Poster Session C
Rheumatoid arthritis (RA)
Session: (2095–2140) RA – Diagnosis, Manifestations, and Outcomes Poster III
2139: Associations of Adipocytokines with Cancer Incidence in a Prospective Rheumatoid Arthritis Cohort
Tuesday, November 14, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- NS
Namrata Singh, MD, MSc
University of Washington
Bellevue, WA, United StatesDisclosure(s): Pfizer: Advisor or Review Panel Member (Terminated, April 29, 2022)
Abstract Poster Presenter(s)
Namrata Singh1, Aaron Baraff2, K Wysham3, Punyasha Roul4, Grant Cannon5, Brian Sauer6, Geoffrey Thiele4, Bryant England4, Ted R Mikuls7 and Joshua Baker8, 1University of Washington, Bellevue, WA, 2VA Puget Sound Seattle, Seattle, WA, 3VA Puget Sound/University of Washington, Seattle, WA, 4University of Nebraska Medical Center, Omaha, NE, 5University of Utah and Salt Lake City VA, Salt Lake City, UT, 6Salt Lake City VA/University of Utah, Salt Lake City, UT, 7Division of Rheumatology and Immunology, University of Nebraska Medical Center, Omaha, NE, 8University of Pennsylvania, Philadelphia, PA
Background/Purpose: A prior study suggested a higher risk of cancer mortality in patients with rheumatoid arthritis (RA) with higher levels of circulating leptin, an adipocytokine 1. Leptin and leptin receptor signaling pathway have been implicated in various key processes in cancer progression, such as cell proliferation, metastasis, and angiogenesis 2. We examined the associations between circulating adipocytokines with incident cancer in Veterans with RA.
