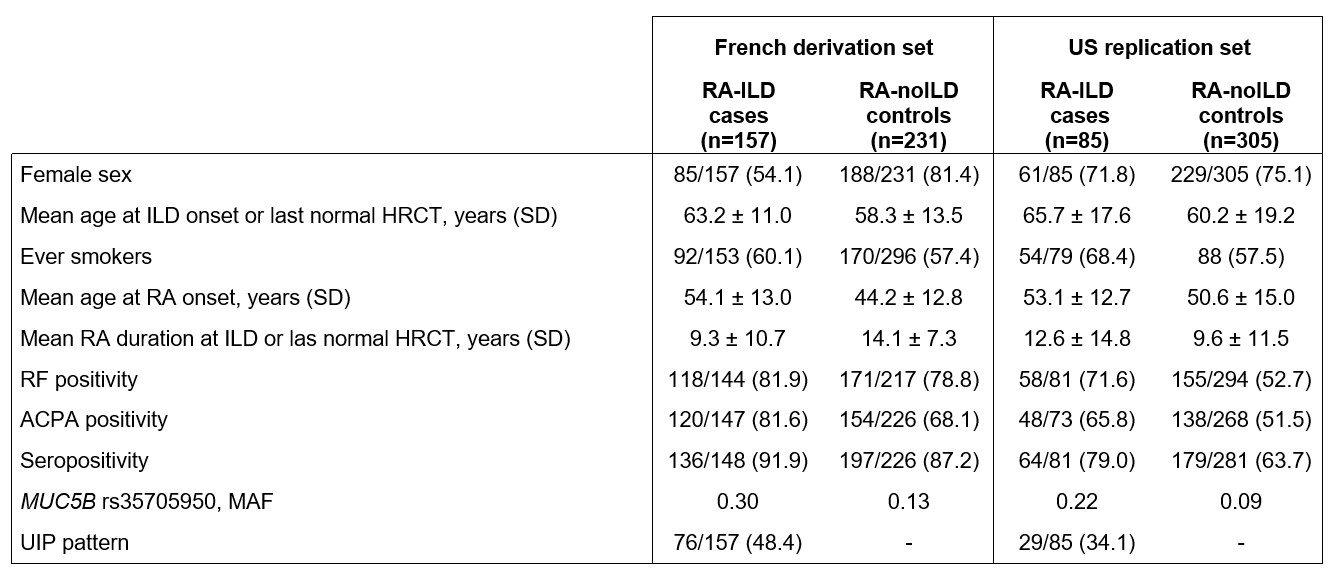
Table 1. Characteristics of the included patients
ACPA: anti-citrullinated peptides antibodies; HRCT: high resolution computed tomography; ILD: interstitial lung disease; MAF: minor allele frequency; RF: rheumatoid factor; UIP: usual interstitial pneumonia.
ACPA: anti-citrullinated peptides antibodies; HRCT: high resolution computed tomography; ILD: interstitial lung disease; MAF: minor allele frequency; RF: rheumatoid factor; UIP: usual interstitial pneumonia.
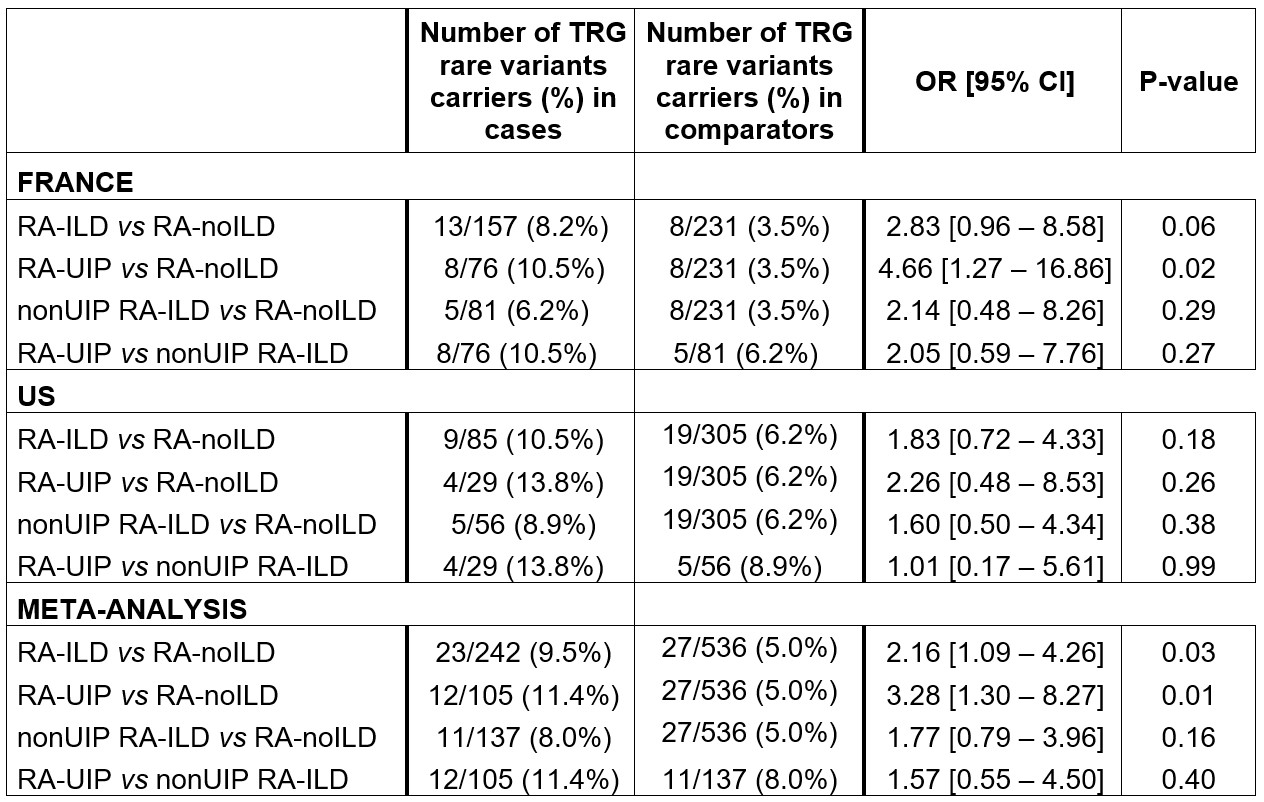
Table 2. Classical burden test comparing the frequency of TRG rare deleterious variants in patients with RA-ILD (cases) and patients with RA-noILD (controls).
