Abstract Session
Systemic lupus erythematosus (SLE)
Session: Abstracts: SLE – Diagnosis, Manifestations, & Outcomes IV: Outcomes & Comorbidity (2587–2592)
2592: Trends, Sociodemographic and Clinical Factors Associated with Avascular Necrosis and Related Arthroplasties in Hospitalized Patients with Systemic Lupus Erythematosus and Rheumatoid Arthritis
Wednesday, November 15, 2023
12:15 PM - 12:25 PM PT
Location: Room 25A-C
- RD
Rashmi Dhital, MD
UC San Diego
San Diego, CA, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Presenting Author(s)
Rashmi Dhital1, Neha Singh2, Brian Pedersen2 and Christie M. Bartels3, 1UC San Diego, San Diego, CA, 2University of California San Diego, San Diego, CA, 3University of Wisconsin, School of Medicine and Public Health, Madison, WI
Background/Purpose: Avascular necrosis (AVN) can be a debilitating complication of autoimmune diseases and steroid treatment, with a higher prevalence in systemic lupus erythematosus (SLE) (0.8-33%) compared to rheumatoid arthritis (RA) (0.4%-12). AVN frequently leads to progressive joint destruction necessitating arthroplasty. Limited research exists on trends following the introduction of newer steroid-sparing agents as well as sociodemographic and clinical factors associated with AVN. We aimed to analyze rates, trends, and characteristics associated with AVN and AVN-related joint arthroplasties among SLE and RA hospitalizations using the largest publicly available all-payer inpatient US database, the National Inpatient Sample (NIS).
Methods: This cross-sectional study used NIS data (2000-2019) to identify hospitalized adults (≥18 years) with diagnoses of SLE and RA, and those with concomitant AVN diagnoses using validated International Classification of Disease (ICD) codes. AVN was further grouped into whether or not they had arthroplasties to examine trends. We compared SLE and RA hospitalizations with and without AVN, and arthroplasties using STATA and the Joinpoint regression program to calculate annual percent change (APC).
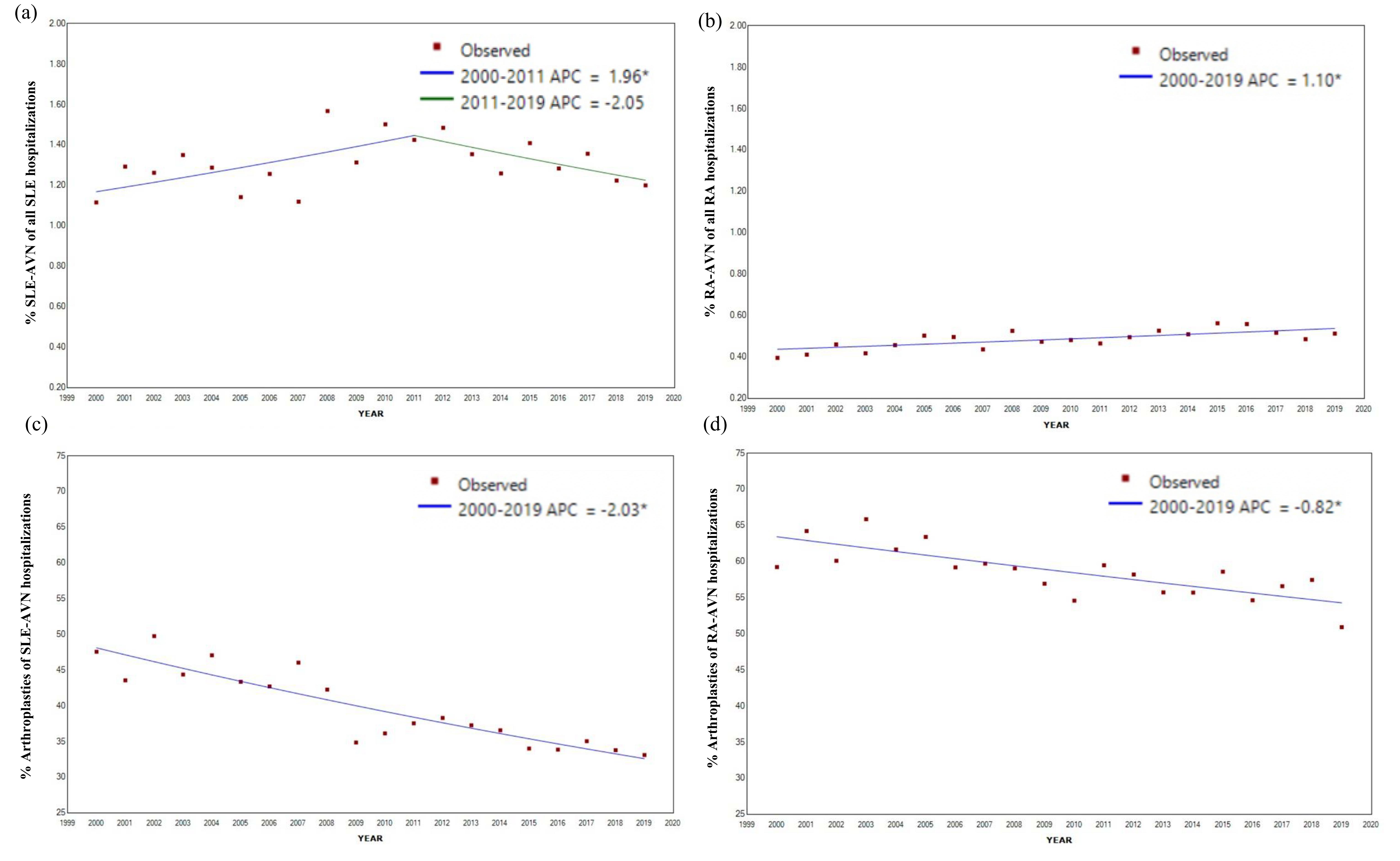
Results: From 2000-2019, there were 3,295,384 SLE and 8,983,521 RA hospitalizations, among which 43,339 (1.3%) and 44,148 (0.5%) had concomitant AVN (herein referred to as SLE-AVN and RA-AVN, respectively; Table 1). Of the SLE-AVN and RA-AVN, 16,941 (39%) and 25,509 (57%) underwent arthroplasties, respectively (Table 1, Figure 1). We observed an uptrend in RA-AVN (APC: 1.10*), with a decrease in the proportions of arthroplasties (APC: -0.82*; Figure 2). In contrast, there was an initial increase followed by a tendency to decline in SLE-AVN (APC 2000-2011: 1.96* APC 2011-2019 -2.05), with a decrease in the proportion of