Methods: Veterans enrolled in Veterans Affairs RA (VARA) registry, a multicenter prospective RA cohort, without a prior history of cancer were eligible for this study. Adipocytokines (adiponectin and leptin) were measured as part of a multi-analyte panel on banked serum at VARA enrollment. Records were linked to VA central cancer registry to identify incident cancers. Participants were followed from enrollment to the first of incident cancer, death, or end of study period (2/1/23). Associations between adipocytokine levels (divided into quartiles) and incident overall cancers were assessed in Cox regression models accounting for covariates (measured at baseline) including age, sex, RA disease activity, smoking status, and comorbidity burden estimated using rheumatic disease comorbidity index (RDCI). In a sub-analysis, we also assessed associations between adipocytokine levels and incident lung cancer, the most frequent malignancy in this cohort.
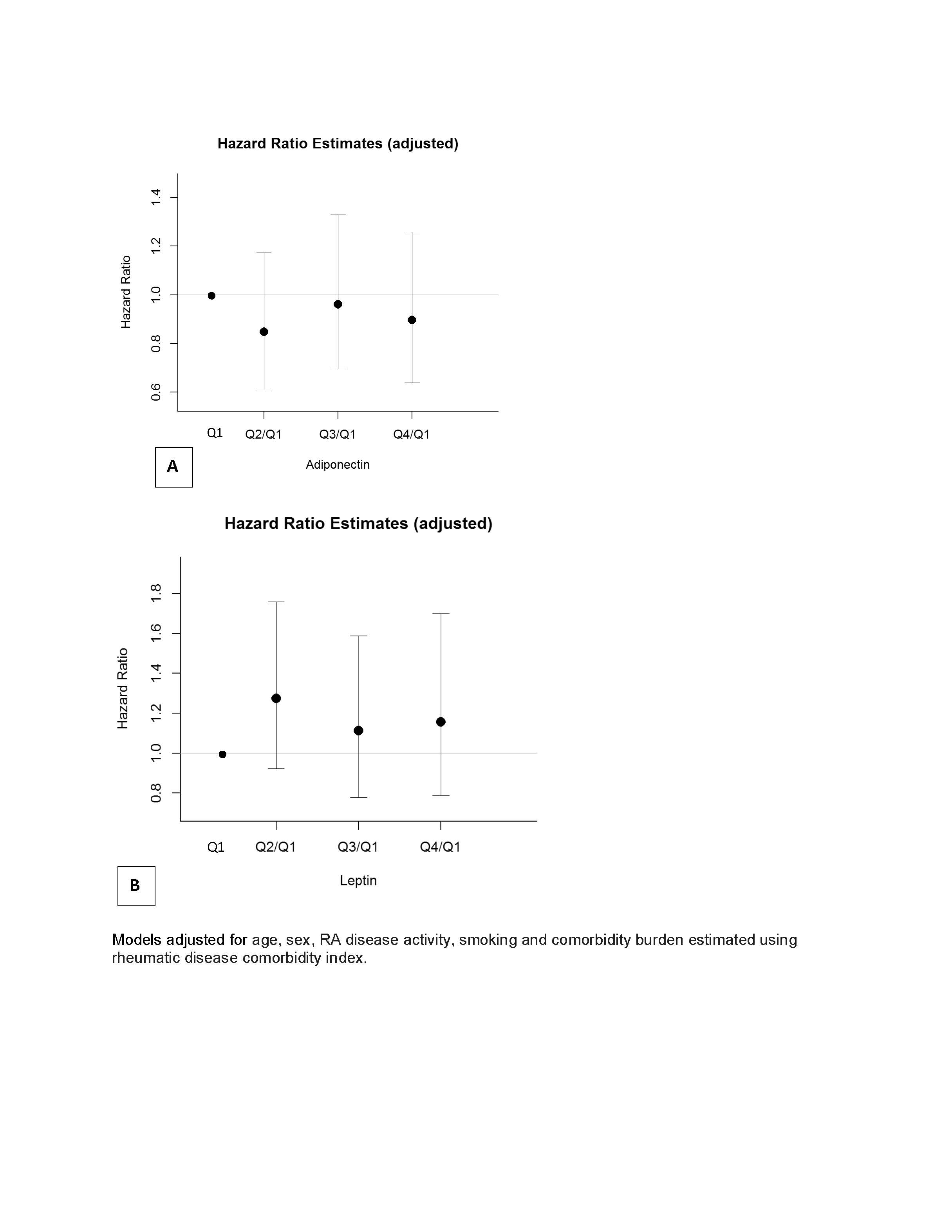
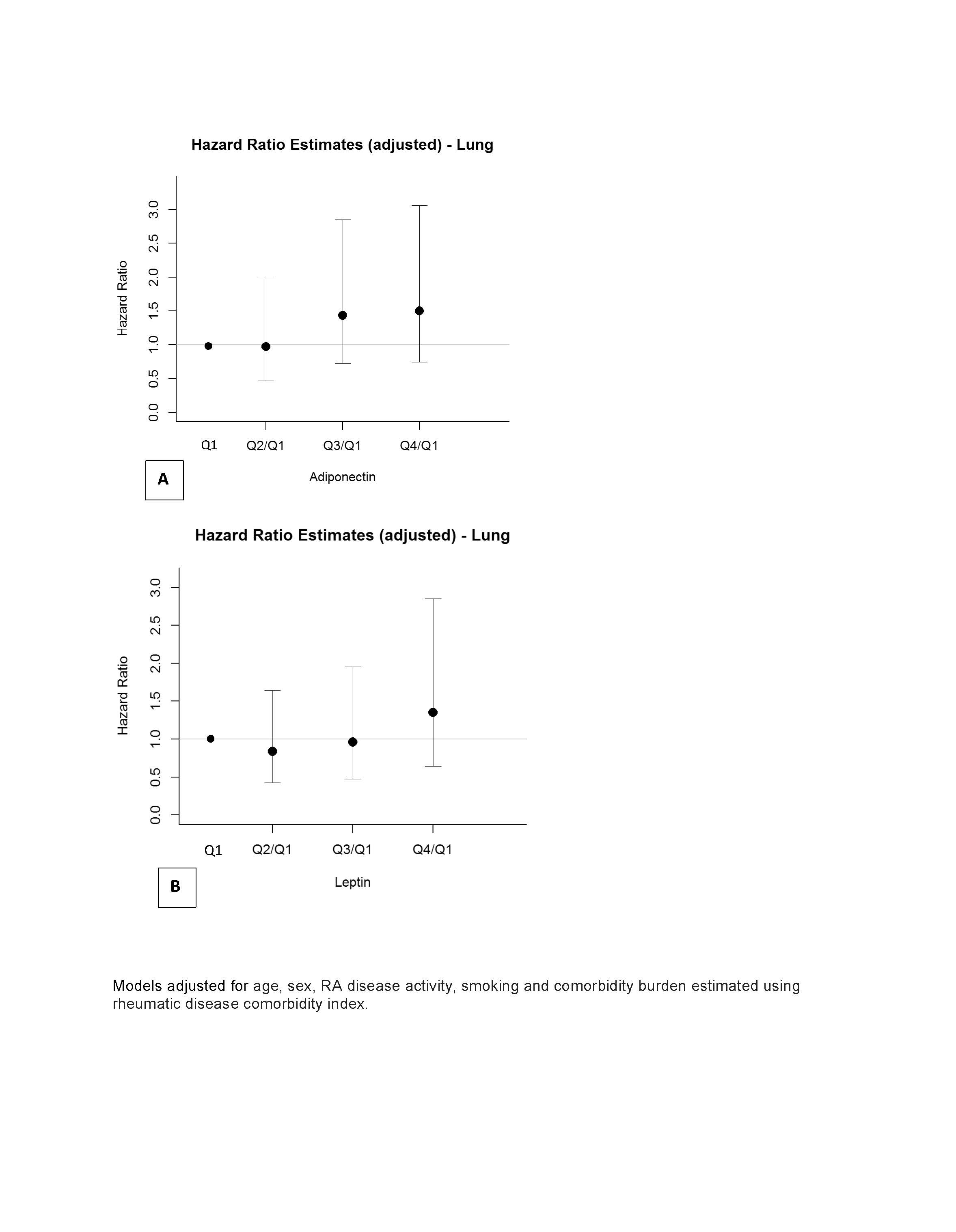
Results: 2391 Veterans met eligibility criteria of whom 87.7% were male. Higher adiponectin levels were associated with older age, lower BMI, former smoking status. Higher leptin levels were associated with higher BMI and