Poster Session B
Vasculitis
Session: (1534–1553) Vasculitis – ANCA-Associated Poster II: Epidemiology, Outcomes, & Classification
1542: The Burden of Multimorbidity in ANCA-Associated Vasculitis: A Cohort Study
Monday, November 13, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- ZW
Zachary Wallace, MD, MSc
Massachusetts General Hospital
Newton, MA, United StatesDisclosure(s): No relevant disclosure to display
Abstract Poster Presenter(s)
Zachary Wallace1, Xiaoqing Fu2, Shruthi Srivatsan2, Zachary Williams2, Claire Cook2, Jennifer Hanberg2, John Stone3, Hyon K. Choi4 and Yuqing Zhang5, 1Massachusetts General Hospital, Newton, MA, 2Massachusetts General Hospital, Boston, MA, 3Massachusetts General Hospital Rheumatology Unit, Harvard Medical School, Concord, MA, 4Massachusetts General Hospital and Harvard Medical School, Lexington, MA, 5Division of Rheumatology, Allergy, and Immunology, Department of Medicine, Massachusetts General Hospital, Boston, MA
Background/Purpose: With improvements in the risks of relapse and mortality in ANCA-associated vasculitis (AAV), a better understanding of disease- and treatment-related complications is necessary to optimize outcomes and personalize care. Multimorbidity (MM) is a patient-centered approach to measuring complications and is associated with risk of death and quality of life in other conditions. It is defined as having multiple chronic conditions but remains poorly understood in AAV. We sought to determine the burden of multimorbidity in AAV.