arthroplasties over time (APC -2.03*, Figure 2). Hospitalizations with AVN were younger [SLE (mean age: 43 vs 52 without), RA (mean age: 60 vs 68 without)] and more often Black race [SLE (41% Black with AVN, 26% without), RA (17% with AVN vs 10% without); Table 1]. SLE-AVN patients had higher rates of antiphospholipid syndrome (5% vs 3%) and end-stage renal disease (11% vs 9%); RA-AVN patients had higher nicotine use (15% vs 12%) compared to those without AVN. Among SLE-AVN and RA-AVN, encounters with arthroplasty (Table 1) were less likely to be Black (34% vs 46% in SLE-AVN and 13% vs 23% in RA-AVN) or have Medicaid coverage (15% vs 24% for SLE-AVN, and 9% vs 15% for RA-AVN) or most comorbidities than those without.
Conclusion: We report an initial increasing trend of SLE-AVN followed by a tendency to decline, which may relate to newer steroid-sparing therapies (i.e., Belimumab approval in 2011). There was an overall declining trend of AVN-associated arthroplasties in both SLE and RA. AVN hospitalizations were more likely to be younger and of the Black race. Yet, arthroplasty was less likely in encounters with patients who were Black or had Medicaid coverage. Our data indicate potential healthcare disparities that may influence surgical access. Further research should examine sociodemographic and treatment differences impacting AVN and arthroplasty rates.
.jpg)

R. Dhital: None; N. Singh: None; B. Pedersen: None; C. Bartels: Pfizer, 5.
Background/Purpose: Avascular necrosis (AVN) can be a debilitating complication of autoimmune diseases and steroid treatment, with a higher prevalence in systemic lupus erythematosus (SLE) (0.8-33%) compared to rheumatoid arthritis (RA) (0.4%-12). AVN frequently leads to progressive joint destruction necessitating arthroplasty. Limited research exists on trends following the introduction of newer steroid-sparing agents as well as sociodemographic and clinical factors associated with AVN. We aimed to analyze rates, trends, and characteristics associated with AVN and AVN-related joint arthroplasties among SLE and RA hospitalizations using the largest publicly available all-payer inpatient US database, the National Inpatient Sample (NIS).
Methods: This cross-sectional study used NIS data (2000-2019) to identify hospitalized adults (≥18 years) with diagnoses of SLE and RA, and those with concomitant AVN diagnoses using validated International Classification of Disease (ICD) codes. AVN was further grouped into whether or not they had arthroplasties to examine trends. We compared SLE and RA hospitalizations with and without AVN, and arthroplasties using STATA and the Joinpoint regression program to calculate annual percent change (APC).