higher comorbidity scores. Over a median (interquartile range) 6.2 (6.9) years of follow-up, there were 322 incident cancers. The most common cancers observed were: lung (n= 75), prostate (n= 61), gastrointestinal cancers (n=42), and hematological (n=40). In multivariable Cox Proportional hazard models, we did not observe a significant association between levels of adiponectin (HR 0.90, 95% confidence interval, CI, 0.64-1.26 for quartile 4 versus quartile 1) (Figure 1, panel A) or leptin (HR for quartile 4 versus first quartile 1.16, 95% CI 0.79-1.70) with incident cancer (Figure 1, panel B). Those with the highest adiponectin or leptin levels tended to have higher incidence of lung cancer although the associations were not statistically significant (Figure 2).
Conclusion: In this study, we did not observe an association between levels of adipocytokines and incident overall cancer risk and specifically lung cancer risk in Veterans with RA. Further studies will explore the association between adipocytokines and incidence of specific cancers, especially obesity-related cancers.
References: 1. Baker JF, England BR, George MD, et al. Elevations in adipocytokines and mortality in rheumatoid arthritis. Rheumatology (Oxford). 2022;61(12):4924-4934. 2. Lin TC, Hsiao M. Leptin and Cancer: Updated Functional Roles in Carcinogenesis, Therapeutic Niches, and Developments. Int J Mol Sci. 2021;22(6).
