Poster Session A
Rheumatoid arthritis (RA)
Session: (0423–0459) RA – Treatment Poster I
0453: Risk of Lung Cancer in Veterans with Rheumatoid Arthritis in Relation to Use of Conventional versus Biologic or Targeted Synthetic DMARDs
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- NS
Namrata Singh, MD, MSc
University of Washington
Bellevue, WA, United StatesDisclosure(s): Pfizer: Advisor or Review Panel Member (Terminated, April 29, 2022)
Abstract Poster Presenter(s)
Namrata Singh1, Alexander Peterson2, Aaron Baraff2, K Wysham3, Bryant England4, Joshua Baker5, Nicholas Smith2, Ted R Mikuls6 and Noel Weiss7, 1University of Washington, Bellevue, WA, 2VA Puget Sound Seattle, Seattle, WA, 3VA Puget Sound/University of Washington, Seattle, WA, 4University of Nebraska Medical Center, Omaha, NE, 5University of Pennsylvania, Philadelphia, PA, 6Division of Rheumatology and Immunology, University of Nebraska Medical Center, Omaha, NE, 7University of Washington, Seattle, WA
Background/Purpose: Rheumatoid arthritis (RA) is associated with an increased risk of lung cancer compared to the general population. While smoking is a shared risk factor, little is known about the association between use of disease modifying anti-rheumatic drugs (DMARDs) and development of lung cancer. We undertook this study to evaluate the association between use of conventional synthetic (cs) versus biologic (b) or targeted synthetic (ts) DMARDs and incident lung cancer in patients with RA.
Methods: In this retrospective cohort study, we identified Veterans diagnosed with RA in any United States Veterans Affairs facility from 1/1/2002 and 12/31/2018. Criteria for the presence of RA were: two or more International Classification of Diseases Version 9 or 10 (ICD9 or ICD10) diagnosis codes for RA at least 7 days apart but no more than 365 days apart, and a prescription for a csDMARD within 90 days of the first RA diagnosis (index date). The csDMARDs included in these analyses were: methotrexate, sulfasalazine, leflunomide, and hydroxychloroquine. The bDMARDs included were tumor necrosis factor inhibitors (TNFi) and non-TNFi biologics such as tocilizumab, rituximab, abatacept, and biosimilars; tsDMARDs included tofacitinib and baricitinib. Patients with lung cancer before the diagnosis of RA were excluded. Incident lung cancer was determined by ³2 outpatient ICD9/10 codes, or ³1 ICD9/ICD10/ICDO codes if from inpatient or the oncology raw domain. Drug exposure categories (csDMARD versus b/tsDMARD) were treated as a time-varying variable. Multivariable Cox models were fit to estimate the hazard ratio for developing lung cancer during and following the use of a b/tsDMARD relative to b/tsDMARD-naïve persons adjusting for time-varying age, rheumatic disease comorbidity index (RDCI) and RA interstitial lung disease (RA-ILD, identified using validated administrative algorithms(1)); and baseline sex, race, ethnicity, smoking status, body mass index (BMI), cohort entry (2002-2007, 2008-2013, 2014-2019), rheumatoid factor or anti-CCP positivity, use of opioids, NSAIDs, and steroids. Missing data were imputed using multiple imputation by chained equations.