ILD: interstitial lung disease, OR [95% IC]: Odd ratios with 95% confidence interval; TRGs: telomere related genes; UIP: usual interstitial pneumonia.
ILD: interstitial lung disease, OR [95% IC]: Odd ratios with 95% confidence interval; TRGs: telomere related genes; UIP: usual interstitial pneumonia.
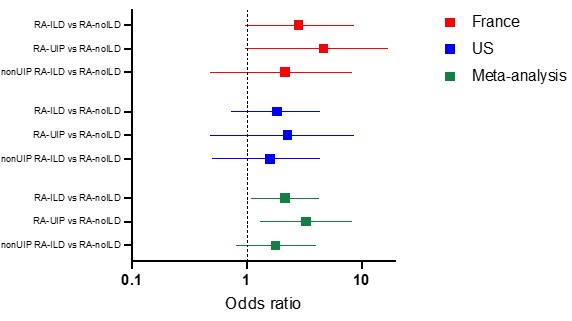
Figure 1. Results from the Burden test assessing TRG rare deleterious variants contribution in RA-ILD.
Forest plot of odds ratios (OR) and 95% confidence intervals (CI). The boxes indicate OR, and the horizontal lines indicate 95% CI for the burden test comparing frequency of telomere related genes (TRG) rare deleterious exonic variants carriers in cases vs controls.
Forest plot of odds ratios (OR) and 95% confidence intervals (CI). The boxes indicate OR, and the horizontal lines indicate 95% CI for the burden test comparing frequency of telomere related genes (TRG) rare deleterious exonic variants carriers in cases vs controls.
P. Juge: None; L. Kawano-Dourado: None; S. Gazal: None; G. McDermott: None; K. Hayashi: None; J. Cui: None; M. Debray: None; L. Stervinou-Wemeau: None; S. Marchand-Adam: None; C. Richez: AbbVie/Abbott, 2, 6, Amgen, 6, AstraZeneca, 2, 6, Bristol-Myers Squibb(BMS), 6, Eli Lilly, 6, 12, receipt of drugs, GlaxoSmithKlein(GSK), 2, 6, Novartis, 2, 6, Pfizer, 2, 6; H. Nunes: None; J. Avouac: AbbVie, 6, AstraZeneca, 6, Biogen, 6, BMS, 5, 6, Fresenius Kabi, 5, 6, Galapagos, 5, 6, Janssen, 6, Lilly, 6, Medac, 6, MSD, 6, Nordic Pharma, 6, Novartis, 6, Novartis (Dreamer), 5, Pfizer, 6, Pfizer (Passerelle), 5, Roche-Chugai, 6, Sandoz, 6, Sanofi, 6; R. Flipo: AbbVie, 2, Bristol-Myers Squibb(BMS), 2, Eli Lilly, 2, Janssen, 2, Medac, 2, MSD, 2, Nordic Pharma, 2, Novartis, 2, Pfizer, 2, Roche-Chugaï, 2, Sandoz, 2, Sanofi, 2; V. Cottin: Boehringer Ingelheim, 2, 5, 6, 12, Support for attending meetings, Celgene/BMS, 1, 2, CSL Behring, 2, Ferrer, 2, 6, 12, Support for attending meetings, FibroGen, 1, Galapagos, 1, 2, Galecto, 1, GlaxoSmithKline, 2, Pliant, 2, Pure Tech, 2, Redx, 2, Roche, 1, 2, 6, 12, Support for attending meetings, Sanofi, 2, Shionogi, 2; M. Soubrier: None; N. Saidenberg Kermanac'h: None; C. Kannengiesser: None; R. Borie: None; B. Crestani: None; T. Doyle: None; S. Raychaudhuri: AbbVie, 6, Janssen, 1, Mestag, Inc, 2, 8, Pfizer, 1, Sanofi, 1, Sonoma, 1, 8; E. Karlson: None; J. Sparks: AbbVie, 2, Amgen, 2, Boehringer Ingelheim, 2, Bristol-Myers Squibb, 2, 5, Gilead, 2, Inova Diagnostics, 2, Janssen, 2, Optum, 2, Pfizer, 2, ReCor, 2; P. Dieudé: AbbVie, 2, 6, Boehringer Ingelheim, 1, 2, 6, Bristol-Myers Squibb, 1, 2, 5, 6, Chugai, 5, Galapagos, 5, 6, Janssen, 2, 6, Novartis, 2, Pfizer, 1, 2, 5, 6.



