Poster Session B
Osteoarthritis (OA) and related disorders
Session: (1183–1199) Osteoarthritis – Clinical Poster II
1186: Presence of Erosions Is Not a Risk Factor for the Development of Knee OA in a Hand OA Population: The Framingham OA Study
Monday, November 13, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- TV
Tine Vanhaverbeke, MD (she/her/hers)
Ghent University
Ghent, BelgiumDisclosure information not submitted.
Abstract Poster Presenter(s)
Tine Vanhaverbeke1, Gabriela Rabasa2, Ruth Wittoek1, Ida Kristin Haugen3 and David Felson2, 1Dept. of Rheumatology, Ghent University Hospital, Ghent University, Ghent, Belgium, 2Boston University, Boston, MA, 3Diakonhjemmet Hospital, Oslo, Norway
Background/Purpose: Osteoarthritis (OA) is a prevalent musculoskeletal disease and can affect multiple joint sites in one patient. Studies have shown an association between hand and knee OA (1). However, few studies have examined the association between erosive hand OA, a subtype of hand OA considered to be more inflammatory, and knee OA. The goal of this study was to assess the association between erosive hand OA and knee OA and to identify risk factors for the development of knee OA in a hand OA population.
Methods: All subjects were selected from the Offspring and Community cohorts of the Framingham OA study. Bilateral knee and hand radiographs were obtained and scored using the Kellgren-Lawrence grade (KLG). Radiographic tibiofemoral OA was defined as at least one knee having a KLG≥2. Symptomatic knee OA was defined as presence of radiographic OA, in combination with presence of frequent knee pain. Radiographic hand OA (RHOA) was defined as KLG≥2 in at least one hand joint, erosive hand OA as RHOA plus a central erosion and symptomatic hand OA as RHOA plus pain, aching or stiffness in the same joint. Crude prevalence and incidence numbers were calculated. Multivariable logistic regression analysis, adjusted for age, sex and BMI was performed.
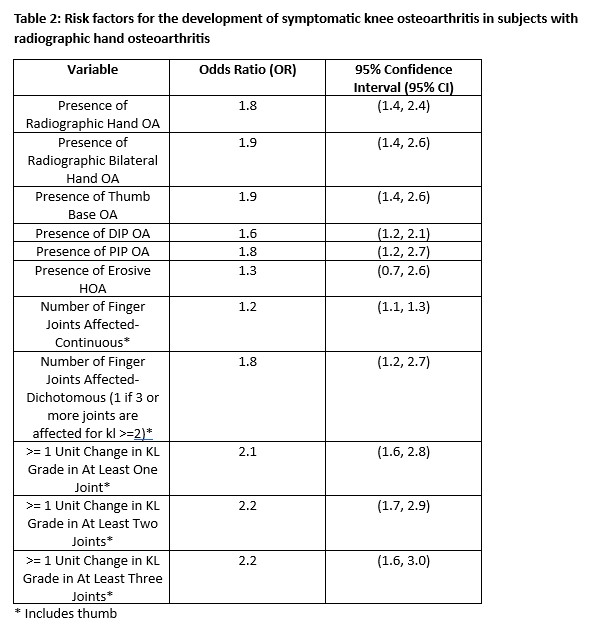
Results: In total, 1293 participants were studied. After adjustment for age, sex and BMI, presence of radiographic hand OA was associated with the development of symptomatic knee OA (OR 1.8 [1.4,2.4]). Similar results were found for symptomatic hand OA as the predictor (OR 1.9 [1.3,2.7]). However, compared with nonerosive hand OA, erosive hand OA was not identified as a risk factor for the development of symptomatic knee OA (OR 1.3 [0.7, 2.6]). Other risk factors identified for the development of symptomatic knee OA were: presence of thumb OA (vs. no thumb OA), presence of OA at a distal interphalangeal (DIP) joint, presence of OA at a proximal interphalangeal (PIP) joint, the number of finger joints affected and a change of at least 1 unit in KL grade in one or more hand joints (interphalangeal and thumb joints). .
Conclusion: This study confirms presence of hand OA is a risk factor for the development of knee OA. However, in a hand OA population, presence of erosions is not an additional risk factor. Our results may suggest that erosive hand OA is unrelated to OA in the knee.
References
< 1. Hirsch R et al. Association of hand and knee osteoarthritis: evidence for a polyarticular disease subset. Ann Rheum Dis. 1996 Jan;55(1):25-9.
