Poster Session B
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (1155–1182) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
1181: Real-World Myositis Antibody Frequency and Patient Awareness
Monday, November 13, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- RL
Raisa Lomanto Silva, MD (she/her/hers)
University of Pittsburgh Medical Center
Pittsburgh, PA, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Raisa Lomanto Silva1, shiri keret2, Akanksha Sharma3, Tanya Chandra4, Siamak Moghadam-Kia1, Chester V. Oddis5 and Rohit Aggarwal5, 1University of Pittsburgh Medical Center, Pittsburgh, PA, 2Bnai Zion, Atlit, Israel, 3UPMC Mercy Hospital, Pittsburgh, PA, 4Georgetown University Hospital, Washington, DC, 5University of Pittsburgh, Pittsburgh, PA
Background/Purpose: Myositis-specific antibodies (MSA) represent unique phenotypes in idiopathic inflammatory myopathies (IIM). Myositis-associated antibodies (MAA) most commonly occur in IIM overlap syndromes. MSA and MAA should be assessed in all IIM patients, but their real-world frequency, distribution, and patient awareness are not well known. Given the increasing importance of MSA/MAA in IIM diagnosis and management, we examined their real-world vs. expert-center frequency, awareness, and distribution.
Methods: Myositis Patient-Centered Tele-Research is a multi-center observational study. Patients were enrolled remotely from anywhere in the U.S. through social media and patient organizations (Tele-Research Cohort, TRC) and traditionally through myositis centers (Center-Based Cohort, CBC). Patients completed a pre-screening questionnaire with MSA/MAA and IIM self-report, the latter being confirmed by a rheumatologist, neurologist, or dermatologist. Patients also self-reported on study disease criteria: proximal muscle weakness, muscle or skin biopsy, electromyography, muscle enzyme, and/or dermatomyositis rashes. A subset of patients had their clinical features, diagnosis, and MSA/MAA results confirmed by physician chart review.
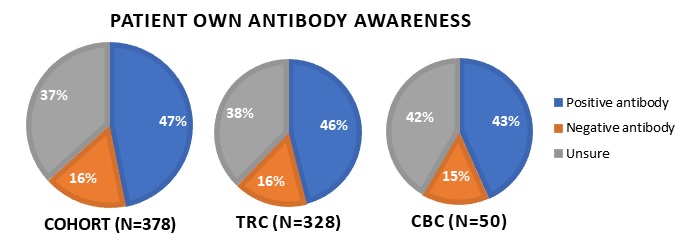
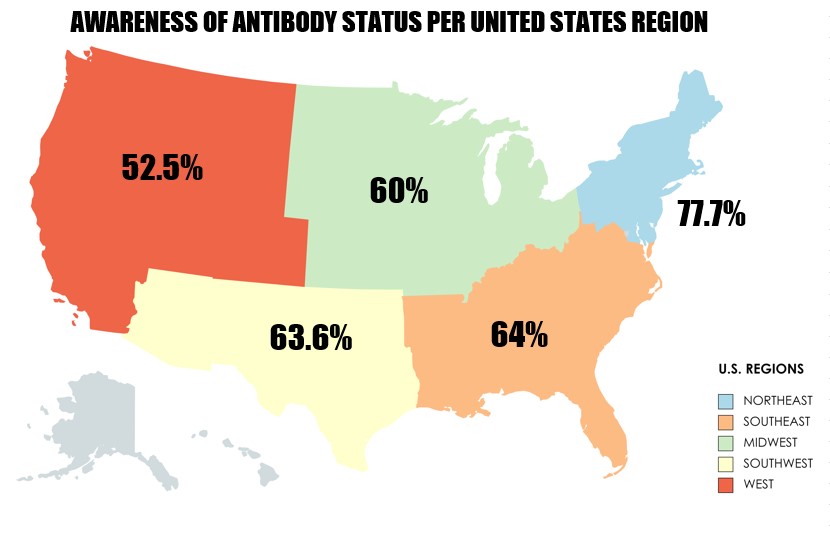