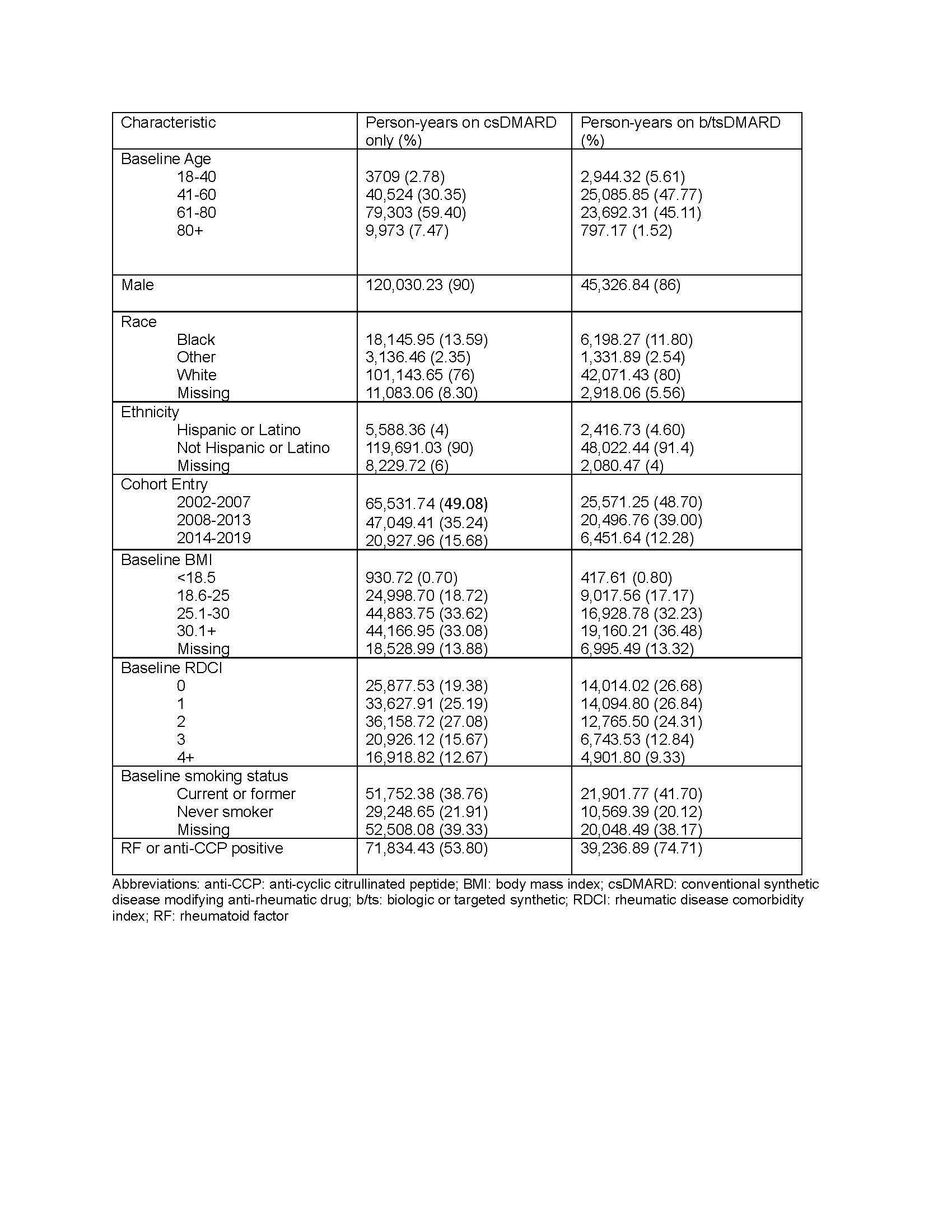
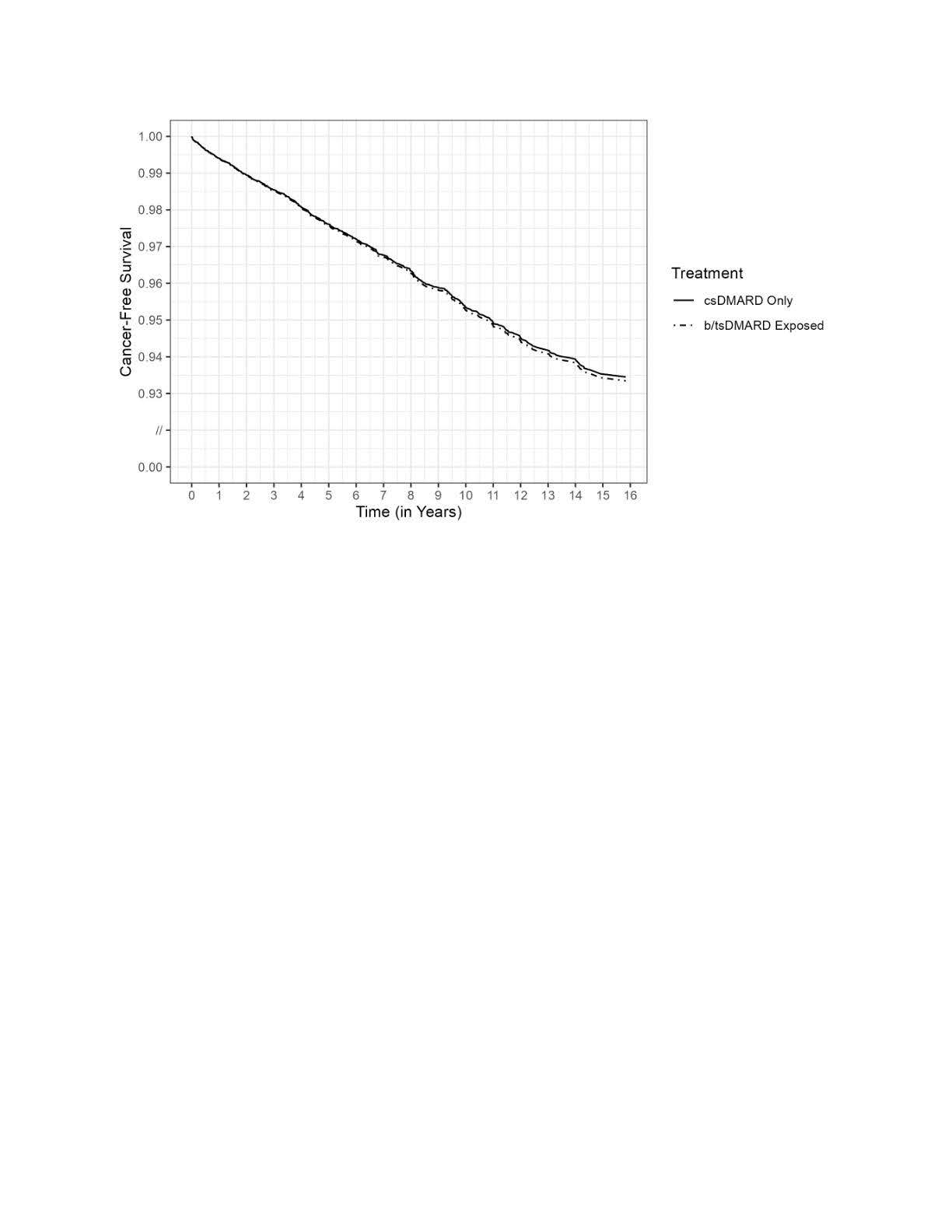
Results: 26,625 veterans met eligibility criteria, of whom 89% were male and 71% were Non-Hispanic White (Table 1). Over a mean (±standard deviation) follow up of 7.0 (±4.5) years, 852 incident lung cancers were detected. The age-standardized incidence among those only on csDMARDs was 4.56 per 1000-person years, compared to 5.33 for those exposed to b/tsDMARDs. In multivariable adjusted models, the hazard ratio for lung cancer in persons who had been treated with a b/tsDMARD was 1.03 (95% confidence interval (CI) 0.87-1.21) relative to those only on csDMARDs (Figure 1).
Conclusion: Among Veterans with RA, we observed no evidence of an altered risk of lung cancer associated with different forms of RA treatment. However, incomplete information on cigarette smoking history, along with the relatively short period of follow-up, limit any conclusions that might be drawn.
