Poster Session A
Reproductive health
Session: (0460–0479) Reproductive Issues in Rheumatic Disorders Poster I
0467: Cardiovascular Events During Pregnancy: Implications for Adverse Pregnancy Outcomes in Individuals with Autoimmune Rheumatic Diseases and Antiphospholipid Syndrome
Sunday, November 12, 2023
9:00 AM - 11:00 AM PT
Location: Poster Hall
- RD
Rashmi Dhital, MD
UC San Diego
San Diego, CA, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Rashmi Dhital, Rebecca Baer and Christina Chambers, University of California San Diego, La Jolla, CA
Background/Purpose: Autoimmune rheumatic diseases (ARD) and antiphospholipid syndrome (APS) are autoimmune conditions with increased risks of cardiovascular complications as well as negative pregnancy consequences. We recently found significantly higher risks for acute cardiovascular events (CVEs) during pregnancy and postpartum in women with ARD and APS compared to individuals without such conditions. However, the impact of such CVEs on adverse pregnancy outcomes (APOs) is not well known. The primary aim was to compare APOs between individuals with ARDs, primary APS and those without either condition, based on the presence or absence of acute CVEs during pregnancy.
Methods: We used the Study of Outcomes in Mothers and Infants (SOMI) database (2005-2020), an administrative population-based birth cohort in California. The main outcomes were APOs, which included preterm birth (PTB) and small-for-gestational age (SGA). Preterm birth was sub grouped as spontaneous, provider initiated, early preterm birth (< 32 weeks), and late preterm birth (32 – 36 weeks). We compared APOs between individuals with or without acute CVEs during pregnancy, after categorizing them into three groups: those with ARDs, those with primary APS, and those with no ARDs or APS. We calculated relative risks (aRR) and 95% confidence intervals (CIs), adjusting for age at delivery, race/ethnicity, primary payer, maternal education, maternal pre-pregnancy body mass index, preexisting hypertension, preexisting diabetes, hyperlipidemia, smoking, alcohol use, drug use, and depression.