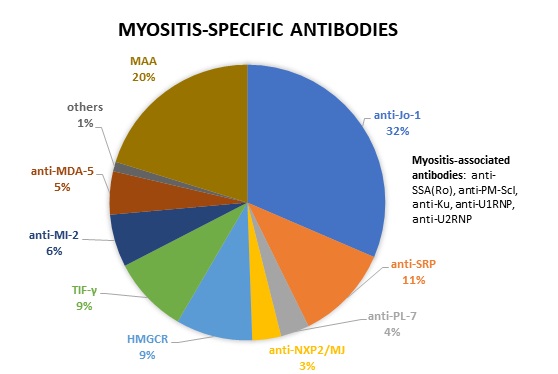
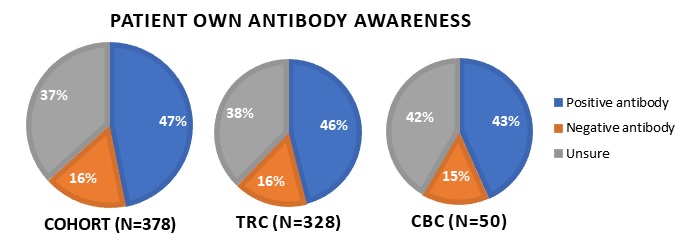
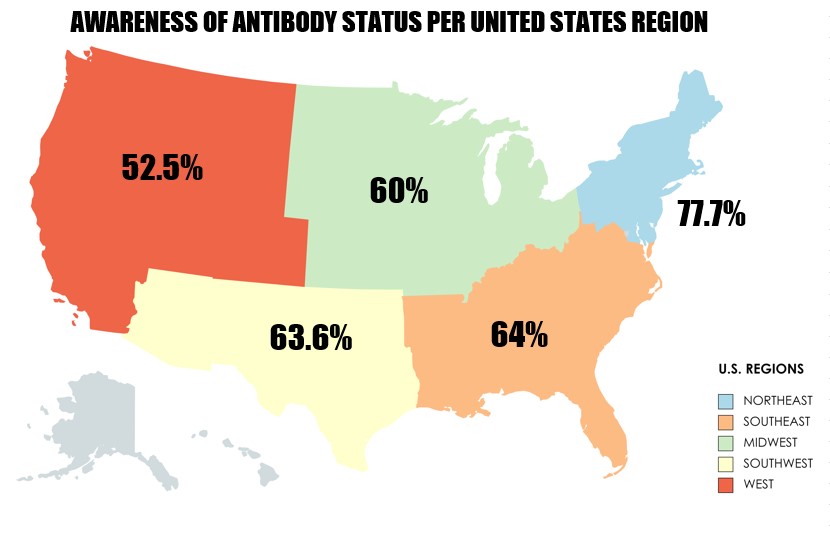
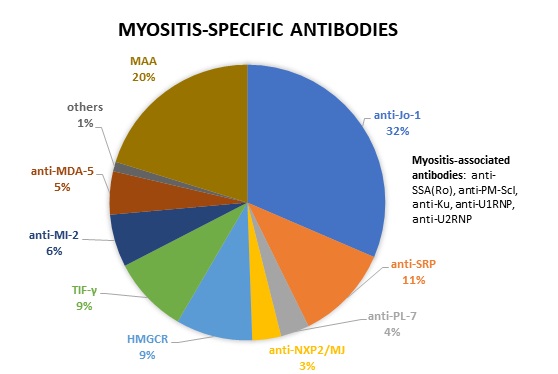
Results: 408 participants completed the pre-screening questionnaire: 317 (77.8%) females, mean age 54.84 (SD +/- 13.8), 378 (92.6%) non-Hispanic, and 328 (80.4%) White, 49 (12%) Black, 13 (3.3%) Asian. Most patients (378, 92.6%) met study IIM criteria. The most common diagnoses were dermatomyositis (195; 51.6%), polymyositis, or necrotizing myopathy (183; 48.4%). A total of 177 (46.8%) reported a positive MSA and/or MAA while 62 (12.4%) were antibody negative and 139 (36.8%) were unsure about their antibody status. The most common MSAs were Jo-1 (31.6%), anti-SRP (11.3%), anti-HMGCR (9%), anti-TIF1-γ (9%), anti-Mi-2 (6.2%), and anti-MDA-5 (5.1%). Regarding MAA, 21 (11.8%) had a positive SSA (Ro), 9 (5.1%) anti-PM-Scl, 3 (1.74%) anti-Ku, and 2 (1.13%) anti-U1RNP. There was no difference in MSA/MAA frequency or distribution by U.S. region or enrollment method (remote vs. from myositis center). Antibody status awareness was significantly higher in the Northeast compared to other regions. Age, gender, ethnicity, and race were not associated with antibody knowledge. There was no difference in antibody awareness between enrollment methods. In a subset of patients (n=94), antibody self-report was highly consistent with physician chart-confirmed MSA/MAA positivity (96.4%) and overall negative or positive status (91.5%).
Conclusion: In a large national real-world IIM cohort, anti-Jo1, -SRP, -HMGCR, -TIF1-γ, -Mi-2, -MDA-5, -SSA, - PM-Scl were the most common MSA/MAA reported by patients. One-third of patients were unaware of their antibody status. There was no difference in antibody frequency, distribution, or awareness by patients enrolled remotely vs. by expert centers. Patients enrolled from the Northeast had significantly more autoantibody awareness. No demographic differences were seen. Patient awareness of their disease and key test results is crucial, as they are important allies in healthcare decision-making.