Results: From 2000-2019, there were 3,295,384 SLE and 8,983,521 RA hospitalizations, among which 43,339 (1.3%) and 44,148 (0.5%) had concomitant AVN (herein referred to as SLE-AVN and RA-AVN, respectively; Table 1). Of the SLE-AVN and RA-AVN, 16,941 (39%) and 25,509 (57%) underwent arthroplasties, respectively (Table 1, Figure 1). We observed an uptrend in RA-AVN (APC: 1.10*), with a decrease in the proportions of arthroplasties (APC: -0.82*; Figure 2). In contrast, there was an initial increase followed by a tendency to decline in SLE-AVN (APC 2000-2011: 1.96* APC 2011-2019 -2.05), with a decrease in the proportion of arthroplasties over time (APC -2.03*, Figure 2). Hospitalizations with AVN were younger [SLE (mean age: 43 vs 52 without), RA (mean age: 60 vs 68 without)] and more often Black race [SLE (41% Black with AVN, 26% without), RA (17% with AVN vs 10% without); Table 1]. SLE-AVN patients had higher rates of antiphospholipid syndrome (5% vs 3%) and end-stage renal disease (11% vs 9%); RA-AVN patients had higher nicotine use (15% vs 12%) compared to those without AVN. Among SLE-AVN and RA-AVN, encounters with arthroplasty (Table 1) were less likely to be Black (34% vs 46% in SLE-AVN and 13% vs 23% in RA-AVN) or have Medicaid coverage (15% vs 24% for SLE-AVN, and 9% vs 15% for RA-AVN) or most comorbidities than those without.
Conclusion: We report an initial increasing trend of SLE-AVN followed by a tendency to decline, which may relate to newer steroid-sparing therapies (i.e., Belimumab approval in 2011). There was an overall declining trend of AVN-associated arthroplasties in both SLE and RA. AVN hospitalizations were more likely to be younger and of the Black race. Yet, arthroplasty was less likely in encounters with patients who were Black or had Medicaid coverage. Our data indicate potential healthcare disparities that may influence surgical access. Further research should examine sociodemographic and treatment differences impacting AVN and arthroplasty rates.
.jpg)
Comparison of SLE and RA hospitalizations with and without diagnoses of AVN and with and without AVN-associated arthroplasties (hip, knee, shoulder), National Inpatient Sample, 2000-2019
*SLE: systemic lupus erythematosus, RA: rheumatoid arthritis, AVN: avascular necrosis, SEM: standard error of mean
APS: Antiphospholipid syndrome ESRD: End-stage renal disease IHD: Ischemic heart disease PVD: Peripheral vascular disease HF: Heart failure, CMP: cardiomyopathy
Differences in variables between groups are significant with p < 0.05 except for:
SLE without AVN vs SLE with AVN: hypertension;
SLE-AVN without and with arthroplasty: sex, COPD, hyperlipidemia, alcohol-related disorders;
RA without AVN vs RA with AVN: sex, ESRD, alcohol-related disorders;
RA-AVN without and with arthroplasty: sex, hypertension, nicotine dependence
*SLE: systemic lupus erythematosus, RA: rheumatoid arthritis, AVN: avascular necrosis, SEM: standard error of mean
APS: Antiphospholipid syndrome ESRD: End-stage renal disease IHD: Ischemic heart disease PVD: Peripheral vascular disease HF: Heart failure, CMP: cardiomyopathy
Differences in variables between groups are significant with p < 0.05 except for:
SLE without AVN vs SLE with AVN: hypertension;
SLE-AVN without and with arthroplasty: sex, COPD, hyperlipidemia, alcohol-related disorders;
RA without AVN vs RA with AVN: sex, ESRD, alcohol-related disorders;
RA-AVN without and with arthroplasty: sex, hypertension, nicotine dependence

Avascular necrosis (AVN) and related arthroplasties per 100,000 hospitalized adults with systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA), National Inpatient Sample, 2000-2019.
Green represents RA, orange represents SLE, arthroplasties are represented by lighter shading.
Green represents RA, orange represents SLE, arthroplasties are represented by lighter shading.
