Poster Session C
Vasculitis
Session: (2370–2386) Vasculitis – ANCA-Associated Poster III: Biomarkers & Renal Outcomes
2382: Relapse of Patients with ANCA-associated Vasculitis Who Are on Dialysis
Tuesday, November 14, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- HS
Hansun Song, MD (he/him/his)
Asan medical center
Seoul, South KoreaDisclosure information not submitted.
Abstract Poster Presenter(s)
Yeo-Jin Lee1, Hansun Song2, Wook Jang Seo3, Jinseok Kim4, Soo-Min Ahn1, Ji-Seon Oh5, Yong-Gil Kim2, Chang-Keun Lee1, Bin Yoo1 and Seokchan Hong1, 1Asan Medical Center, Seoul, South Korea, 2Department of Rheumatology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, South Korea, 3Department of Rheumatology, Veteran Health Service Medical Center, Seoul, South Korea, 4Department of Rheumatology, Jeju National University Hospital, Jeju National University School of Medicine, Jeju-si, Jeju-do, South Korea, La Jolla, CA, South Korea, 5Department of Information Medicine, Big Data Research Center, Asan Medical Center, University of Ulsan College of Medicine, Ulsan, South Korea
Background/Purpose: It is known that disease activity of ANCA-associated vasculitis (AAV) is decreased after dialysis. However, most studies have been conducted on Caucasians, and factors associated with relapse during dialysis have not been well-studied. Therefore, this study aimed to elucidate the clinical manifestation of AAV relapse during dialysis, and identify factors associated with relapse, in an Asian country.
