Abstract Session
Vasculitis
Session: Abstracts: Vasculitis – Non-ANCA-Associated & Related Disorders I: Imaging (1645–1650)
1645: Aortic Dilatation and PET/CT Vascular Activity at Diagnosis and 5 Years in an Inception Giant Cell Arteritis (GCA) Cohort
Monday, November 13, 2023
2:00 PM - 2:10 PM PT
Location: Room 6E/6D
- AS
Anthony Sammel, PhD, MBBS
Prince of Wales Hospital
Sydney, New South Wales, AustraliaDisclosure information not submitted.
Presenting Author(s)
Anthony Sammel1, Ivan Ho Shon2, Daniel Moses1, Fredericks Stacey1, Gita Mathur1, Claudia Hillenbrand3, Edward Hsiao4, Schembri Geoffrey4, Rodger Laurent4 and Eva Wegner2, 1Prince of Wales Hospital, Randwick, Australia, 2The Prince of Wales Hospital, Sydney, Australia, 3University of NSW, Randwick, Australia, 4Royal North Shore Hospital, St. Leonards, Australia
Background/Purpose: Aortic dilatation is typically a late complication of giant cell arteritis (GCA) but there are no tools to risk stratify patients at the time of diagnosis. We assessed the prevalence of aortic dilatation at 5 years in an inception giant cell arteritis cohort and assessed the relationship with FDG-PET/CT detected vascular activity at diagnosis, 6 months and 5 years.
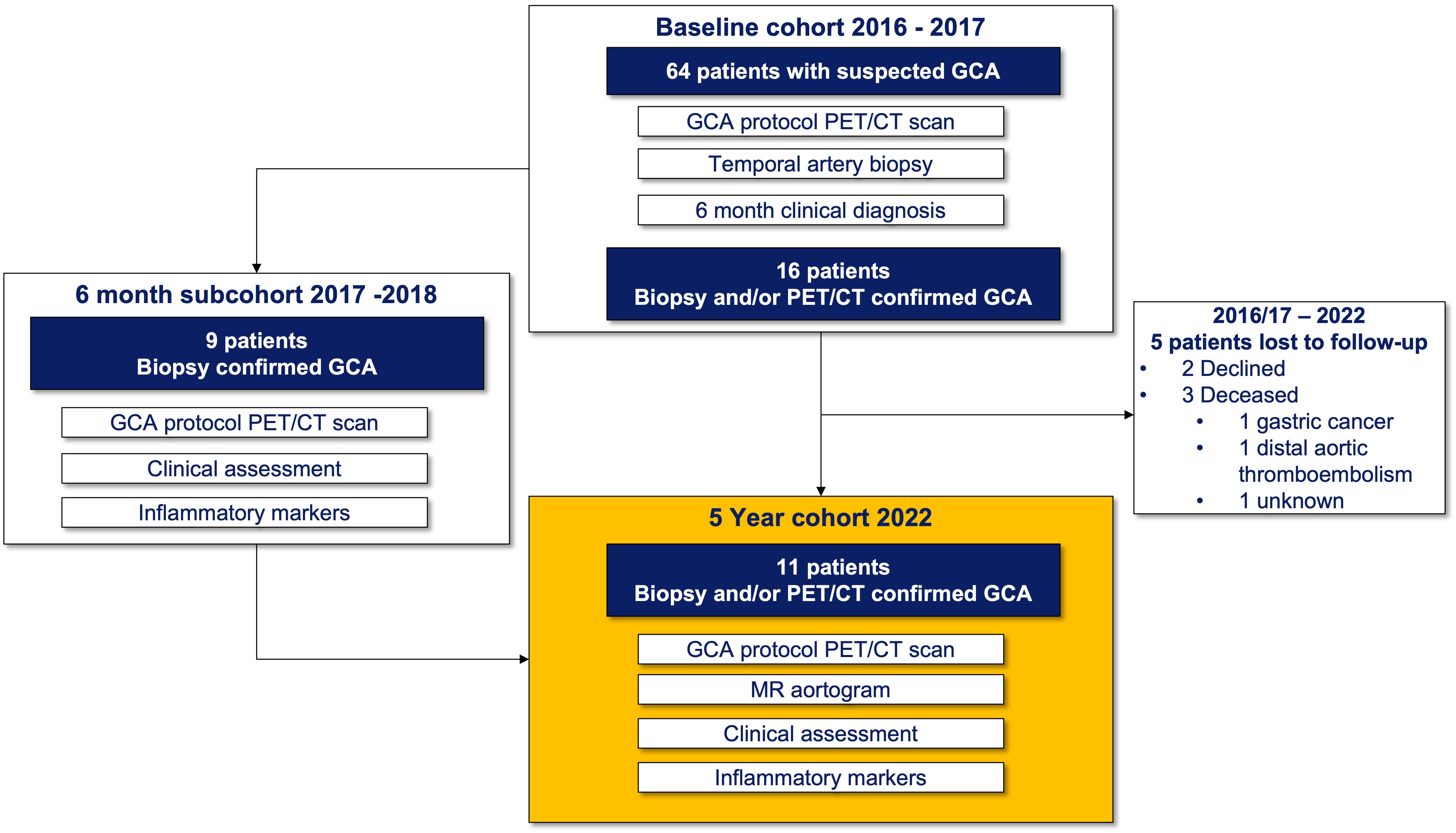