Methods: We used the 2002-2019 Mass General Brigham (MGB) AAV cohort: an inception cohort of consecutive MPO- or PR3-ANCA+ incident AAV cases at a multi-center healthcare system. Up to 10 comparators without systemic rheumatic disease were identified from MGB and matched to each case by encounter date, age, sex, and race. We adapted a definition of MM as the presence of ≥ 2 of 37 chronic conditions, identified by use of ICD-9/10 codes. Manifestations of AAV (e.g., kidney disease) were excluded from this definition. Pre-existing comorbidities were excluded. We determined the proportion of cases and comparators with MM using the Aalen-Johansen method, accounting for the competing risks of death and loss to follow up. We used Cox proportional hazard models to estimate the risk of MM in cases vs comparators and restricted mean survival time to estimate days free of MM. Among patients with AAV, we used latent class analysis to characterize clusters of morbidity among people with MM and time-varying multivariable-adjusted Cox proportional hazards models to assess the association of MM with mortality risk.
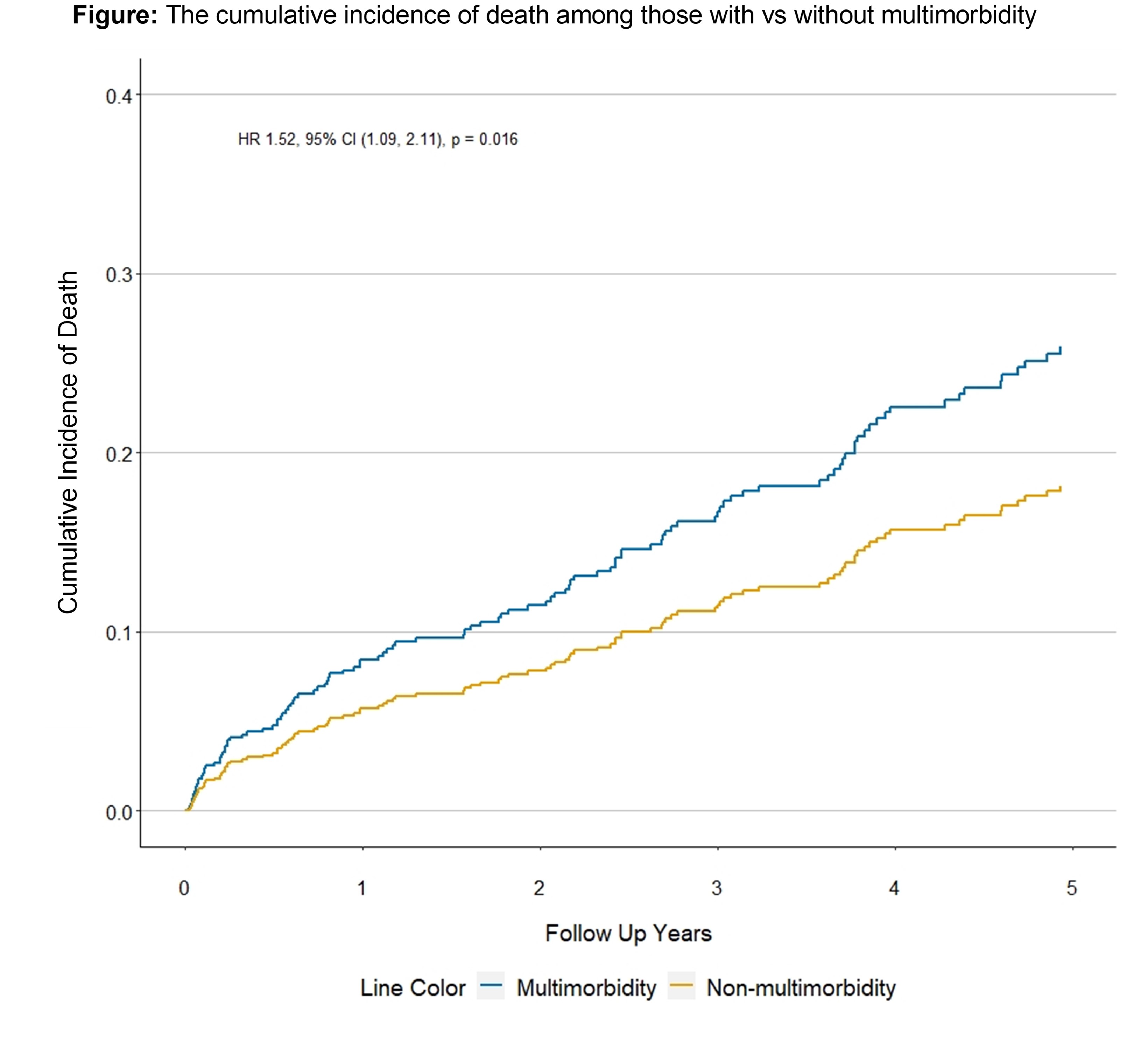
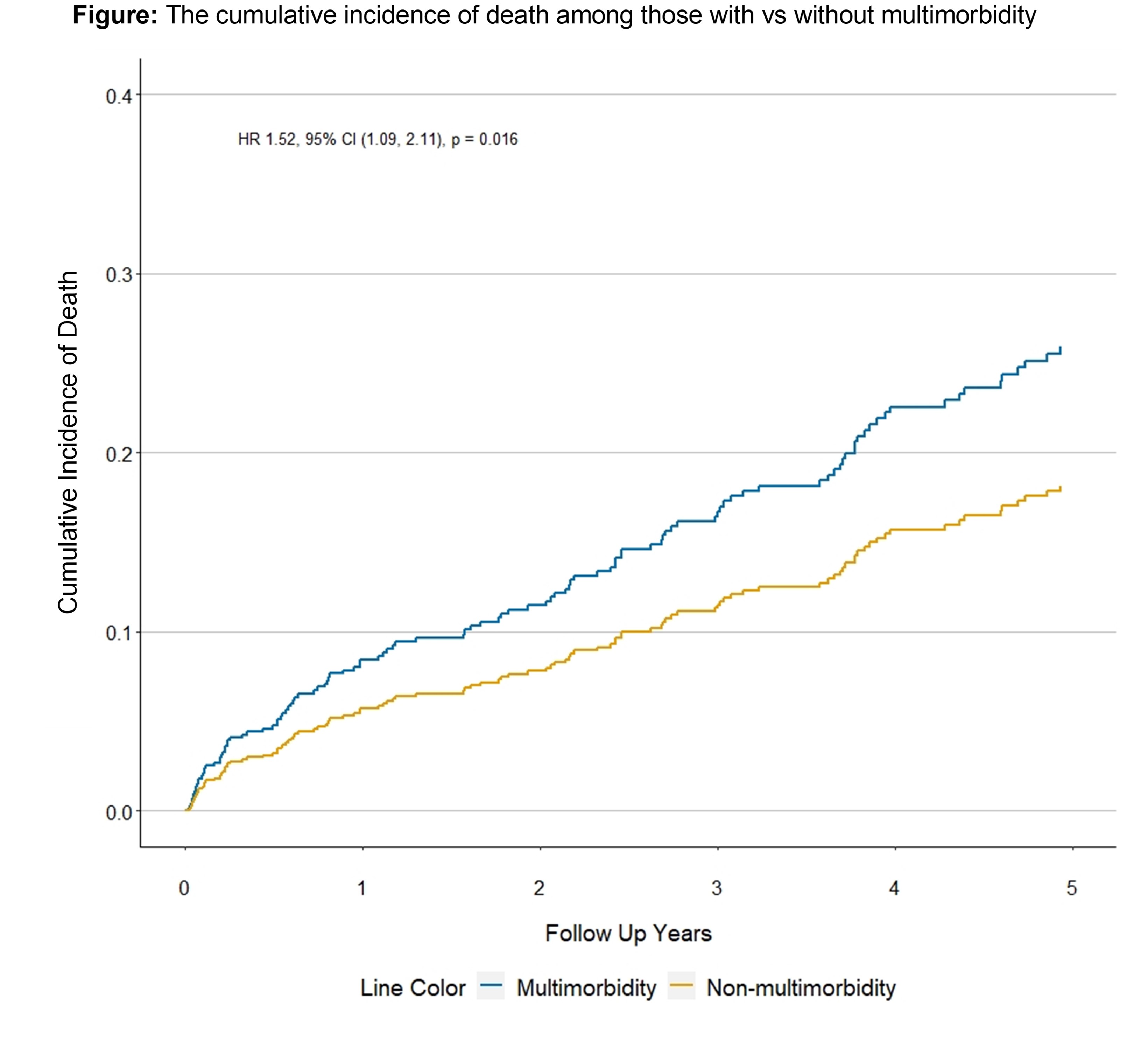
Results: There were 547 cases matched to 5,259 comparators (Table 1). AAV cases had nearly an 8-fold higher risk of MM vs comparators (Table 2, aHR 7.6, 95% CI 6.6-8.7). Over 5 years, each case had an average of 707 fewer days with MM than comparators (963.4 vs 1670.5 days, p< 0.001). At 1 year, two clusters of MM in AAV were identified: Clusters 1A (76%) and 1B (24%). Hypertension and hyperlipidemia were common in Cluster 1A; Cluster 1B was characterized by painful conditions (e.g., headache, back pain, GERD). At 2 years, two clusters were identified: Clusters 2A (82%) and 2B (18%). Cluster 2B was distinguished from 2A by a high burden of cardiovascular (CV) and pulmonary disease. At 