Abstract Session
Imaging
Session: Abstracts: Imaging of Rheumatic Diseases (0745–0750)
0748: Assessment of Myositis-related Interstitial Lung Disease by ⁶⁸ Ga-DATA.SA.FAPi PET/CT
Sunday, November 12, 2023
2:45 PM - 2:55 PM PT
Location: Room 24A-C
- KK
Presenting Author(s)
Kastriot Kastrati1, Thomas S Nakuz2, Oana C Kulterer2, Stephan Blüml3, Michael Bonelli3, Irina Gessl4, Hans-Peter Kiener3, Werner Langsteger2, Daniel Mrak3, Florian Prayer5, Helmut Prosch5, Elisabeth Simader3, Tatjana Traub-Weidinger2, Daniel Aletaha6, Helga Radner7, Marcus Hacker2 and Peter Mandl3, 1Dept of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna (Austria), Vienna, Austria, 2Division of Nuclear Medicine, Department of Biomedical Imaging and Image-Guided Therapy, Medical University of Vienna, Vienna, Austria, 3Division of Rheumatology, Department of Internal Medicine III, Medical University of Vienna, Vienna, Austria, 4Department of Rheumatology, Medical University of Vienna, Vienna, Austria, 5Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Vienna, Austria, 6Division of Rheumatology, Department of Medicine III, Medical University of Vienna, Vienna, Austria, Wien, Austria, 7Division of Rheumatology, Medical University of Vienna, Vienna, Austria
Background/Purpose: Interstitial lung disease (ILD) is a common manifestation of idiopathic inflammatory myopathies (IIM) ranging up to 78% in IIM and is a key contributor to hospitalization, excess morbidity and mortality. In-vivo visualization evidence of ongoing tissue remodeling in IIM-ILD is scarce. In this study, we aimed to quantify and compare fibroblast activation in the lungs of IIM-patients and control subjects using ⁶⁸Ga-labelled inhibitor of Fibroblast-Activation-Protein based (⁶⁸Ga-DATA.SA.FAPI) positron emission tomography combined with computed tomography (FAPI PET/CT) imaging.
Methods: Patients with IIM recruited prospectively from the rheumatology outpatient clinic, and control subjects without rheumatic conditions or ILD recruited from the cardiology outpatient clinic underwent FAPI PET-CT imaging. Pulmonary FAPI accumulation was assessed by measuring the maximal standardized uptake (SUV) value (SUVmax) and mean SUV (SUVmean) over the whole lung (wl) using the liver as internal reference, respectively. Values of SUV were compared across IIM patients with and without ILD and controls using analysis of variance test and displayed as mean ± standard deviation (SD). Standard-of-care procedures such as high-resolution computed tomography (hr-CT) and pulmonary function testing (PFT) were performed in all IIM-patients at baseline and in patients with ILD at follow-up.