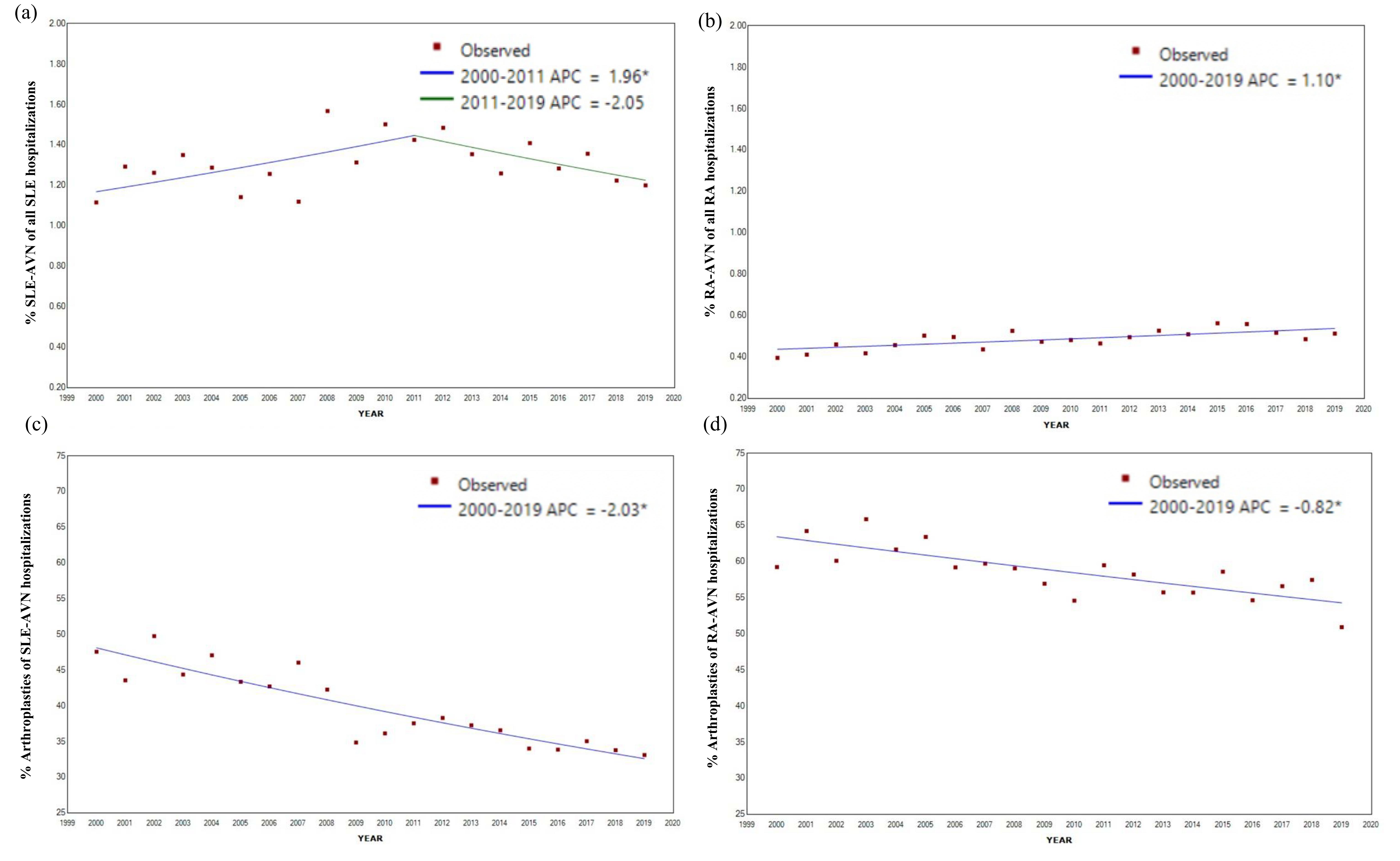
Trends of avascular necrosis (AVN) and AVN-associated arthroplasties among hospitalized adults with systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA), National Inpatient Sample, 2000-2019.
(a) The percentage of AVN among SLE hospitalizations shows an initial significant uptrend (APC 1.96*) with a peak around 2011
(b) The percentage of AVN among RA hospitalizations shows a modest significant uptrend over time (APC 1.10*), however, rates are lower compared to SLE-AVN.
(c) AVN-related arthroplasties in both SLE-AVN (APC -2.03*) and (d) RA-AVN (APC -0.82*) show a significant decline over time.
The rate of change from 2000 to 2019 was calculated using Joinpoint regression software and expressed as Annual Percent Change (APC). *Indicates significant difference at alpha = 0.05 level.
(a) The percentage of AVN among SLE hospitalizations shows an initial significant uptrend (APC 1.96*) with a peak around 2011
(b) The percentage of AVN among RA hospitalizations shows a modest significant uptrend over time (APC 1.10*), however, rates are lower compared to SLE-AVN.
(c) AVN-related arthroplasties in both SLE-AVN (APC -2.03*) and (d) RA-AVN (APC -0.82*) show a significant decline over time.
The rate of change from 2000 to 2019 was calculated using Joinpoint regression software and expressed as Annual Percent Change (APC). *Indicates significant difference at alpha = 0.05 level.
R. Dhital: None; N. Singh: None; B. Pedersen: None; C. Bartels: Pfizer, 5.