Reference:
1. England BR, et al. Performance of Administrative Algorithms to Identify Interstitial Lung Disease in Rheumatoid Arthritis. AC&R 2020
N. Singh: None; A. Peterson: None; A. Baraff: None; K. Wysham: None; B. England: Boehringer-Ingelheim, 2, 5; J. Baker: CorEvitas, 2, Cumberland Pharma, 2, Horizon Pharmaceuticals, 5; N. Smith: None; T. Mikuls: Elsevier, 9, Horizon Therapeutics, 2, 5, Pfizer, 2, Sanofi, 2, UCB Pharma, 2, Wolters Kluwer Health (UpToDate), 9; N. Weiss: None.
Background/Purpose: Rheumatoid arthritis (RA) is associated with an increased risk of lung cancer compared to the general population. While smoking is a shared risk factor, little is known about the association between use of disease modifying anti-rheumatic drugs (DMARDs) and development of lung cancer. We undertook this study to evaluate the association between use of conventional synthetic (cs) versus biologic (b) or targeted synthetic (ts) DMARDs and incident lung cancer in patients with RA.
Methods: In this retrospective cohort study, we identified Veterans diagnosed with RA in any United States Veterans Affairs facility from 1/1/2002 and 12/31/2018. Criteria for the presence of RA were: two or more International Classification of Diseases Version 9 or 10 (ICD9 or ICD10) diagnosis codes for RA at least 7 days apart but no more than 365 days apart, and a prescription for a csDMARD within 90 days of the first RA diagnosis (index date). The csDMARDs included in these analyses were: methotrexate, sulfasalazine, leflunomide, and hydroxychloroquine. The bDMARDs included were tumor necrosis factor inhibitors (TNFi) and non-TNFi biologics such as tocilizumab, rituximab, abatacept, and biosimilars; tsDMARDs included tofacitinib and baricitinib. Patients with lung cancer before the diagnosis of RA were excluded. Incident lung cancer was determined by ³2 outpatient ICD9/10 codes, or ³1 ICD9/ICD10/ICDO codes if from inpatient or the oncology raw domain. Drug exposure categories (csDMARD versus b/tsDMARD) were treated as a time-varying variable. Multivariable Cox models were fit to estimate the hazard ratio for developing lung cancer during and following the use of a b/tsDMARD relative to b/tsDMARD-naïve persons adjusting for time-varying age, rheumatic disease comorbidity index (RDCI) and RA interstitial lung disease (RA-ILD, identified using validated administrative algorithms(1)); and baseline sex, race, ethnicity, smoking status, body mass index (BMI), cohort entry (2002-2007, 2008-2013, 2014-2019), rheumatoid factor or anti-CCP positivity, use of opioids, NSAIDs, and steroids. Missing data were imputed using multiple imputation by chained equations.
Results: 26,625 veterans met eligibility criteria, of whom 89% were male and 71% were Non-Hispanic White (Table 1). Over a mean (±standard deviation) follow up of 7.0 (±4.5) years, 852 incident lung cancers were detected. The age-standardized incidence among those only on csDMARDs was 4.56 per 1000-person years, compared to 5.33 for those exposed to b/tsDMARDs. In multivariable adjusted models, the hazard ratio for lung cancer in persons who had been treated with a b/tsDMARD was 1.03 (95% confidence interval (CI) 0.87-1.21) relative to those only on csDMARDs (Figure 1).
Conclusion: Among Veterans with RA, we observed no evidence of an altered risk of lung cancer associated with different forms of RA treatment. However, incomplete information on cigarette smoking history, along with the relatively short period of follow-up, limit any conclusions that might be drawn.