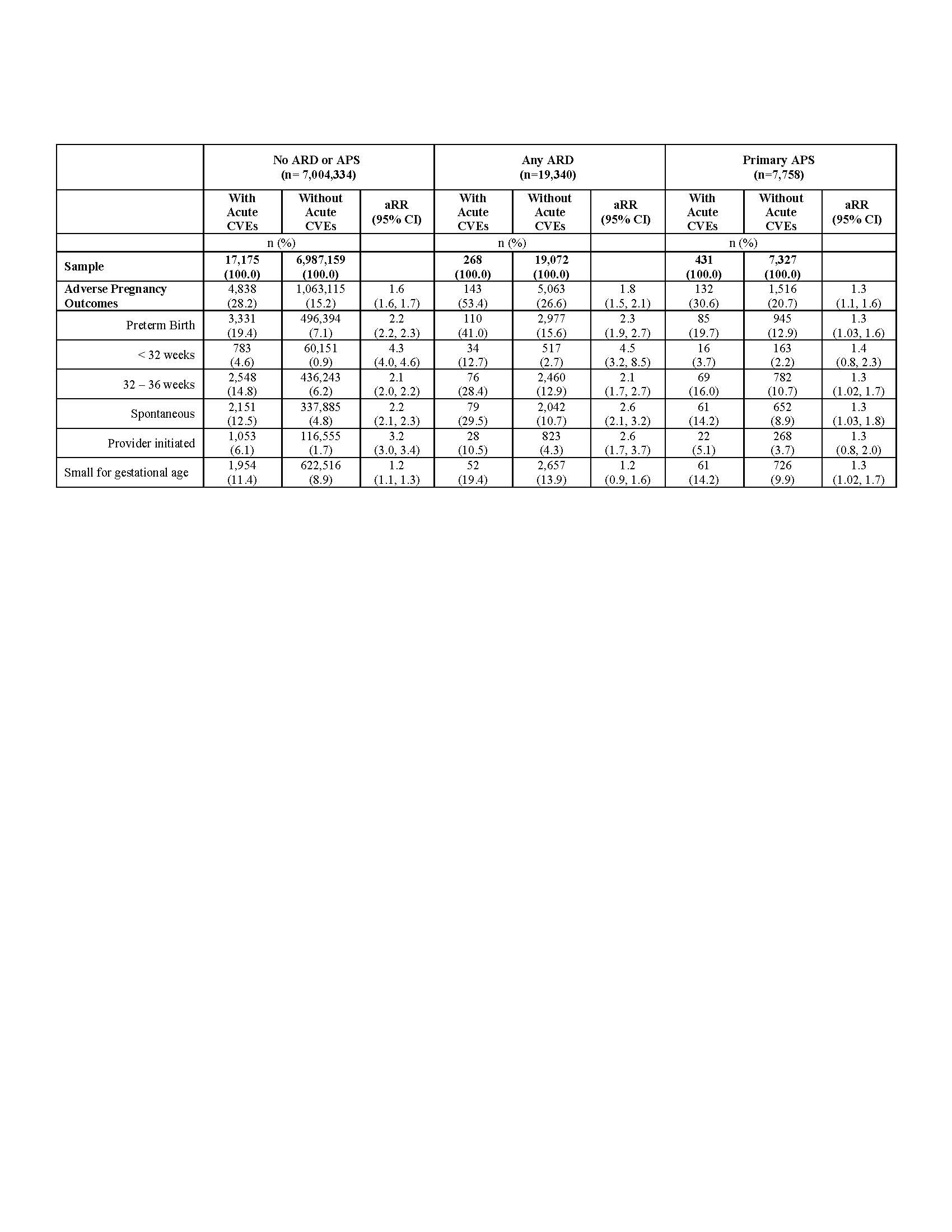
Results: Pregnant individuals with an ARD (26.9%) or primary APS (21.3%) had significantly higher APOs as compared to women without these conditions (15.2%). The presence of acute CVEs during pregnancy further increased the adjusted risk of an APO by 1.8-fold for ARD, 1.3-fold for primary APS and 1.6-fold for those without an ARD or APS. Among individuals with an ARD, more than half (53.4%) with CVEs experienced APOs, compared to 26.6% without CVEs (aRR 1.8, 95% CI 1.5 to 2.1). The increased risk of APOs in ARD pregnancies with CVEs was primarily driven by higher rates of PTB, which was 41.0% in ARD patients with CVEs compared to 15.6% in those without CVEs during pregnancy (RR: 2.3, 95% CI 1,9, 2.7), whereas the rate of SGA was similar among ARD patients with and without CVEs. Among ARD patients with CVEs, 12.7% experienced early PTB, while 2.7% of those without CVEs had early PTB (RR 4.5, 95% CI 3.2 to 8.5) (Table 1).
Conclusion: Pregnant individuals with an ARD or APS had higher rates of APOs than those without these conditions. Acute CVEs during pregnancy further increased the risk of an APO, regardless of ARD or APS diagnosis. These findings highlight the need for close monitoring and management of pregnant women, not only for adverse outcomes, but also for cardiovascular risks and events, in order to identify those at the highest risk for adverse outcomes. This need is particularly significant for individuals with ARDs, as 53.4% of our population with an ARD and CVE in pregnancy experienced an APO.
R. Dhital: None; R. Baer: None; C. Chambers: Amgen, 5, AstraZeneca, 5, Bristol-Myers Squibb(BMS), 5, Genzyme Sanofi-Aventis, 5, Gerber Foundation, 5, Gilead, 5, GlaxoSmithKline, 5, Hoffman La-Roche-Genentech, 5, Janssen Pharmaceuticals, 5, Leo Pharma, 5, Novartis, 5, Pfizer, Inc., 5, Regeneron, 5, Sanofi, 5, Sun Pharma Global FZE, 5, Takeda Pharmaceutical Company Limited, 5, UCB Pharma, USA, 5.