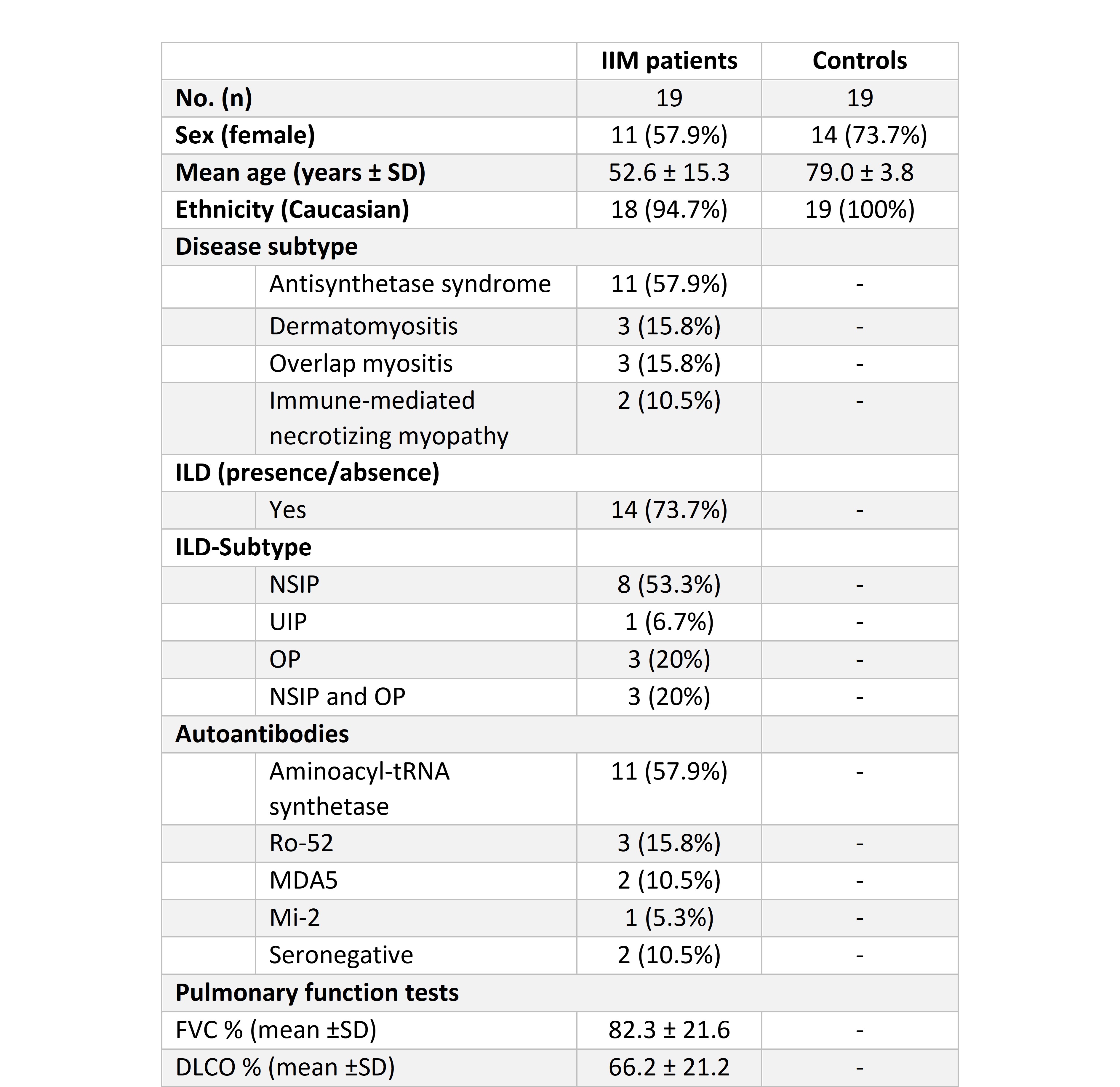
Results: The clinical characteristics of patients with IIM (14 patients with ILD confirmed by hr-CT and 5 non-ILD patients with primary muscular affection) and control subjects (n=19) are displayed in Table 1. Three (n=3) patients in the control group were excluded from analysis due to pulmonary disease or cardiac decompensation. In individuals with IIM-related ILD, whole-lung ⁶⁸Ga-DATA.SA.FAPI uptake assessed by wlSUVmax (Figure 1A) and wlSUVmean (Figure 1B) corrected for the liver was significantly increased as compared to both non-ILD IIM patients and the control group. No differences of wlSUVmax or wlSUVmean were observed between non-ILD IIM patients and the control group. FAPI uptake in the lungs correlated significantly with pulmonary function tests, severity of dyspnea and serum concentration of acute phase reactants at baseline. Moreover, IIM-patients with progressive ILD (defined as worsening in pulmonary function tests at 1-year follow up and/or need for intensification of immunosuppressive therapy) had significantly increased pulmonary FAPI uptake at baseline (Figure 2).