Methods: Patients were eligible for this 5-year study if they had been enrolled in the Giant Cell Arteritis and PET Scan (GAPS) cohort in 2016 or 2017, had a clinical diagnosis of GCA and a positive temporal artery biopsy (TAB) and/or a positive FDG-PET/CT scan at diagnosis. Patients underwent an FDG-PET/CT scan including assessment of cranial and large vessels, non-contrast MRI of the aorta, trans-thoracic echocardiogram (TTE) of the ascending aorta, blood collection and clinical assessment. PET/CT scans were dual reported by 2 blinded nuclear medicine physicians. Scans were reported overall positive or negative for disease activity and a visual grading of FDG avidity in each vascular territory was made with comparison to blood pool. MRI was reported by a single blinded cardiovascular radiologist and thoracic aortic dilatation was defined as external diameter >= 40 mm in ascending or >= 30 mm in the descending aorta.
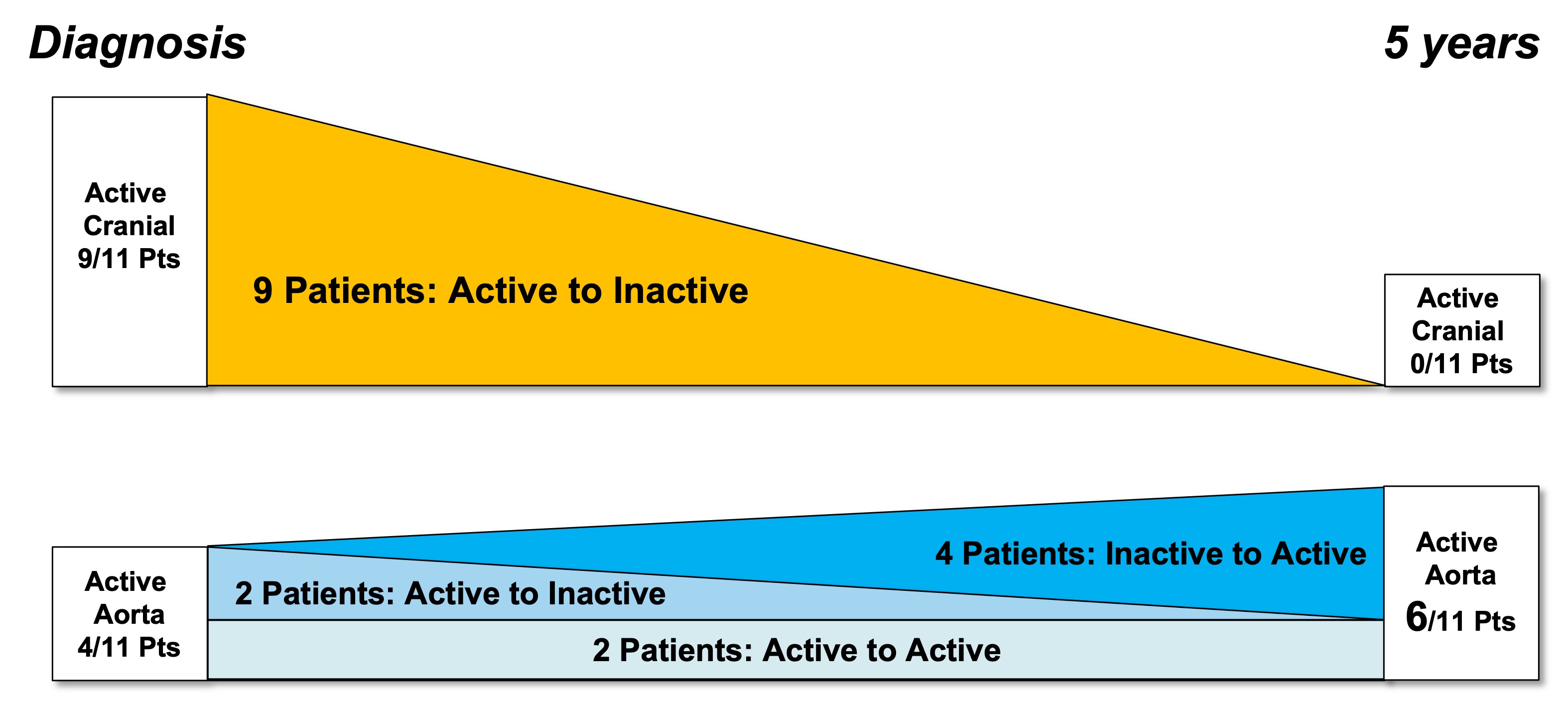
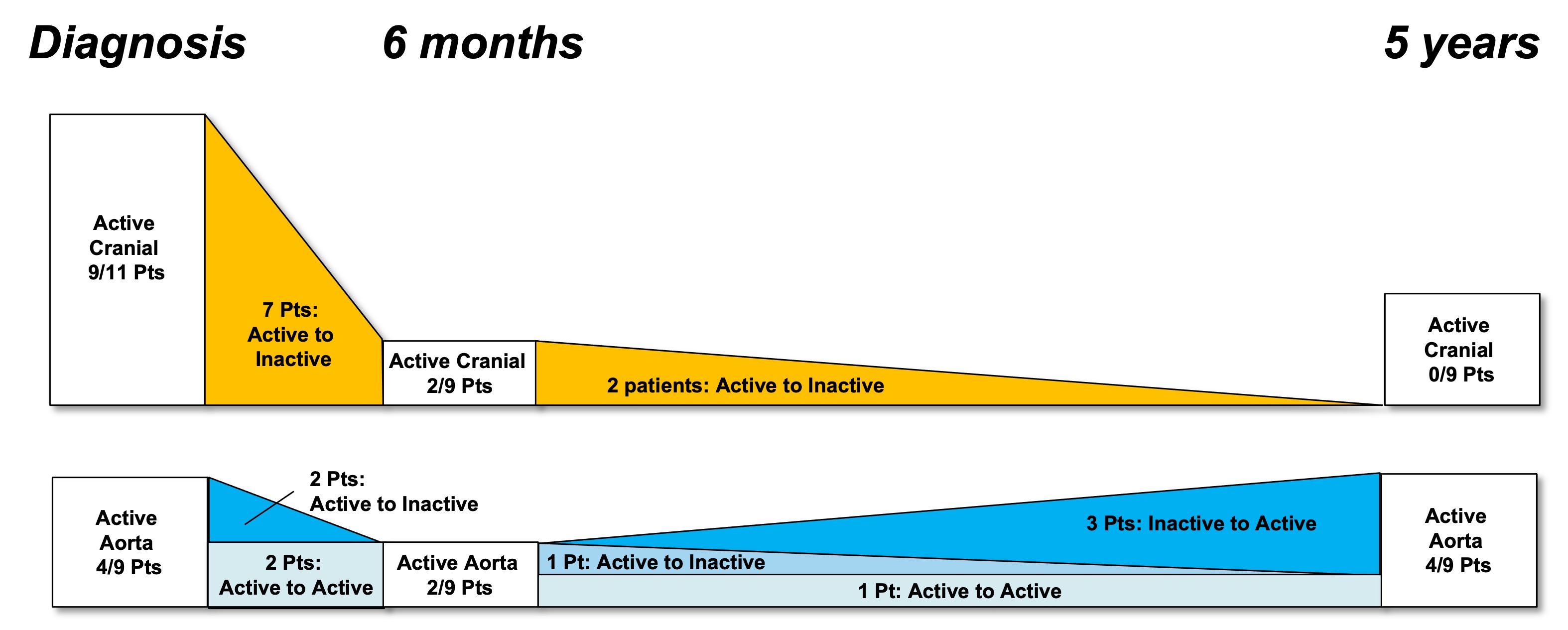
Results: 16 of the original 64 “suspected GCA” patients in the GAPS cohort met inclusion criteria and 11 participated in the 5-year study (3/16 deceased, 2/16 declined). The median age was 75, 73% were female and all were in clinical and serological remission with a median CRP of 1 (range 1 - 8). 