N. Singh: None; A. Baraff: None; K. Wysham: None; P. Roul: None; G. Cannon: None; B. Sauer: None; G. Thiele: None; B. England: Boehringer-Ingelheim, 2, 5; T. Mikuls: Elsevier, 9, Horizon Therapeutics, 2, 5, Pfizer, 2, Sanofi, 2, UCB Pharma, 2, Wolters Kluwer Health (UpToDate), 9; J. Baker: CorEvitas, 2, Cumberland Pharma, 2, Horizon Pharmaceuticals, 5.
Background/Purpose: A prior study suggested a higher risk of cancer mortality in patients with rheumatoid arthritis (RA) with higher levels of circulating leptin, an adipocytokine 1. Leptin and leptin receptor signaling pathway have been implicated in various key processes in cancer progression, such as cell proliferation, metastasis, and angiogenesis 2. We examined the associations between circulating adipocytokines with incident cancer in Veterans with RA.
Methods: Veterans enrolled in Veterans Affairs RA (VARA) registry, a multicenter prospective RA cohort, without a prior history of cancer were eligible for this study. Adipocytokines (adiponectin and leptin) were measured as part of a multi-analyte panel on banked serum at VARA enrollment. Records were linked to VA central cancer registry to identify incident cancers. Participants were followed from enrollment to the first of incident cancer, death, or end of study period (2/1/23). Associations between adipocytokine levels (divided into quartiles) and incident overall cancers were assessed in Cox regression models accounting for covariates (measured at baseline) including age, sex, RA disease activity, smoking status, and comorbidity burden estimated using rheumatic disease comorbidity index (RDCI). In a sub-analysis, we also assessed associations between adipocytokine levels and incident lung cancer, the most frequent malignancy in this cohort.
Results: 2391 Veterans met eligibility criteria of whom 87.7% were male. Higher adiponectin levels were associated with older age, lower BMI, former smoking status. Higher leptin levels were associated with higher BMI and higher comorbidity scores. Over a median (interquartile range) 6.2 (6.9) years of follow-up, there were 322 incident cancers. The most common cancers observed were: lung (n= 75), prostate (n= 61), gastrointestinal cancers (n=42), and hematological (n=40). In multivariable Cox Proportional hazard models, we did not observe a significant association between levels of adiponectin (HR 0.90, 95% confidence interval, CI, 0.64-1.26 for quartile 4 versus quartile 1) (Figure 1, panel A) or leptin (HR for quartile 4 versus first quartile 1.16, 95% CI 0.79-1.70) with incident cancer (Figure 1, panel B). Those with the highest adiponectin or leptin levels tended to have higher incidence of lung cancer although the associations were not statistically significant (Figure 2).
Conclusion: In this study, we did not observe an association between levels of adipocytokines and incident overall cancer risk and specifically lung cancer risk in Veterans with RA. Further studies will explore the association between adipocytokines and incidence of specific cancers, especially obesity-related cancers.
References: 1. Baker JF, England BR, George MD, et al. Elevations in adipocytokines and mortality in rheumatoid arthritis. Rheumatology (Oxford). 2022;61(12):4924-4934. 2. Lin TC, Hsiao M. Leptin and Cancer: Updated Functional Roles in Carcinogenesis, Therapeutic Niches, and Developments. Int J Mol Sci. 2021;22(6).
Figure 1. Multivariable model of adipocytokine quartiles and incident overall cancer with reference to quartile 1.
Figure 2. Multivariable model of adipocytokine quartiles and incident lung cancer with reference to quartile 1.
N. Singh: None; A. Baraff: None; K. Wysham: None; P. Roul: None; G. Cannon: None; B. Sauer: None; G. Thiele: None; B. England: Boehringer-Ingelheim, 2, 5; T. Mikuls: Elsevier, 9, Horizon Therapeutics, 2, 5, Pfizer, 2, Sanofi, 2, UCB Pharma, 2, Wolters Kluwer Health (UpToDate), 9; J. Baker: CorEvitas, 2, Cumberland Pharma, 2, Horizon Pharmaceuticals, 5.