Conclusion: Our study demonstrates higher FAPI uptake in patients with IIM-ILD. Intensity of pulmonary FAPI accumulation was associated with progression of ILD. Thus, ⁶⁸ Ga-DATA.SA.FAPi PET/CT may serve as a useful non-invasive tool for risk stratification of lung disease in IIM.
.jpg)
.jpg)
K. Kastrati: None; T. Nakuz: None; O. Kulterer: None; S. Blüml: None; M. Bonelli: Eli Lilly, 12, personal fees, Galapagos, 5, GlaxoSmithKlein(GSK), 5; I. Gessl: None; H. Kiener: None; W. Langsteger: None; D. Mrak: None; F. Prayer: None; H. Prosch: AstraZeneca, 5, 6, Boehringer-Ingelheim, 1, 5, 6, 12, Travel grants, Bristol-Myers Squibb(BMS), 1, 6, EU Commission (EU4Health, Horizon Europe Health), 5, Janssen, 6, Merck/MSD, 1, 6, Novartis, 6, Roche, 1, 6, Sanofi, 1, 6, Siemens Healthcare, 5, 6, Takeda, 6; E. Simader: None; T. Traub-Weidinger: None; D. Aletaha: AbbVie, 2, 5, 6, Amgen, 2, 5, 6, Janssen, 2, 6, Lilly, 2, 5, 6, Merck, 2, 6, Novartis, 2, 5, 6, Pfizer, 2, 6, Roche, 2, 5, 6, Sandoz, 2, 6, Sanofi, 5, Sobi, 5; H. Radner: None; M. Hacker: None; P. Mandl: AbbVie/Abbott, 5, 6, Bristol-Myers Squibb(BMS), 5, 6, Celgene, 5, 6, Eli Lilly, 5, 6, Janssen, 5, 6, Merck/MSD, 5, 6, Novartis, 5, 6, Roche, 5, 6, UCB, 5, 6.
Background/Purpose: Interstitial lung disease (ILD) is a common manifestation of idiopathic inflammatory myopathies (IIM) ranging up to 78% in IIM and is a key contributor to hospitalization, excess morbidity and mortality. In-vivo visualization evidence of ongoing tissue remodeling in IIM-ILD is scarce. In this study, we aimed to quantify and compare fibroblast activation in the lungs of IIM-patients and control subjects using ⁶⁸Ga-labelled inhibitor of Fibroblast-Activation-Protein based (⁶⁸Ga-DATA.SA.FAPI) positron emission tomography combined with computed tomography (FAPI PET/CT) imaging.
Methods: Patients with IIM recruited prospectively from the rheumatology outpatient clinic, and control subjects without rheumatic conditions or ILD recruited from the cardiology outpatient clinic underwent FAPI PET-CT imaging. Pulmonary FAPI accumulation was assessed by measuring the maximal standardized uptake (SUV) value (SUVmax) and mean SUV (SUVmean) over the whole lung (wl) using the liver as internal reference, respectively. Values of SUV were compared across IIM patients with and without ILD and controls using analysis of variance test and displayed as mean ± standard deviation (SD). Standard-of-care procedures such as high-resolution computed tomography (hr-CT) and pulmonary function testing (PFT) were performed in all IIM-patients at baseline and in patients with ILD at follow-up.
Results: The clinical characteristics of patients with IIM (14 patients with ILD confirmed by hr-CT and 5 non-ILD patients with primary muscular affection) and control subjects (n=19) are displayed in Table 1. Three (n=3) patients in the control group were excluded from analysis due to pulmonary disease or cardiac decompensation. In individuals with IIM-related ILD, whole-lung ⁶⁸Ga-DATA.SA.FAPI uptake assessed by wlSUVmax (Figure 1A) and wlSUVmean (Figure 1B) corrected for the liver was significantly increased as compared to both non-ILD IIM patients and the control group. No differences of wlSUVmax or wlSUVmean were observed between non-ILD IIM patients and the control group. FAPI uptake in the lungs correlated significantly with pulmonary function tests, severity of dyspnea and serum concentration of acute phase reactants at baseline. Moreover, IIM-patients with progressive ILD (defined as worsening in pulmonary function tests at 1-year follow up and/or need for intensification of immunosuppressive therapy) had significantly increased pulmonary FAPI uptake at baseline (Figure 2).