5 years, three clusters were identified: Cluster 5A (81%), 5B (11%), and 5C (8%). Morbidities most common in Cluster 5A were hypertension and hyperlipidemia. Cluster 5B was distinguished by a high burden of CV and pulmonary disease; 5C had a high burden of glucocorticoid toxicities (e.g., osteoporosis, obesity, hypertension). Among AAV patients, developing MM is associated with a 52% higher risk of death than not having MM (Figure, age-, sex-, race-, and creatinine-adjusted HR 1.52, 95% CI 1.09-2.11).
Conclusion: AAV is associated with a high burden of MM and greater risk of MM than the general population. MM in AAV is characterized by clusters defined by morbidity burdens that vary over disease course and reflect a high impact of disease and its treatment. MM in AAV is associated with mortality risk. The development of interventions to prevent MM and minimize its impacts are needed.
.jpg)
.jpg)
Z. Wallace: BioCryst, 2, Bristol-Myers Squibb(BMS), 5, Horizon, 1, 2, 5, MedPace, 2, Novartis, 1, PPD, 2, Sanofi, 1, 5, Shionogi, 1, Visterra, 1, 2, Zenas, 1, 2; X. Fu: None; S. Srivatsan: None; Z. Williams: None; C. Cook: None; J. Hanberg: None; J. Stone: Abvie, 2, Amgen, 1, 2, Argenx, 2, Aztrazeneca, 2, Bristol Myers Squibb, 2, 5, Celgene, 2, Chemocentryx, 2, Chugai, 2, GSK, 2, Horizon Therapeutics, 1, 2, 5, InflaRx, 2, IQVIA, 1, 2, Kyverna, 2, Mirabio, 2, NIH, 5, Novartis, 2, PPD, 2, Prometheus, 2, Q32, 2, Regeneron, 2, Roche-Genentech, 2, Roivant, 2, Sanofi, 2, 5, Spruce Biosciences, 2, Star Therapeutics, 2, Steritas, 12, Chair, Scientific Advisory Board (no fiduciary responsibilities), ZenasBio, 2; H. Choi: Ani, 2, Horizon, 2, 5, LG, 2, Protalix, 2, Shanton, 2; Y. Zhang: None.