Methods: We retrospectively reviewed the data of patients diagnosed with AAV who were on dialysis due to renal involvement during follow-up from July 2005 to March 2021 at a single tertiary center in Seoul, Korea. Diagnosis of AAV was based on the International Chapel Hill Consensus Conference on the Nomenclature of Systemic Vasculitides. The patients on dialysis at the time of AAV diagnosis or during follow-up period were included in our study. Cox regression analysis was performed with the relapse as the dependent variable for the univariable and multivariable analysis.
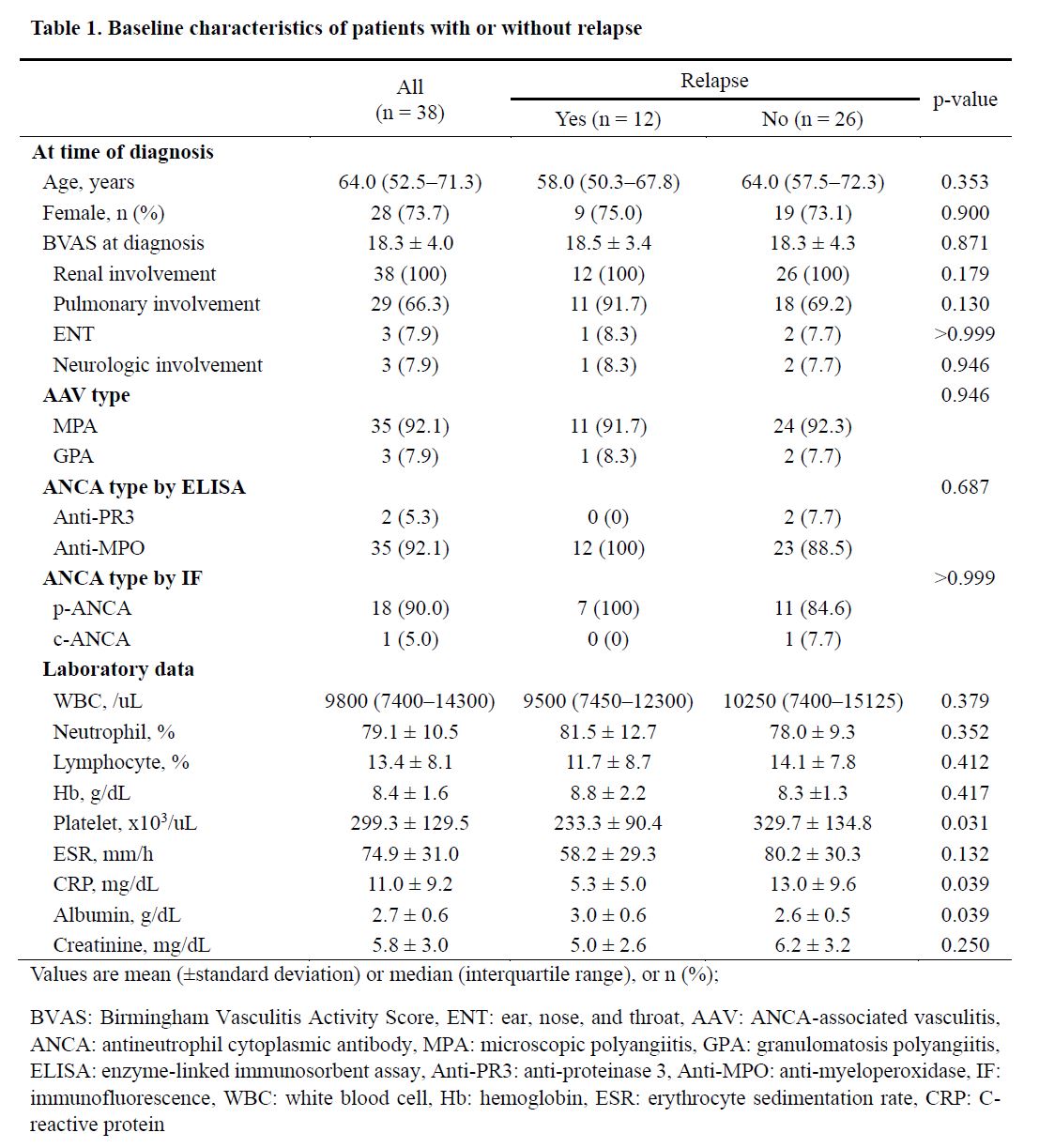
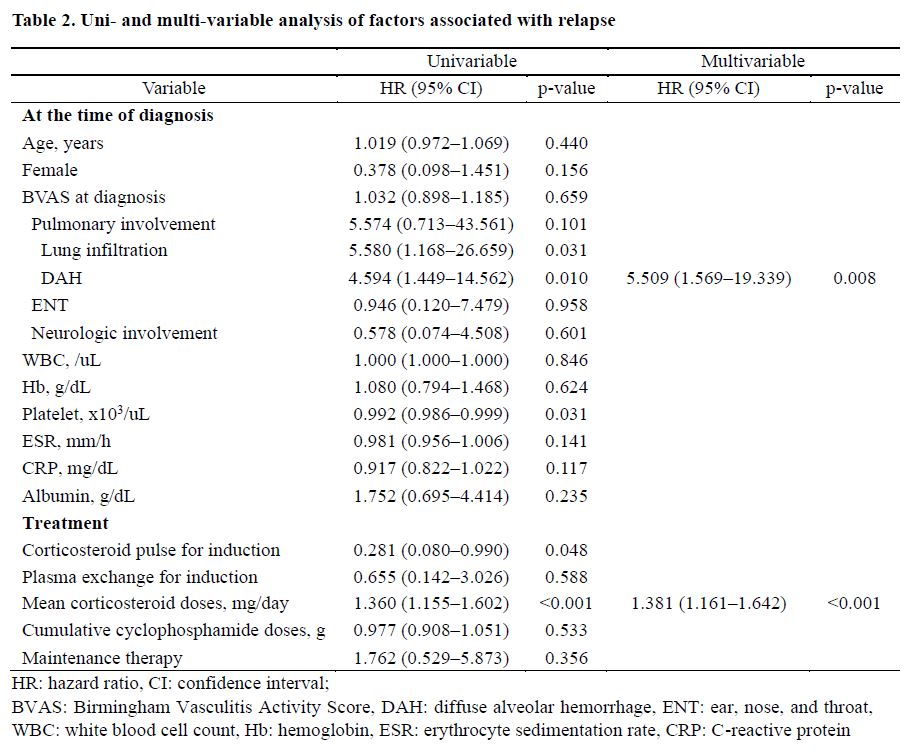
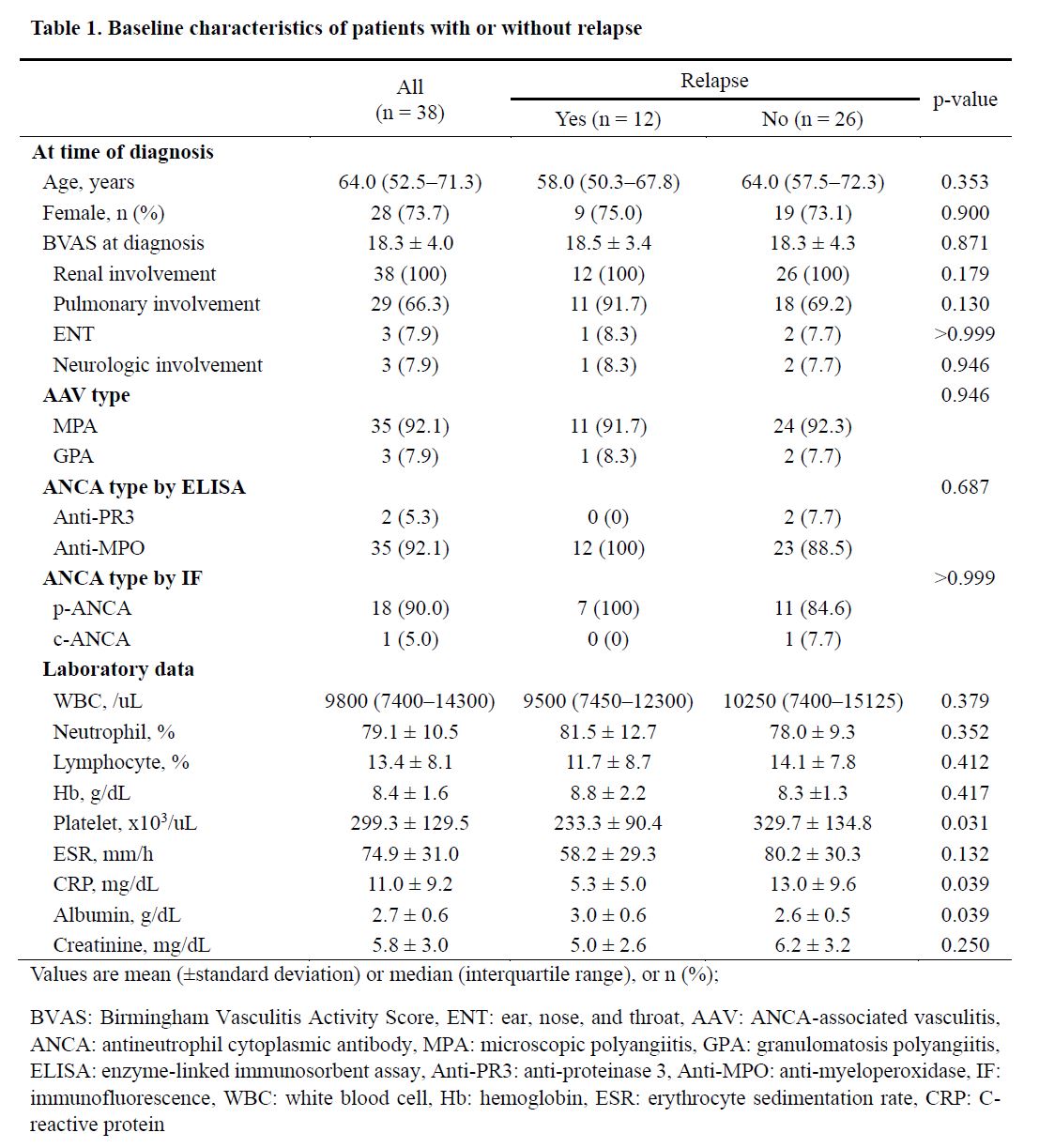
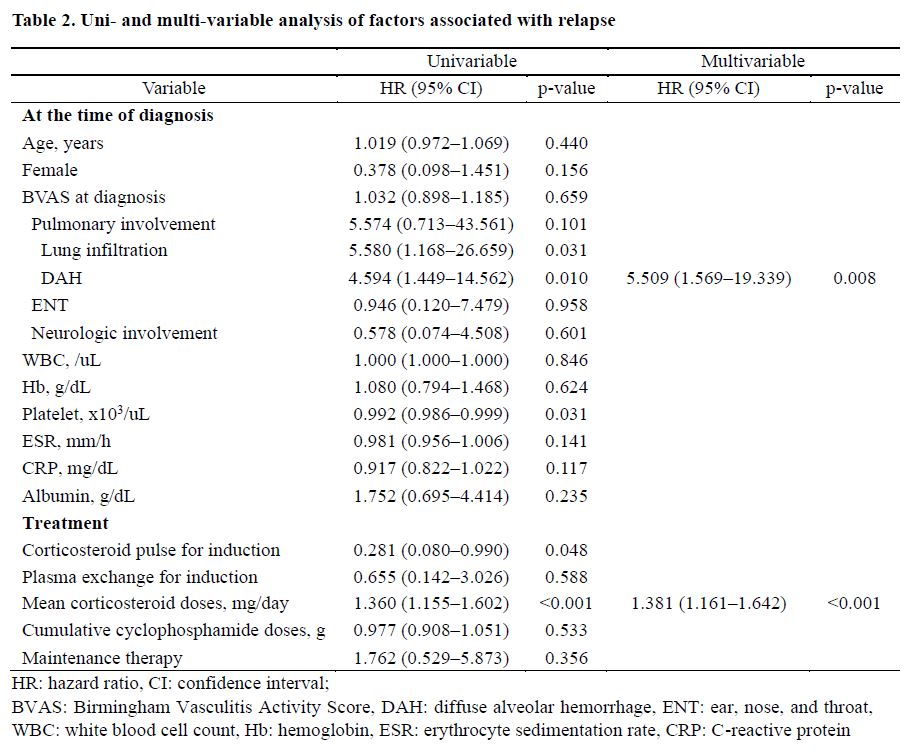
Results: A total of 38 patients were included in the present study. Median age of participants was 64.0 (52.5–71.3) years, 28 (73.7%) were female, and 92.1% had microscopic polyangiitis (MPA). At diagnosis, mean BVAS was 18.3 (± 4.0), and 66.3% of patients had pulmonary manifestations. Of them, 12 patients were relapsed during followed up for 59.7 (± 50.4) months after dialysis. Among patients who experienced relapse, 9 had diffuse alveolar hemorrhage (DAH), and interstitial lung disease (ILD) aggravation (n = 2) and DAH (n =1) were found. There were no significant differences in age, sex, or mean BVAS at baseline between relapse and non-relapse group. Treatment regimen including cyclophosphamide, plasmapheresis, and maintenance therapy with azathioprine did not show statistical differences between the two groups. However, in univariable analysis, significant associations were observed between lung infiltration [HR 5.580 (1.168–26.659), p=0.031], DAH [HR 4.594 (1.449–14.562), p=0.010], corticosteroid pulse for induction [HR 0.281 (0.080–0.990), p=0.048], and mean corticosteroid doses [HR 1.360 (1.155–1.602), p< 0.001] with AAV relapse. Multivariable analysis showed that DAH [5.509 (1.569–19.339), p=0.008] and mean corticosteroid doses [1.381 (1.161–1.642), p< 0.001] were significantly associated with relapse.
Conclusion: Pulmonary manifestation, including DAH at baseline, was significantly associated with AAV relapse, and a significant association between mean corticosteroid doses and relapse was found.
Y. Lee: None; H. Song: None; W. Seo: None; J. Kim: None; S. Ahn: None; J. Oh: None; Y. Kim: None; C. Lee: None; B. Yoo: None; S. Hong: None.
Background/Purpose: It is known that disease activity of ANCA-associated vasculitis (AAV) is decreased after dialysis. However, most studies have been conducted on Caucasians, and factors associated with relapse during dialysis have not been well-studied. Therefore, this study aimed to elucidate the clinical manifestation of AAV relapse during dialysis, and identify factors associated with relapse, in an Asian country.
Methods: We retrospectively reviewed the data of patients diagnosed with AAV who were on dialysis due to renal involvement during follow-up from July 2005 to March 2021 at a single tertiary center in Seoul, Korea. Diagnosis of AAV was based on the International Chapel Hill Consensus Conference on the Nomenclature of Systemic Vasculitides. The patients on dialysis at the time of AAV diagnosis or during follow-up period were included in our study. Cox regression analysis was performed with the relapse as the dependent variable for the univariable and multivariable analysis.