Reference:
1. England BR, et al. Performance of Administrative Algorithms to Identify Interstitial Lung Disease in Rheumatoid Arthritis. AC&R 2020
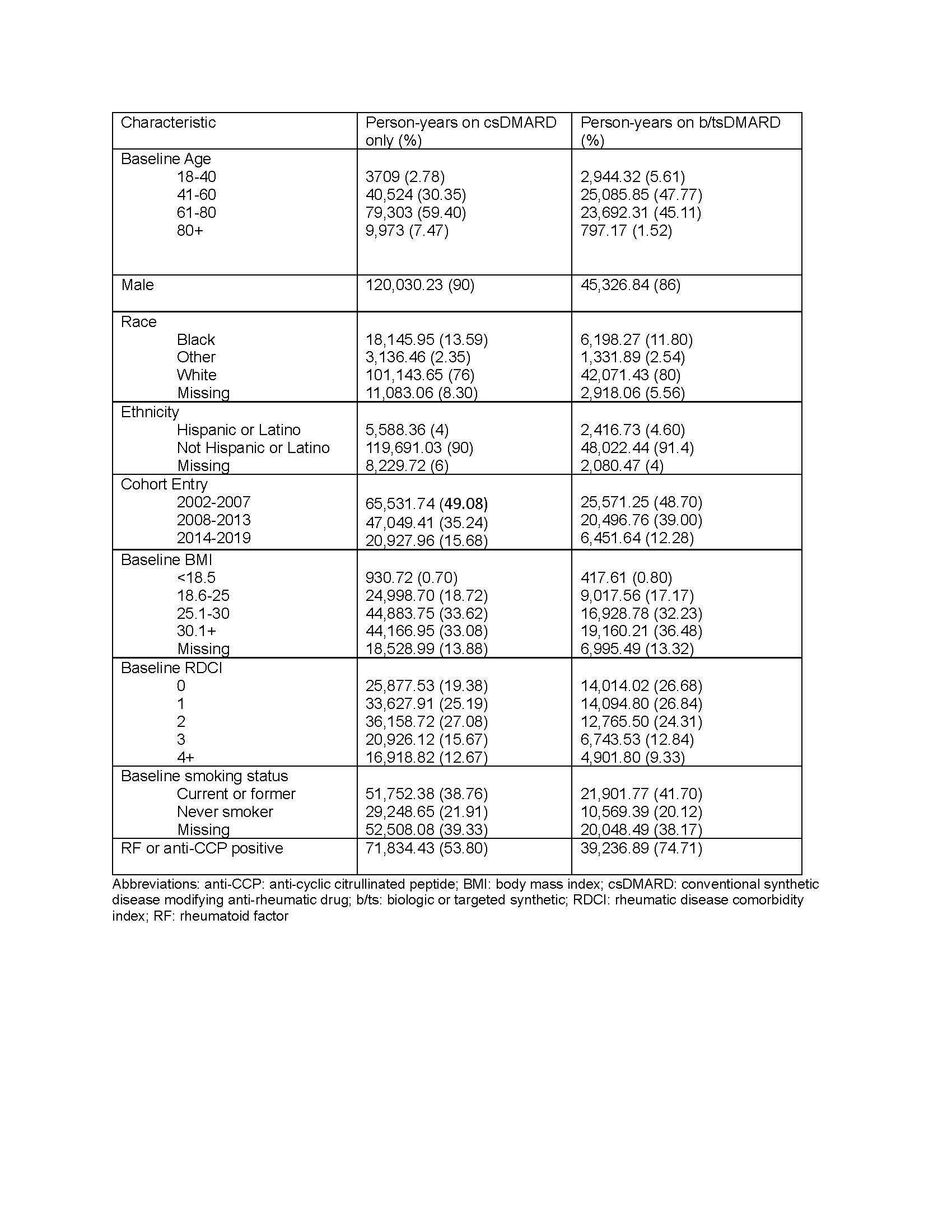
Table 1. Characteristics of the cohort in person-years by DMARD exposure
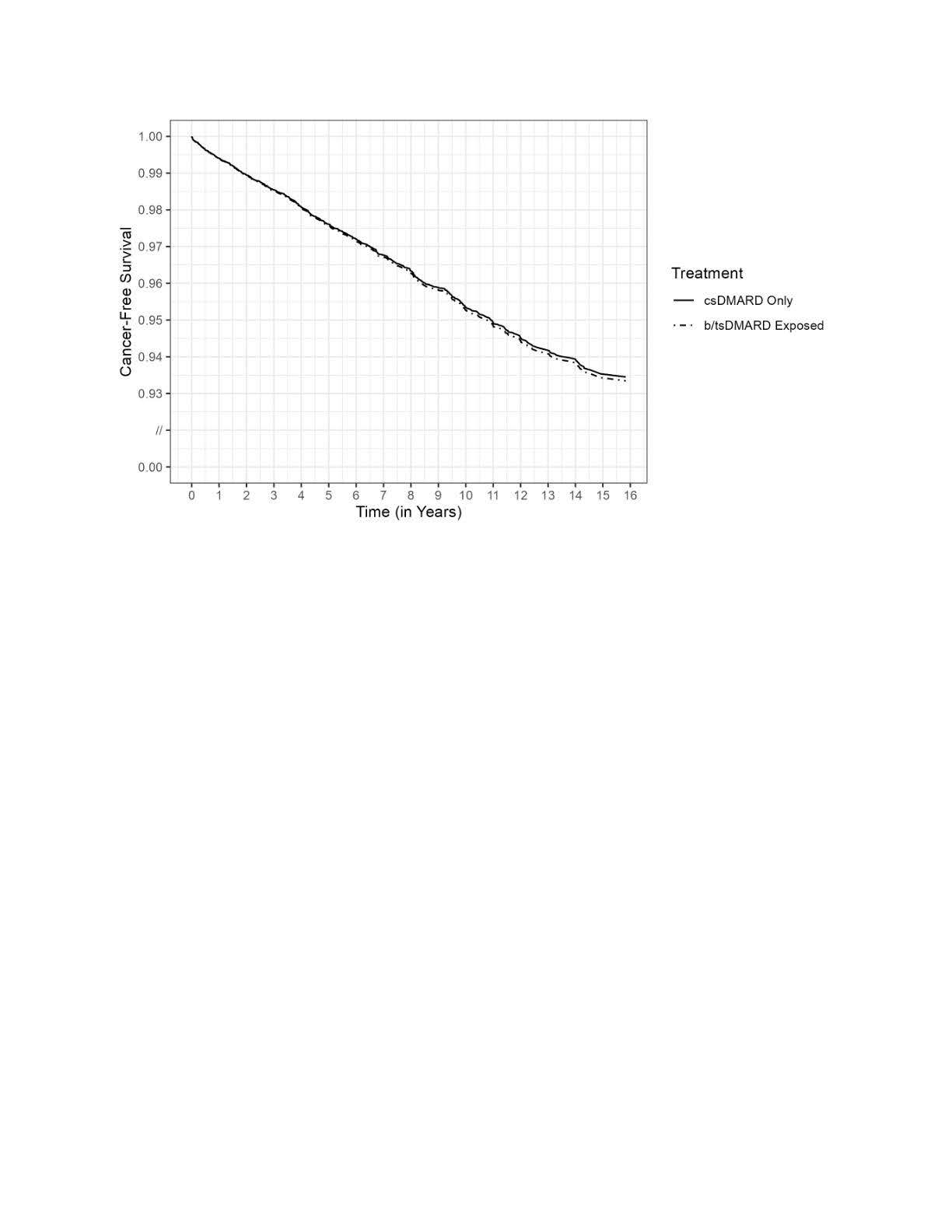
Figure 1. Kaplan Meier curves showing association between use of disease modifying anti-rheumatic drugs and lung cancer.
N. Singh: None; A. Peterson: None; A. Baraff: None; K. Wysham: None; B. England: Boehringer-Ingelheim, 2, 5; J. Baker: CorEvitas, 2, Cumberland Pharma, 2, Horizon Pharmaceuticals, 5; N. Smith: None; T. Mikuls: Elsevier, 9, Horizon Therapeutics, 2, 5, Pfizer, 2, Sanofi, 2, UCB Pharma, 2, Wolters Kluwer Health (UpToDate), 9; N. Weiss: None.