Conclusion: Our study demonstrates higher FAPI uptake in patients with IIM-ILD. Intensity of pulmonary FAPI accumulation was associated with progression of ILD. Thus, ⁶⁸ Ga-DATA.SA.FAPi PET/CT may serve as a useful non-invasive tool for risk stratification of lung disease in IIM.
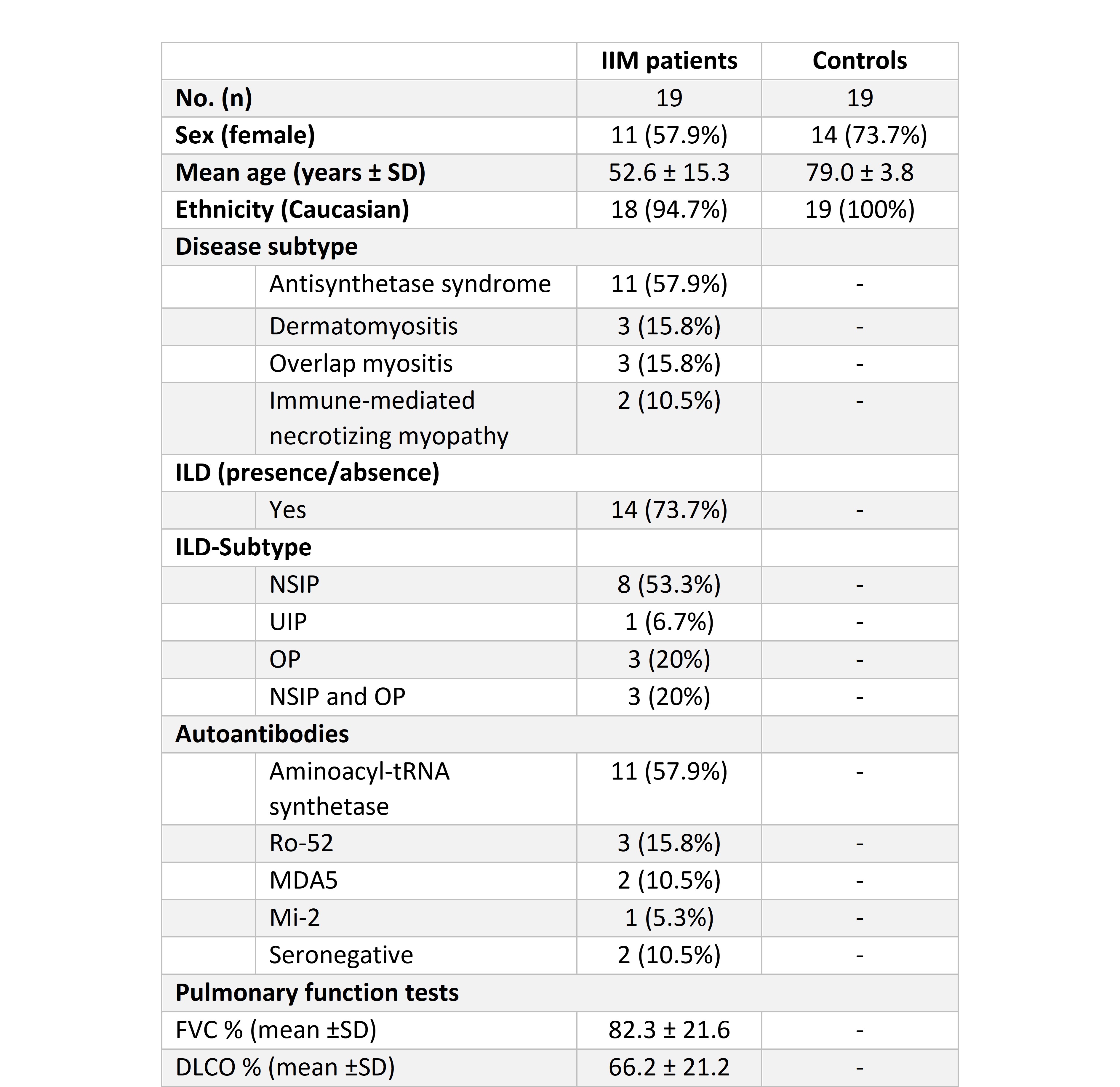
Table 1: Demographic and clinical characteristics of participants at baseline. Abbreviations: DLCO, diffusion capacity of the lungs for carbon monoxide; FVC, forced vital capacity; IIM: idiopathic inflammatory myopathy; ILD: interstitial lung disease; No./n, number; NSIP, nonspecific interstitial pneumonia; OP, organizing pneumonia; SD, standard deviation; UIP, usual interstitial pneumonia
.jpg)
Figure 1: ⁶⁸Ga-FAPI uptake in the lungs of IIM-patients and controls. A) Whole-lung maximal standardized uptake value; B) whole-lung mean standardized uptake value in myositis patients with or without interstitial lung disease and control subjects. Abbreviations: wlSUVmax (liver), whole-lung maximal standardized uptake value in relation to liver; wlSUVmean (liver), whole-lung mean standardized uptake value in relation to liver; ILD, interstitial lung disease, ns, not significant.
.jpg)