4/11 (36%) patients had aortic dilatation (range 40 - 43mm) and 5/11 (45%) had globally active FDG-PET/CT scans. There was a trend towards a higher median aortic diameter in those with positive scans at 5 years (42 mm vs 35 mm, p=0.08) but aortic avidity at diagnosis did not predict 5-year dilatation. The distribution of FDG-PET/CT detected activity changed from a mix of cranial and large vessel disease at diagnosis to exclusively large vessel disease at 5-years. Aortitis developed in 4 patients who previously had inactive aortas. All 6 patients with inactive scans were taking an immunosuppressive agent (methotrexate, leflunomide, azathioprine or tocilizumab) at 5 years while all patients with active scans were not on therapy (p=0.02). TTE had excellent correlation with MRI for maximum aortic diameter (Pearson’s correlation coefficient 0.91).
Conclusion: Aortic dilatation was present in 36% GCA patients at 5 years. The distribution of FDG PET-CT detected avidity changed from predominantly cranial to exclusively large vessel disease and this may explain the lack of association between aortic avidity at diagnosis and dilatation at 5 years. Long-term use of steroid sparing agents may protect against subclinical vascular disease activity. TTE was a reliable screening modality for late aortic dilatation.
A. Sammel: None; I. Ho Shon: None; D. Moses: None; F. Stacey: None; G. Mathur: None; C. Hillenbrand: None; E. Hsiao: None; S. Geoffrey: None; R. Laurent: None; E. Wegner: None.
Background/Purpose: Aortic dilatation is typically a late complication of giant cell arteritis (GCA) but there are no tools to risk stratify patients at the time of diagnosis. We assessed the prevalence of aortic dilatation at 5 years in an inception giant cell arteritis cohort and assessed the relationship with FDG-PET/CT detected vascular activity at diagnosis, 6 months and 5 years.
Methods: Patients were eligible for this 5-year study if they had been enrolled in the Giant Cell Arteritis and PET Scan (GAPS) cohort in 2016 or 2017, had a clinical diagnosis of GCA and a positive temporal artery biopsy (TAB) and/or a positive FDG-PET/CT scan at diagnosis. Patients underwent an FDG-PET/CT scan including assessment of cranial and large vessels, non-contrast MRI of the aorta, trans-thoracic echocardiogram (TTE) of the ascending aorta, blood collection and clinical assessment. PET/CT scans were dual reported by 2 blinded nuclear medicine physicians. Scans were reported overall positive or negative for disease activity and a visual grading of FDG avidity in each vascular territory was made with comparison to blood pool. MRI was reported by a single blinded cardiovascular radiologist and thoracic aortic dilatation was defined as external diameter >= 40 mm in ascending or >= 30 mm in the descending aorta.