Background/Purpose: With improvements in the risks of relapse and mortality in ANCA-associated vasculitis (AAV), a better understanding of disease- and treatment-related complications is necessary to optimize outcomes and personalize care. Multimorbidity (MM) is a patient-centered approach to measuring complications and is associated with risk of death and quality of life in other conditions. It is defined as having multiple chronic conditions but remains poorly understood in AAV. We sought to determine the burden of multimorbidity in AAV.
Methods: We used the 2002-2019 Mass General Brigham (MGB) AAV cohort: an inception cohort of consecutive MPO- or PR3-ANCA+ incident AAV cases at a multi-center healthcare system. Up to 10 comparators without systemic rheumatic disease were identified from MGB and matched to each case by encounter date, age, sex, and race. We adapted a definition of MM as the presence of ≥ 2 of 37 chronic conditions, identified by use of ICD-9/10 codes. Manifestations of AAV (e.g., kidney disease) were excluded from this definition. Pre-existing comorbidities were excluded. We determined the proportion of cases and comparators with MM using the Aalen-Johansen method, accounting for the competing risks of death and loss to follow up. We used Cox proportional hazard models to estimate the risk of MM in cases vs comparators and restricted mean survival time to estimate days free of MM. Among patients with AAV, we used latent class analysis to characterize clusters of morbidity among people with MM and time-varying multivariable-adjusted Cox proportional hazards models to assess the association of MM with mortality risk.
Results: There were 547 cases matched to 5,259 comparators (Table 1). AAV cases had nearly an 8-fold higher risk of MM vs comparators (Table 2, aHR 7.6, 95% CI 6.6-8.7). Over 5 years, each case had an average of 707 fewer days with MM than comparators (963.4 vs 1670.5 days, p< 0.001). At 1 year, two clusters of MM in AAV were identified: Clusters 1A (76%) and 1B (24%). Hypertension and hyperlipidemia were common in Cluster 1A; Cluster 1B was characterized by painful conditions (e.g., headache, back pain, GERD). At 2 years, two clusters were identified: Clusters 2A (82%) and 2B (18%). Cluster 2B was distinguished from 2A by a high burden of cardiovascular (CV) and pulmonary disease. At 5 years, three clusters were identified: Cluster 5A (81%), 5B (11%), and 5C (8%). Morbidities most common in Cluster 5A were hypertension and hyperlipidemia. Cluster 5B was distinguished by a high burden of CV and pulmonary disease; 5C had a high burden of glucocorticoid toxicities (e.g., osteoporosis, obesity, hypertension). Among AAV patients, developing MM is associated with a 52% higher risk of death than not having MM (Figure, age-, sex-, race-, and creatinine-adjusted HR 1.52, 95% CI 1.09-2.11).
Conclusion: AAV is associated with a high burden of MM and greater risk of MM than the general population. MM in AAV is characterized by clusters defined by morbidity burdens that vary over disease course and reflect a high impact of disease and its treatment. MM in AAV is associated with mortality risk. The development of interventions to prevent MM and minimize its impacts are needed.
.jpg)
.jpg)
Z. Wallace: BioCryst, 2, Bristol-Myers Squibb(BMS), 5, Horizon, 1, 2, 5, MedPace, 2, Novartis, 1, PPD, 2, Sanofi, 1, 5, Shionogi, 1, Visterra, 1, 2, Zenas, 1, 2; X. Fu: None; S. Srivatsan: None; Z. Williams: None; C. Cook: None; J. Hanberg: None; J. Stone: Abvie, 2, Amgen, 1, 2, Argenx, 2, Aztrazeneca, 2, Bristol Myers Squibb, 2, 5, Celgene, 2, Chemocentryx, 2, Chugai, 2, GSK, 2, Horizon Therapeutics, 1, 2, 5, InflaRx, 2, IQVIA, 1, 2, Kyverna, 2, Mirabio, 2, NIH, 5, Novartis, 2, PPD, 2, Prometheus, 2, Q32, 2, Regeneron, 2, Roche-Genentech, 2, Roivant, 2, Sanofi, 2, 5, Spruce Biosciences, 2, Star Therapeutics, 2, Steritas, 12, Chair, Scientific Advisory Board (no fiduciary responsibilities), ZenasBio, 2; H. Choi: Ani, 2, Horizon, 2, 5, LG, 2, Protalix, 2, Shanton, 2; Y. Zhang: None.