.jpg)
T. Vanhaverbeke: AbbVie, 6; G. Rabasa: None; R. Wittoek: AbbVie, 2, Amgen, 5, Fresenius Kabi, 6, Galapagos, 6, Merck/MSD, 6, Pfizer, 5; I. Haugen: AbbVie/Abbott, 6, GlaxoSmithKlein(GSK), 6, Grünenthal, 6, Novartis, 6, Pfizer, 5; D. Felson: None.
Background/Purpose: Osteoarthritis (OA) is a prevalent musculoskeletal disease and can affect multiple joint sites in one patient. Studies have shown an association between hand and knee OA (1). However, few studies have examined the association between erosive hand OA, a subtype of hand OA considered to be more inflammatory, and knee OA. The goal of this study was to assess the association between erosive hand OA and knee OA and to identify risk factors for the development of knee OA in a hand OA population.
Methods: All subjects were selected from the Offspring and Community cohorts of the Framingham OA study. Bilateral knee and hand radiographs were obtained and scored using the Kellgren-Lawrence grade (KLG). Radiographic tibiofemoral OA was defined as at least one knee having a KLG≥2. Symptomatic knee OA was defined as presence of radiographic OA, in combination with presence of frequent knee pain. Radiographic hand OA (RHOA) was defined as KLG≥2 in at least one hand joint, erosive hand OA as RHOA plus a central erosion and symptomatic hand OA as RHOA plus pain, aching or stiffness in the same joint. Crude prevalence and incidence numbers were calculated. Multivariable logistic regression analysis, adjusted for age, sex and BMI was performed.
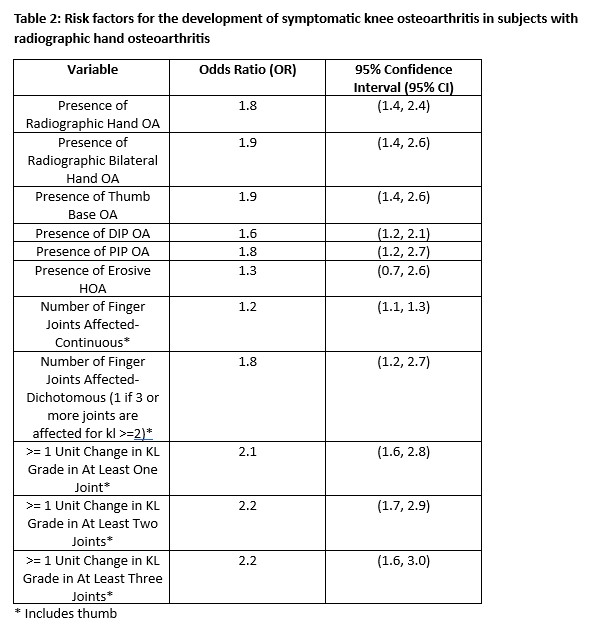
Results: In total, 1293 participants were studied. After adjustment for age, sex and BMI, presence of radiographic hand OA was associated with the development of symptomatic knee OA (OR 1.8 [1.4,2.4]). Similar results were found for symptomatic hand OA as the predictor (OR 1.9 [1.3,2.7]). However, compared with nonerosive hand OA, erosive hand OA was not identified as a risk factor for the development of symptomatic knee OA (OR 1.3 [0.7, 2.6]). Other risk factors identified for the development of symptomatic knee OA were: presence of thumb OA (vs. no thumb OA), presence of OA at a distal interphalangeal (DIP) joint, presence of OA at a proximal interphalangeal (PIP) joint, the number of finger joints affected and a change of at least 1 unit in KL grade in one or more hand joints (interphalangeal and thumb joints). .
Conclusion: This study confirms presence of hand OA is a risk factor for the development of knee OA. However, in a hand OA population, presence of erosions is not an additional risk factor. Our results may suggest that erosive hand OA is unrelated to OA in the knee.
References
< 1. Hirsch R et al. Association of hand and knee osteoarthritis: evidence for a polyarticular disease subset. Ann Rheum Dis. 1996 Jan;55(1):25-9.
.jpg)
T. Vanhaverbeke: AbbVie, 6; G. Rabasa: None; R. Wittoek: AbbVie, 2, Amgen, 5, Fresenius Kabi, 6, Galapagos, 6, Merck/MSD, 6, Pfizer, 5; I. Haugen: AbbVie/Abbott, 6, GlaxoSmithKlein(GSK), 6, Grünenthal, 6, Novartis, 6, Pfizer, 5; D. Felson: None.