Results: 16 of the original 64 “suspected GCA” patients in the GAPS cohort met inclusion criteria and 11 participated in the 5-year study (3/16 deceased, 2/16 declined). The median age was 75, 73% were female and all were in clinical and serological remission with a median CRP of 1 (range 1 - 8). 4/11 (36%) patients had aortic dilatation (range 40 - 43mm) and 5/11 (45%) had globally active FDG-PET/CT scans. There was a trend towards a higher median aortic diameter in those with positive scans at 5 years (42 mm vs 35 mm, p=0.08) but aortic avidity at diagnosis did not predict 5-year dilatation. The distribution of FDG-PET/CT detected activity changed from a mix of cranial and large vessel disease at diagnosis to exclusively large vessel disease at 5-years. Aortitis developed in 4 patients who previously had inactive aortas. All 6 patients with inactive scans were taking an immunosuppressive agent (methotrexate, leflunomide, azathioprine or tocilizumab) at 5 years while all patients with active scans were not on therapy (p=0.02). TTE had excellent correlation with MRI for maximum aortic diameter (Pearson’s correlation coefficient 0.91).
Conclusion: Aortic dilatation was present in 36% GCA patients at 5 years. The distribution of FDG PET-CT detected avidity changed from predominantly cranial to exclusively large vessel disease and this may explain the lack of association between aortic avidity at diagnosis