Figure 2: Baseline pulmonary ⁶⁸Ga-FAPI accumulation and ILD progression. Boxplot demonstrating FAPI uptake determined by whole-lung mean standardized uptake value (wlSUVmean) in relation to liver. IIM-patients with progressive ILD (Progressors) were defined as worsening in pulmonary function tests at 1-year follow up and/or need for intensification of immunosuppressive therapy. Non-progressors were defined as patients with myositis-related ILD with forced vital capacity reduction of less than 5%, diffusion capacity of carbon monoxide reduction of less than 10%, and stable respiratory symptoms. Abbreviations: wlSUVmean (liver), whole-lung mean standardized uptake value in relation to liver.
K. Kastrati: None; T. Nakuz: None; O. Kulterer: None; S. Blüml: None; M. Bonelli: Eli Lilly, 12, personal fees, Galapagos, 5, GlaxoSmithKlein(GSK), 5; I. Gessl: None; H. Kiener: None; W. Langsteger: None; D. Mrak: None; F. Prayer: None; H. Prosch: AstraZeneca, 5, 6, Boehringer-Ingelheim, 1, 5, 6, 12, Travel grants, Bristol-Myers Squibb(BMS), 1, 6, EU Commission (EU4Health, Horizon Europe Health), 5, Janssen, 6, Merck/MSD, 1, 6, Novartis, 6, Roche, 1, 6, Sanofi, 1, 6, Siemens Healthcare, 5, 6, Takeda, 6; E. Simader: None; T. Traub-Weidinger: None; D. Aletaha: AbbVie, 2, 5, 6, Amgen, 2, 5, 6, Janssen, 2, 6, Lilly, 2, 5, 6, Merck, 2, 6, Novartis, 2, 5, 6, Pfizer, 2, 6, Roche, 2, 5, 6, Sandoz, 2, 6, Sanofi, 5, Sobi, 5; H. Radner: None; M. Hacker: None; P. Mandl: AbbVie/Abbott, 5, 6, Bristol-Myers Squibb(BMS), 5, 6, Celgene, 5, 6, Eli Lilly, 5, 6, Janssen, 5, 6, Merck/MSD, 5, 6, Novartis, 5, 6, Roche, 5, 6, UCB, 5, 6.