Background/Purpose: Autoimmune rheumatic diseases (ARD) and antiphospholipid syndrome (APS) are autoimmune conditions with increased risks of cardiovascular complications as well as negative pregnancy consequences. We recently found significantly higher risks for acute cardiovascular events (CVEs) during pregnancy and postpartum in women with ARD and APS compared to individuals without such conditions. However, the impact of such CVEs on adverse pregnancy outcomes (APOs) is not well known. The primary aim was to compare APOs between individuals with ARDs, primary APS and those without either condition, based on the presence or absence of acute CVEs during pregnancy.
Methods: We used the Study of Outcomes in Mothers and Infants (SOMI) database (2005-2020), an administrative population-based birth cohort in California. The main outcomes were APOs, which included preterm birth (PTB) and small-for-gestational age (SGA). Preterm birth was sub grouped as spontaneous, provider initiated, early preterm birth (< 32 weeks), and late preterm birth (32 – 36 weeks). We compared APOs between individuals with or without acute CVEs during pregnancy, after categorizing them into three groups: those with ARDs, those with primary APS, and those with no ARDs or APS. We calculated relative risks (aRR) and 95% confidence intervals (CIs), adjusting for age at delivery, race/ethnicity, primary payer, maternal education, maternal pre-pregnancy body mass index, preexisting hypertension, preexisting diabetes, hyperlipidemia, smoking, alcohol use, drug use, and depression.
Results: Pregnant individuals with an ARD (26.9%) or primary APS (21.3%) had significantly higher APOs as compared to women without these conditions (15.2%). The presence of acute CVEs during pregnancy further increased the adjusted risk of an APO by 1.8-fold for ARD, 1.3-fold for primary APS and 1.6-fold for those without an ARD or APS. Among individuals with an ARD, more than half (53.4%) with CVEs experienced APOs, compared to 26.6% without CVEs (aRR 1.8, 95% CI 1.5 to 2.1). The increased risk of APOs in ARD pregnancies with CVEs was primarily driven by higher rates of PTB, which was 41.0% in ARD patients with CVEs compared to 15.6% in those without CVEs during pregnancy (RR: 2.3, 95% CI 1,9, 2.7), whereas the rate of SGA was similar among ARD patients with and without CVEs. Among ARD patients with CVEs, 12.7% experienced early PTB, while 2.7% of those without CVEs had early PTB (RR 4.5, 95% CI 3.2 to 8.5) (Table 1).