and dilatation at 5 years. Long-term use of steroid sparing agents may protect against subclinical vascular disease activity. TTE was a reliable screening modality for late aortic dilatation.
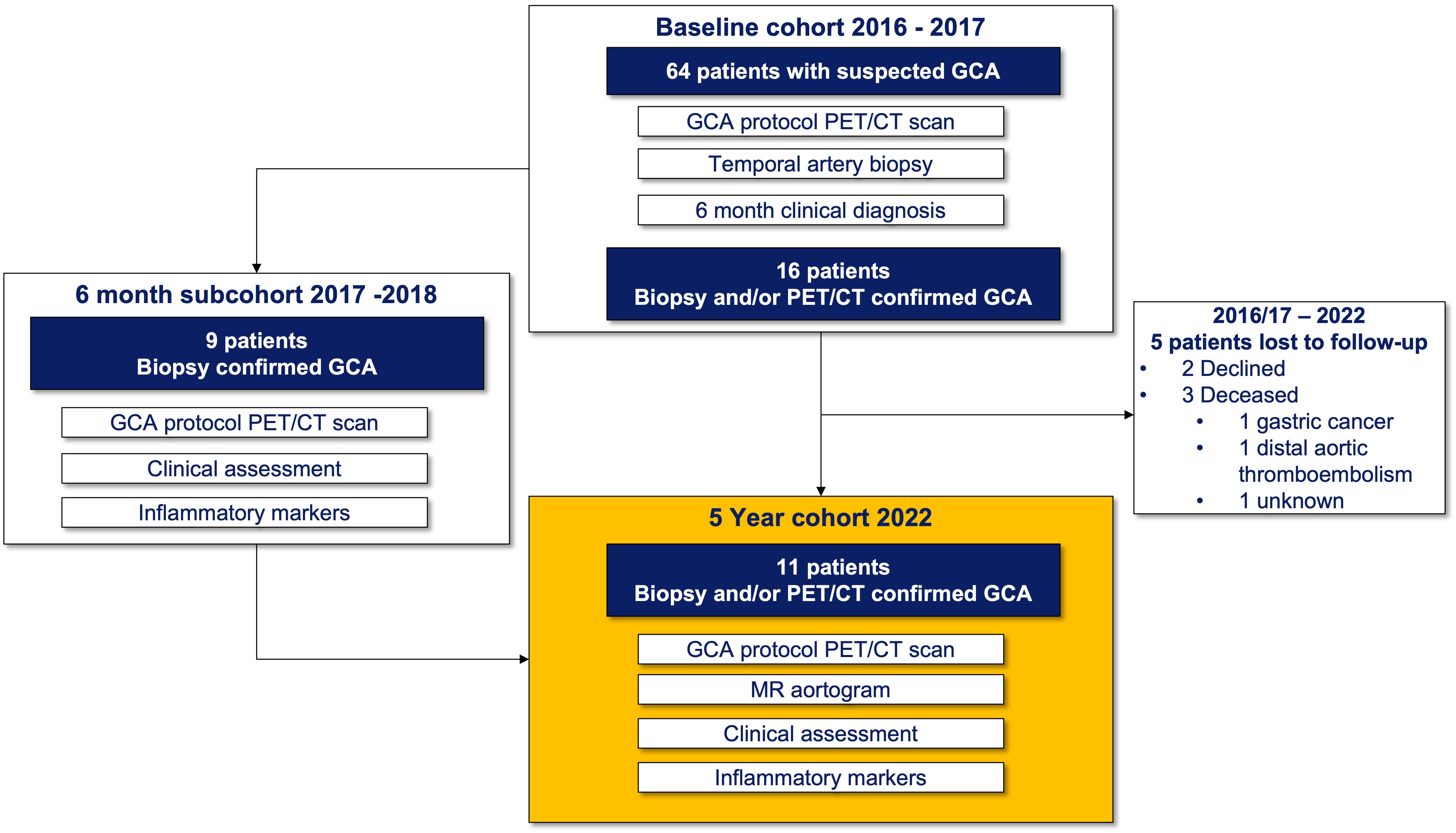
Figure 1: Patient flow
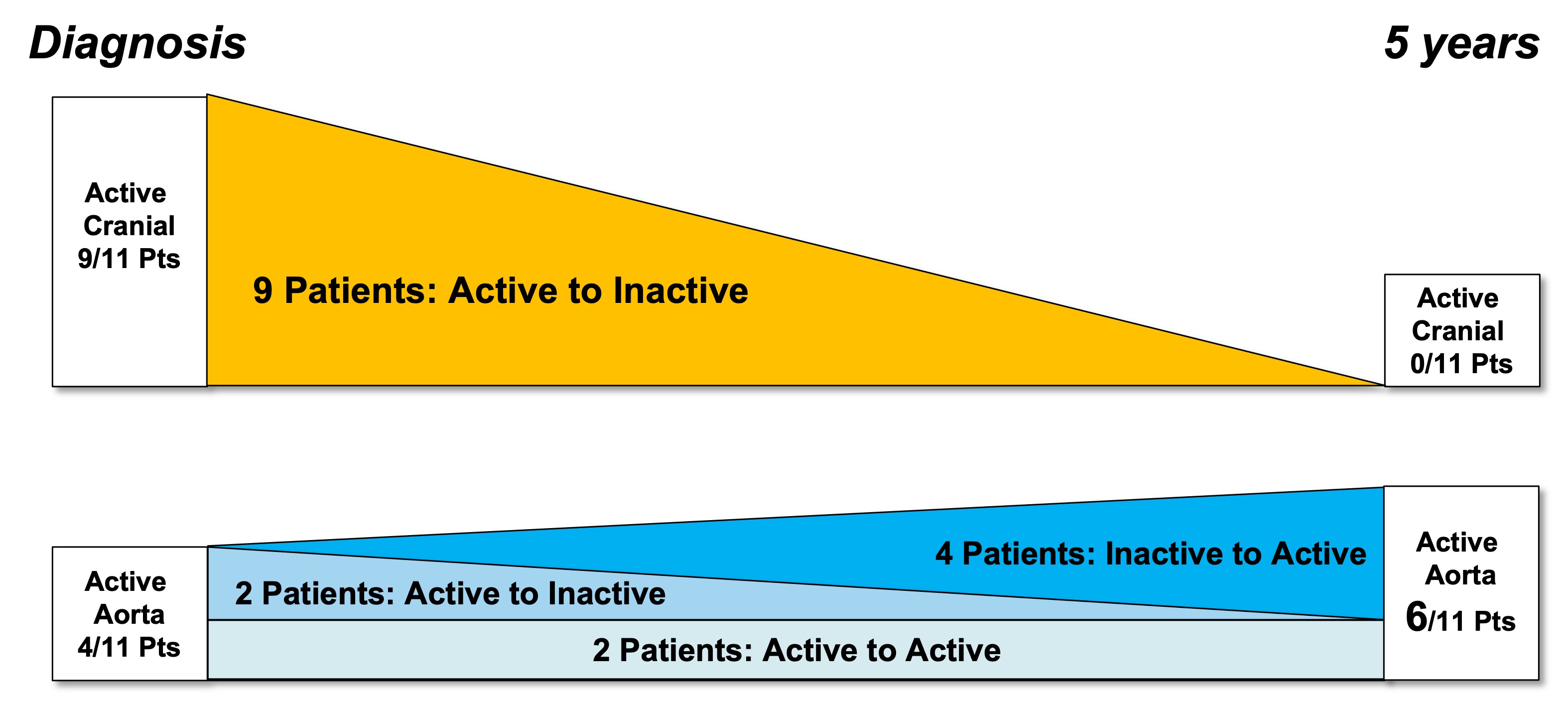
Figure 2: FDG-PET/CT activity by vascular region at diagnosis and 5 years
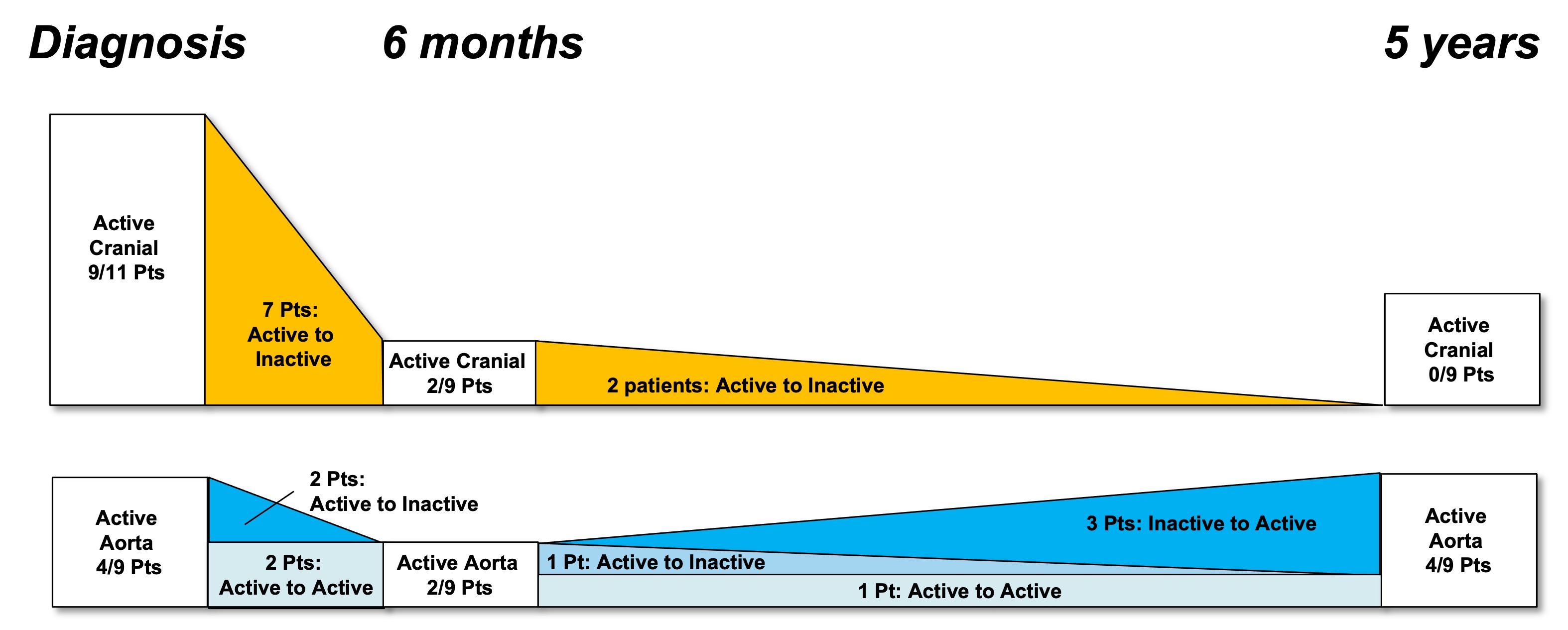
Figure 3: FDG-PET/CT activity by vascular region at diagnosis, 6 months and 5 years (subcohort who underwent 6 month scans)
A. Sammel: None; I. Ho Shon: None; D. Moses: None; F. Stacey: None; G. Mathur: None; C. Hillenbrand: None; E. Hsiao: None; S. Geoffrey: None; R. Laurent: None; E. Wegner: None.