R. Lomanto Silva: None; s. keret: None; A. Sharma: None; T. Chandra: None; S. Moghadam-Kia: None; C. V. Oddis: Boehringer-Ingelheim, 5, Cabaletta, 5, EMD Serono, 5, Novartis, 5, Pfizer, 1; R. Aggarwal: Actigraph, 2, Alexion, 2, ANI Pharmaceuticals, 2, Argenx, 2, AstraZeneca, 2, Boehringer-Ingelheim, 2, 5, Bristol-Myers Squibb(BMS), 2, 5, CabalettaBio, 2, Capella Bioscience, 2, Corbus, 2, CSL Behring, 2, EMD Serono, 2, 5, Galapagos, 2, Horizon Therapeutics, 2, I-Cell, 2, Janssen, 2, 5, Kezar, 2, Kyverna, 2, Mallinckrodt, 5, Merck, 2, Octapharma, 2, Pfizer, 2, 5, Q32, 5, Roivant, 2, Sanofi, 2, Teva, 2.
Background/Purpose: Myositis-specific antibodies (MSA) represent unique phenotypes in idiopathic inflammatory myopathies (IIM). Myositis-associated antibodies (MAA) most commonly occur in IIM overlap syndromes. MSA and MAA should be assessed in all IIM patients, but their real-world frequency, distribution, and patient awareness are not well known. Given the increasing importance of MSA/MAA in IIM diagnosis and management, we examined their real-world vs. expert-center frequency, awareness, and distribution.
Methods: Myositis Patient-Centered Tele-Research is a multi-center observational study. Patients were enrolled remotely from anywhere in the U.S. through social media and patient organizations (Tele-Research Cohort, TRC) and traditionally through myositis centers (Center-Based Cohort, CBC). Patients completed a pre-screening questionnaire with MSA/MAA and IIM self-report, the latter being confirmed by a rheumatologist, neurologist, or dermatologist. Patients also self-reported on study disease criteria: proximal muscle weakness, muscle or skin biopsy, electromyography, muscle enzyme, and/or dermatomyositis rashes. A subset of patients had their clinical features, diagnosis, and MSA/MAA results confirmed by physician chart review.
Results: 408 participants completed the pre-screening questionnaire: 317 (77.8%) females, mean age 54.84 (SD +/- 13.8), 378 (92.6%) non-Hispanic, and 328 (80.4%) White, 49 (12%) Black, 13 (3.3%) Asian. Most patients (378, 92.6%) met study IIM criteria. The most common diagnoses were dermatomyositis (195; 51.6%), polymyositis, or necrotizing myopathy (183; 48.4%). A total of 177 (46.8%) reported a positive MSA and/or MAA while 62 (12.4%) were antibody negative and 139 (36.8%) were unsure about their antibody status. The most common MSAs were Jo-1 (31.6%), anti-SRP (11.3%), anti-HMGCR (9%), anti-TIF1-γ (9%), anti-Mi-2 (6.2%), and anti-MDA-5 (5.1%). Regarding MAA, 21 (11.8%) had a positive SSA (Ro), 9 (5.1%) anti-PM-Scl, 3 (1.74%) anti-Ku, and 2 (1.13%) anti-U1RNP. There was no difference in MSA/MAA frequency or distribution by U.S. region or enrollment method (remote vs. from myositis center). Antibody status awareness was significantly higher in the Northeast compared to other regions. Age, gender, ethnicity, and race were not associated with antibody knowledge. There was no difference in antibody awareness between enrollment methods. In a subset of patients (n=94), antibody self-report was highly consistent with physician chart-confirmed MSA/MAA positivity (96.4%) and overall negative or positive status (91.5%).
Conclusion: In a large national real-world IIM cohort, anti-Jo1, -SRP, -HMGCR, -TIF1-γ, -Mi-2, -MDA-5, -SSA, - PM-Scl were the most common MSA/MAA reported by patients. One-third of patients were unaware of their antibody status. There was no difference in antibody frequency, distribution, or awareness by patients enrolled remotely vs. by expert centers. Patients enrolled from the Northeast had significantly more autoantibody awareness. No demographic differences were seen. Patient awareness of their disease and key test results is crucial, as they are important allies in healthcare decision-making.
R. Lomanto Silva: None; s. keret: None; A. Sharma: None; T. Chandra: None; S. Moghadam-Kia: None; C. V. Oddis: Boehringer-Ingelheim, 5, Cabaletta, 5, EMD Serono, 5, Novartis, 5, Pfizer, 1; R. Aggarwal: Actigraph, 2, Alexion, 2, ANI Pharmaceuticals, 2, Argenx, 2, AstraZeneca, 2, Boehringer-Ingelheim, 2, 5, Bristol-Myers Squibb(BMS), 2, 5, CabalettaBio, 2, Capella Bioscience, 2, Corbus, 2, CSL Behring, 2, EMD Serono, 2, 5, Galapagos, 2, Horizon Therapeutics, 2, I-Cell, 2, Janssen, 2, 5, Kezar, 2, Kyverna, 2, Mallinckrodt, 5, Merck, 2, Octapharma, 2, Pfizer, 2, 5, Q32, 5, Roivant, 2, Sanofi, 2, Teva, 2.