Conclusion: Pregnant individuals with an ARD or APS had higher rates of APOs than those without these conditions. Acute CVEs during pregnancy further increased the risk of an APO, regardless of ARD or APS diagnosis. These findings highlight the need for close monitoring and management of pregnant women, not only for adverse outcomes, but also for cardiovascular risks and events, in order to identify those at the highest risk for adverse outcomes. This need is particularly significant for individuals with ARDs, as 53.4% of our population with an ARD and CVE in pregnancy experienced an APO.
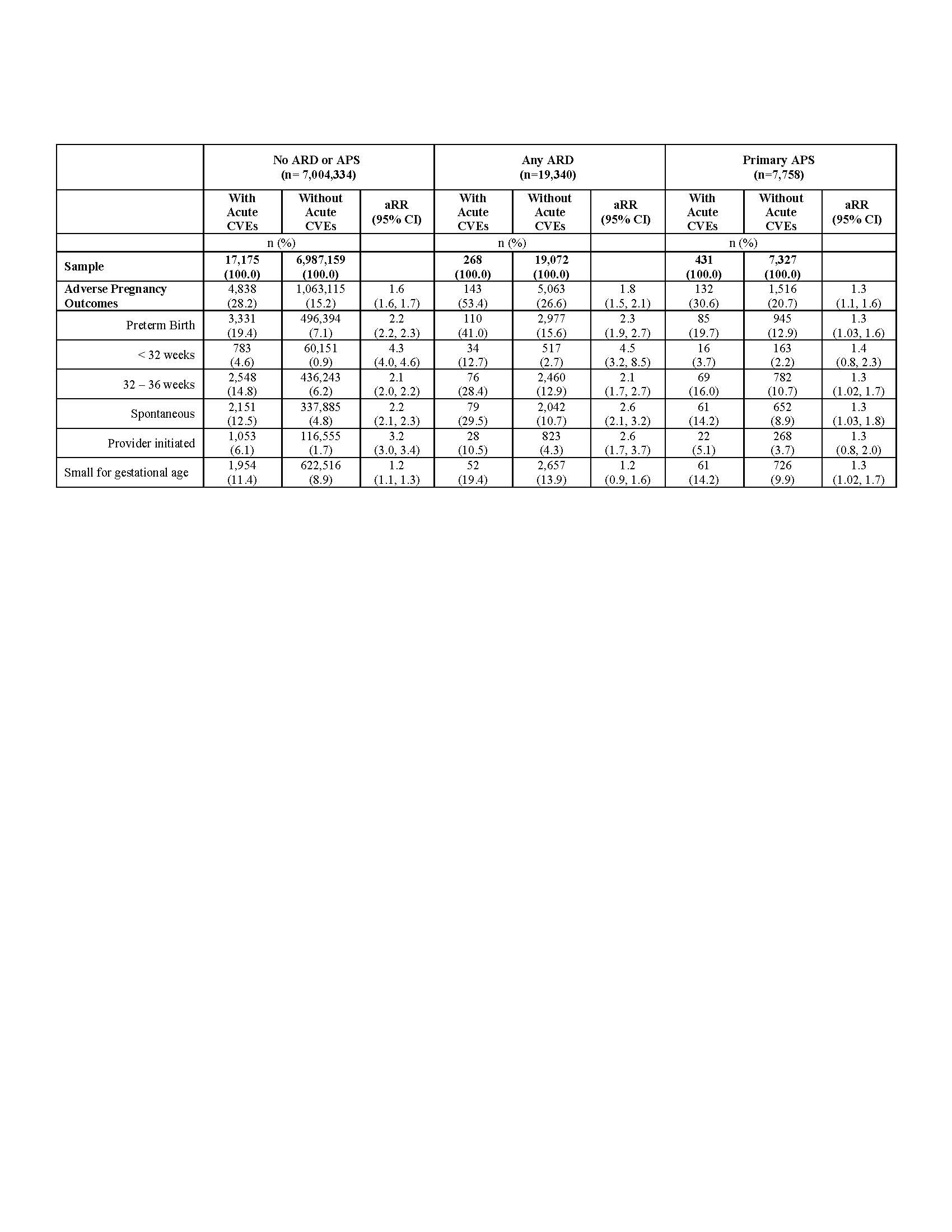
Table 1. Comparison of adverse pregnancy outcomes (APOs) in individuals with or without an acute cardiovascular event during pregnancy, stratified by presence of an autoimmune rheumatic disease (ARD) or primary antiphospholipid syndrome (APS), 2005 – 2020 (n= 7,031,432)
*ARD: autoimmune rheumatic disease, APS: antiphospholipid syndrome, CVEs: cardiovascular events, APOs: adverse pregnancy outcomes
Risks were adjusted for: age at delivery, race/ethnicity, payer for delivery, maternal education, maternal pre-pregnancy body mass index, preexisting hypertension, preexisting diabetes, hyperlipidemia, smoking, alcohol use, drug use, and depression.
*ARD: autoimmune rheumatic disease, APS: antiphospholipid syndrome, CVEs: cardiovascular events, APOs: adverse pregnancy outcomes
Risks were adjusted for: age at delivery, race/ethnicity, payer for delivery, maternal education, maternal pre-pregnancy body mass index, preexisting hypertension, preexisting diabetes, hyperlipidemia, smoking, alcohol use, drug use, and depression.
R. Dhital: None; R. Baer: None; C. Chambers: Amgen, 5, AstraZeneca, 5, Bristol-Myers Squibb(BMS), 5, Genzyme Sanofi-Aventis, 5, Gerber Foundation, 5, Gilead, 5, GlaxoSmithKline, 5, Hoffman La-Roche-Genentech, 5, Janssen Pharmaceuticals, 5, Leo Pharma, 5, Novartis, 5, Pfizer, Inc., 5, Regeneron, 5, Sanofi, 5, Sun Pharma Global FZE, 5, Takeda Pharmaceutical Company Limited, 5, UCB Pharma, USA, 5.