Results: A total of 38 patients were included in the present study. Median age of participants was 64.0 (52.5–71.3) years, 28 (73.7%) were female, and 92.1% had microscopic polyangiitis (MPA). At diagnosis, mean BVAS was 18.3 (± 4.0), and 66.3% of patients had pulmonary manifestations. Of them, 12 patients were relapsed during followed up for 59.7 (± 50.4) months after dialysis. Among patients who experienced relapse, 9 had diffuse alveolar hemorrhage (DAH), and interstitial lung disease (ILD) aggravation (n = 2) and DAH (n =1) were found. There were no significant differences in age, sex, or mean BVAS at baseline between relapse and non-relapse group. Treatment regimen including cyclophosphamide, plasmapheresis, and maintenance therapy with azathioprine did not show statistical differences between the two groups. However, in univariable analysis, significant associations were observed between lung infiltration [HR 5.580 (1.168–26.659), p=0.031], DAH [HR 4.594 (1.449–14.562), p=0.010], corticosteroid pulse for induction [HR 0.281 (0.080–0.990), p=0.048], and mean corticosteroid doses [HR 1.360 (1.155–1.602), p< 0.001] with AAV relapse. Multivariable analysis showed that DAH [5.509 (1.569–19.339), p=0.008] and mean corticosteroid doses [1.381 (1.161–1.642), p< 0.001] were significantly associated with relapse.
Conclusion: Pulmonary manifestation, including DAH at baseline, was significantly associated with AAV relapse, and a significant association between mean corticosteroid doses and relapse was found.
Y. Lee: None; H. Song: None; W. Seo: None; J. Kim: None; S. Ahn: None; J. Oh: None; Y. Kim: None; C. Lee: None; B. Yoo: None; S. Hong: None.



